Microangiopathy of the brain is a lesion of the smallest vessels, capillaries localized in cerebral structures. Pathological changes in the walls, narrowing or complete blockage of blood vessels occur.
The disease does not manifest itself as long as the body is able to cope with disturbances in trophism and nutrition of nerve tissue.
In some cases, the approaching catastrophe is not noticeable, which is why the clinical picture is extremely variable. Depends on the individual characteristics of the body and the localization of the process.
As a rule, the pathology affects all capillaries of the brain at once, but not equally. When assessing a person’s condition, individual, largest lesions are detected. This facilitates targeted therapy if surgical treatment is required.
Correction is mainly medicinal. If ineffective, surgery is prescribed.
Development mechanism
There are several provoking factors underlying this. They occur together or separately. It's more a matter of chance. In total there are 4 main ways:
- Consistently high blood pressure levels. A change in the nature of blood flow through the main vessels leads to stenosis (narrowing) of the arteries, a decrease in their elasticity and a reflex violation of capillary tone.
In addition, negative factors that provoke an increase in blood pressure (usually hormonal or toxic, from smoking, drinking alcohol) can also affect small vessels in the same way.
Then the process becomes complex. The entire brain is affected. Such a number of negative factors brings stroke closer every day.
- Inability to regulate vascular tone, changes in their physical properties due to hormonal instability. A textbook example of such a disorder is diabetes mellitus.
If treatment is not carried out, the body simply cannot provide homeostasis (a state of equilibrium). Hence the change in the tone of the capillaries, also arteries, veins.
Severe complications arise over a short period of time. Patients walk along the edge constantly.
- Improper functioning of the immune system. As a result, active synthesis of antigen-antibody complexes develops, followed by the formation of a special protein conglomerate—amyloid.
This substance settles on the walls of blood vessels and provokes degenerative changes over a short period of time. A similar mechanism applies to autoimmune ones. It is considered difficult to correct and dangerous because the prospects are vague.
- It is also possible for mineral salts to be deposited on the walls of the capillaries. Mainly calcium. This is a relatively common mechanism and occurs in children under one year of age. It is diagnosed during the same period.
In the initial stages, symptoms are not noticeable, but as they progress, health deteriorates.
Objectively, the clinical picture is presented by manifestations of nonspecific neurological deficit. Headaches, nausea, spatial disorientation and others are observed that cannot be linked to a specific disease.
Attention:
If you don't take control of the situation, the consequences are dire. Further development of deficiency, stroke, disability or death.
The timing of the negative scenario from beginning to end is different. In most patients, as a result of compensation of the body and adaptation of impaired blood flow, collaterals are formed. That is, parallel, additional networks of capillaries that were not there initially.
If they are sufficiently formed, the violations will not be so noticeable and the “X-hour” will come later. No one can say how much.
Classification
The main method of division is based on the types of pathological process and its origin.
Hypertensive form
As the name suggests, it develops mainly in patients with the same diagnosis. But not always. A symptomatic increase in blood pressure against the background of other diseases gives the same effect.
The longer the violation exists, the higher the tonometer numbers, the more significant the risks.
A latent pathological process is present in most patients, but not the entire array of situations is diagnosed, because doctors are busy assessing the condition of the arteries, and the capillaries are ignored, which is wrong.
Cerebral microangiopathy amyloid type
Associated with the accumulation of this protein substance in the structures of capillaries. Leads to a fairly rapid development of neurological deficit.
It occurs mainly in patients over 60, which is associated with lifestyle and past illnesses. But the deviation does not have gender and age characteristics.
The pathology is autoimmune and requires correction of the functional activity of the body's defenses.
Lenticulostriate type
It is associated with the deposition of calcium salts on the walls of blood vessels, which does not occur normally. The process progresses extremely slowly, which is why symptoms appear late.
The disease is diagnosed mainly in children. According to research, the disorder occurs in every sixth birth. In Russia - the fourth.
This condition is not always considered a disease. There is an opinion that we are talking about a variant of the physiological norm.
If there are no symptoms and the nature of the trophism of nerve tissue is not changed, this is a feature of the body, not a pathology.
Diabetic form
One of the most common. Occurs as a complication of the named endocrine disorder. Diabetic angiopathy is severe and provokes critical disturbances in cerebral blood flow, since the arteries are also affected.
If the correct course of treatment is chosen, the condition is partially controlled, the likelihood of negative consequences is not so high. A complete correction is also possible.
But the effectiveness of the measures and the final result depend on the patient himself, his willingness to follow the specialist’s recommendations and discipline.
There are also classifications according to the course of the pathological process. Thus, angiopathy can be with or without the presence of foci of gliosis (scars, scars). The first option is one and a half to two times less common.
It is possible to subdivide the pathology according to the volume of the lesion. The extensive type is accompanied by the formation of many areas of impaired vascular function.
Attention:
Single lesions give mild symptoms and are much better treated. Because localization is clear, and you can clearly monitor the dynamics of the process.
Typifications are used to describe pathology in documentation and develop treatment methods.
Symptoms
The clinical picture at the initial and even advanced stages is blurry. Because microangiopathy does not always lead to severe blood flow disturbances. This takes time.
The body also compensates for the disorder by increasing the amount of nutrition due to the formation of new capillary networks. The so-called collaterals.
They cannot replace functional structures completely, but they are enough.
You also need to take into account the number of lesions, their size, and the type of microangiopathy itself. Individual characteristics of the body. Such an array of factors makes bringing the clinic to a common denominator a difficult task.
The following symptoms occur, with varying intensity and severity and at different times:
- Headache. The strength of discomfort varies. By nature it is pressing, shooting, burning. Located in the frontal and temporal lobes. A different location is possible. The intensity increases after physical activity, stress, and smoking. Consumption of coffee, alcohol, changes in climate zone and when exposed to other negative factors.
The pain is paroxysmal. They go away on their own within a few minutes or hours. The drugs help eliminate discomfort faster.
- Dizziness. Inability to properly navigate in space. Usually low intensity.
- Due to insufficient blood flow, the patient becomes more sensitive to aggressive environmental factors. Changes in weather, vegetative-vascular crises, surges in blood pressure against the background of a new temperature regime, for example, when moving to another region or climate zone. Women have a much more difficult time with premenstrual syndrome, etc.
- Nausea. Rarely vomiting. Single episodes and not always.
- There is also an inability to control one’s own body normally. Weakness in the limbs, clumsiness, unsteadiness of gait, muscle discomfort, feeling of leaden heaviness. All these are parts of one whole.
- Asthenic phenomena. A person constantly feels tired. Weakness, fatigue, drowsiness, regardless of the time of day. All these are signs of insufficient trophism of cerebral tissues. The brain goes into an “economy” mode and does not spend energy as actively.
- Behavioral disorders. Aggressiveness, tearfulness, irritability for no apparent reason.
- Problems with thinking and cognitive sphere. Decreased speed and productivity, absent-mindedness, forgetfulness, attention deficit, inability to concentrate on a subject.
- Focal neurological signs. Disorders of the sensory organs and higher nervous activity. In severe cases, speech disorders are observed, the patient cannot perform arithmetic operations, write, read, etc.
This is not as pronounced as with a stroke, but attracts enough attention. Such signs are possible only with brain damage. What kind of plan - vascular, tumor, toxic or other - needs to be quickly clarified.
In rare cases, fainting and syncope are possible. They indicate a progressive disturbance of cerebral blood flow and indicate the severity of the process. A stroke is likely in the near future.
Symptoms are an unreliable diagnostic criterion. However, they must be taken into account.
Causes
Development factors are different. Among the possible:
- Past severe infectious processes. Especially affecting the brain. It is this disorder that often becomes a trigger, a trigger for amyloidosis. The immune system begins to react inadequately to imaginary stimuli.
- Cardiovascular pathologies. Already named hypertension or symptomatic increase in blood pressure.
- Diabetes. The real scourge of patients with this diagnosis is problems with vessels of various sizes throughout the body. In addition, it may be influenced by other hormonal diseases. Like pathologies of the thyroid gland, adrenal glands.
- Smoking, alcoholism. Bad habits.
- Also excessive physical activity.
- Genetic disorders.
- Malfunctions of the immune system. Against the background of other disorders or as a primary deviation, which rarely happens.
Microangiopathy of cerebral vessels can be polyetiological, that is, due to a group of reasons. All of them are taken into account to determine the path of fundamental treatment.
Affective disorders associated with CMA
According to the vascular depression hypothesis, cerebral small vessel disease may cause or worsen depression in older adults. Hypothetically, affective symptoms arise from changes in frontal and limbic brain structures or their pathways involved in mood regulation [6]. A 2014 meta-analysis that included 19 studies and 6,274 participants found a strong association between the degree of white matter damage, an indirect sign of small vessel disease in the brain, and depression. This was later confirmed by a more extensive meta-analysis [7]. Multiple markers of microvascular dysfunction, including markers of endothelial dysfunction and markers of cerebral small vessel disease, are also strongly associated with the severity of depressive disorder. Important arguments in favor of the connection between depression and CMA are the following facts:
symptoms of depression first appear at a late age (after 55–60 years);
there is no history of depressive episodes;
no family history of depression;
The course of depression is characterized by a high relapse rate and resistance to antidepressants.
The connection between the debut of affective symptoms and the onset of vascular aging was pointed out back in the 1990s by GS Alexopoulos, the author of the concept of vascular depression.
There are no diagnostic criteria for depressive disorder that are specific to older adults. However, based on practical observations supported by research, the clinical signs of depression in people with CMA may differ from those observed in early and middle age. It is now generally accepted that the clinical picture of depression associated with CMA has its own distinctive features, which are important for the clinician to know for early diagnosis of this condition:
older patients complain of sadness and a sad mood much less often than younger patients;
with active questioning, asthenia and decreased motivation can be identified;
psychomotor functions slow down, lack of initiative and apathy appear;
hypochondriacal and somatic complaints prevail (persistent unexplained pain, dizziness, tinnitus, intestinal spasms, constipation, etc.);
anxiety often dominates the onset of the clinical picture and overlaps the symptoms of depression;
pathological personality traits worsen;
dyssomnia is usually regarded as the leading complaint;
the speed of information processing decreases;
memory is assessed subjectively low;
functional activity decreases disproportionately with the objective severity of the condition.
For some older adults with depression, sad mood is not the main symptom. They may have other, less obvious symptoms of depression—tearfulness, feelings of hopelessness, worthlessness, or helplessness—that they are often reluctant to talk about. Elderly people who are depressed complain of fatigue, poor sleep, and are grumpy and irritable. Since insomnia naturally occurs more often in old age, it may escape the attention of the doctor, who readily considers this disorder as a symptom of age. Sleep disturbance can manifest itself in different ways: some people have fragmented sleep, with early awakenings, while others, on the contrary, develop hypersomnia. People around them often notice that a person stops being engaged and interested in things that were once enjoyable for him. Such patients exhibit characteristic signs: confusion in a situation that requires a quick reaction, difficulty maintaining attention and making decisions - all this indicates a lack of cognitive functions. Patients themselves and their relatives often perceive these depressive symptoms as a violation of cognitive functions (primarily memory). An observant doctor may note motor retardation and/or slow speech. Finally, depression can affect your appetite and lead to weight gain or loss.
Unlike mental symptoms of depression, somatic symptoms, such as vague and difficult to localize pain, headache, dizziness, tinnitus, indigestion, constipation, become the main reason for visiting a doctor. And patients and their doctors often attribute pain, gastrointestinal distress, fatigue, loss of appetite and sleep disturbances to underlying medical conditions. This leads to unnecessary examinations. The desire to hide complaints in case of cognitive impairment, difficulties in expressing emotions, and the tendency to somatize them significantly complicate the diagnosis of depression [8].
To assess affective disorders in CMA, it is important for the clinician to correctly construct a conversation with the patient. The mental manifestations of depression should not be asked directly, but judged through reactions to external events. Patients are willing to discuss physical symptoms, such as fatigue.
It is typical that the patient experiences fatigue not after physical or mental stress, but constantly and, due to fatigue, does not try to perform even minimal physical work. It is important to find out how much this or that somatic symptom affects the patient’s activity and mood. A properly structured survey and objective examination can reveal the discrepancy between extremely low physical and mental activity and objective health status.
Additional risk factors.
Older age, coupled with more life experience, can be an advantage in dealing with stressors. But, on the other hand, with age, losses increase, and inevitable gaps in social communication occur. Research shows that the highest risk of developing depression is associated with the loss of a significant person (usually a spouse). The next most stressful factor is chronic disease [9]. For example, antihypertensive and corticosteroid drugs that affect the regulation of catecholamine metabolism can cause depression. An increase in the number of physical illnesses and, accordingly, increased use of medications in old age increases the risk of depression.
The 2021 pandemic has been a unique stressor affecting the entire global community. COVID-19 has had a particularly strong impact on the lives of older people with mood disorders. Older people are more affected by the adverse effects of the pandemic: exposure to more serious complications, higher mortality, increased anxiety due to changes in daily routines and limited access to health care, due to the need to turn to technologies such as telemedicine, and finally, for fears that existing diseases will worsen in isolation. This makes older people feel even more lonely and disconnected from life. Additionally, many older adults do not have the necessary resources to cope with the stress associated with COVID-19. They are limited in their ability to engage in physical exercise or intellectual work. Past epidemics have shown that long-term stressors can increase anxiety and depressive symptoms. For example, during the SARS outbreak in 2003, suicide rates among older adults increased dramatically [10]. In addition, previous studies have shown that social isolation increases the risk of cardiovascular, autoimmune, and neurodegenerative diseases [11]. According to early research, more than a third (37.1%) of older people experienced depression and anxiety during the pandemic [12], and emotional reactions in people over 60 years of age were more evident than in other age groups [13].
Diagnostics
The examination is the task of neurologists. If necessary, a specialist in vascular surgery is involved.
The list of activities is always identical, with minor deviations:
- Oral questioning of the patient. It is necessary to identify complaints and make a list of symptoms. This will allow you to determine the direction of further diagnostics.
- Anamnesis collection. In particular: infectious processes suffered in the recent past, current and chronic pathologies, family history of diseases, bad habits.
- General and biochemical blood tests.
- Electroencephalography. To determine the functional activity of cerebral structures.
- MRI or CT scan of the brain. It is possible to conduct two studies at once. Used to identify the location, number of lesions, and severity of the disorder.
Dopplerography and duplex scanning are also possible. To determine the quality of trophism of nerve tissue.
Which method of diagnosing microangiopathy to choose: MRI, CT, angiography
Selection method
- MRI.
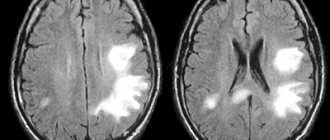
Ischemia of small vessels. Axial FLAIR (a) and T1-weighted ( b ) imaging. In the axial dark-fluid imaging mode, hyperintense zones are identified, consisting of small foci with clear boundaries and/or nodular foci merging with each other. On T1-weighted imaging, these areas are hypointense.
Is MSCT of cerebral vessels informative for lesions of small vessels?
SAE:
- Confluent hypodense zones in the brain parenchyma.
Lacunar strokes:
- Clearly demarcated hypodense lesions measuring 2-5 mm without volumetric effect
- Characteristic localization.
What will MRI images of the brain show in small vessel ischemia?
SAE:
- Confluent hyperintense areas on T2-weighted and proton density-weighted images or hypointense areas in the white matter on T1-weighted images.
Lacunar strokes:
- Well-demarcated hyperintense lesions measuring 2-5 mm on T2-weighted and proton density-weighted images or hypointense areas without evidence of volumetric effect (on T1-weighted images) of the above characteristic location.
Amyloid angiopathy:
- Multilocular microhemorrhages on T2*-weighted images.
Treatment
Therapy involves solving three problems. Eliminating the root cause, relieving symptoms, preventing complications.
There are two methods: conservative or surgical. In the vast majority of cases, the use of medications and, if necessary, lifestyle adjustments are sufficient. What medications are prescribed?
For hypertension and symptomatic increase in blood pressure:
- Means for lowering blood pressure. Beta blockers (Propranolol, Anaprilin, Metoprolol), ACE inhibitors (perindopril in different variations), calcium antagonists (Diltiazem or Verapamil), diuretics (Veroshpron, Hypothiazide), also diuretics, also centrally acting medications (Moxonidine).
- Statins. To adjust the concentration of cholesterol and other lipids in the bloodstream.
In addition, patients are advised to correct their diet (minimum fat and up to 7 grams of salt per day), adequate drinking regimen (1.3-1.8 liters or more, as needed, taking into account the recommendations of a specialist).
Diabetes:
- Antihyperglycemic agents, insulin as needed.
- Statins.
It is also possible to use medications to lower blood pressure levels.
Lenticulostriate type:
The deposition of calcium salts does not always require correction. There is no specialized treatment. Symptomatic drugs are used.
As for the amyloid form:
- A nicotinic acid. The main means of combating violations.
- Immunosuppressants, glucocorticoids (Prednisolone and analogues), cytostatics as needed. But this occurs extremely rarely. The purpose of these drugs is to reduce the activity of the body's defenses.
Systematic administration of vitamin-mineral complexes is indicated for all categories of patients.
Physiotherapy and acupuncture have proven themselves well.
Surgical correction is rarely needed. If there are clear foci of microangiopathy and there is a critical disturbance in the nutrition of nerve tissue in this particular area of the brain. With an additional condition: the drugs do not help.
Attention:
None of these methods can completely eliminate the disorder in the later stages. Foci of gliosis and scars do not disappear anywhere.
However, there is every chance of bringing the disorder under control. Moreover, the body, through the development of collaterals, can cope quite well on its own. You just need to support him.
What do white and black spots mean on MRI images?
Zones of altered MR signal may indicate:
- tissue ischemia;
- edema;
- necrosis;
- purulent melting;
- tumor transformation;
- metastatic lesion;
- gliosis;
- demyelination;
- degeneration, etc.
The radiologist describes the signal intensity, size and location of the lesion. Taking into account the information received, the patient’s complaints and data from previous examinations, the specialist can assume the nature of the pathological changes.
Acute disseminated encephalomyelitis on MRI
Possible complications
Consequences are relatively rare. Years pass from the development of microangiopathy to the final outcome. However, you cannot relax.
Possible problems include:
- Stroke. Acute cerebrovascular accident. Provokes the death of nerve tissue. Severe disability with neurological deficit. The death of a person is possible and even probable.
- Encephalopathy. The process is similar, but there is no destruction of cerebral structures yet.
- Vascular dementia. Dementia due to insufficient brain nutrition.
Complications develop spontaneously. Treatment is the only way to prevent them.
Why does cerebral microangiopathy develop?
- Cerebral microangiopathy is damage to small blood vessels in the brain.
- Occurs in more than 30% of people over 60 years of age
- Associated with vascular risk factors.
SAE (subcortical arteriolosclerotic encephalopathy):
- Subcortical atherosclerotic encephalopathy (SAE) or Binswanger's disease
- Diffuse subcortical lesion
- Evidence of tissue adaptation to hypoperfusion with a decrease in oligodendroglia and myelin content
- Localization: periventricular and subcortical white matter, excluding arcuate fibers.
Lacunar strokes:
- Small strokes caused by occlusion of penetrating arterioles with a diameter of 40-200 µm due to lipid hyaline degeneration and fibrinoid necrosis
- Localization: basal ganglia, thalamus, internal and external capsules, periventricular sections, pons.