Anaprilin is the first developed representative of the group of beta-blockers, the action of which is aimed at stabilizing blood pressure levels. Based on the drug intake, specialists can judge the effectiveness of new medications of this class. As a rule, patients take Anaprilin for blood pressure, but the drug has an additional antiarrhythmic effect, helping to normalize cardiac activity in people with vascular disorders. At what pressure levels can you take the drug and how to dose it correctly to avoid negative effects?
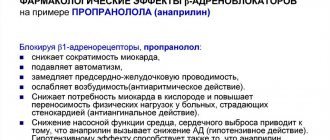
General characteristics of the product
Anaprilin for blood pressure belongs to the group of non-selective beta-adrenergic receptor blockers. The medicine has antiarrhythmic, hypotensive, antiangial properties, due to which it effectively lowers blood pressure without placing additional stress on the myocardium.
After taking a single dose of the drug, a decrease in systolic and diastolic pressure is observed, both in horizontal and vertical positions
Regular use of the medication allows you to achieve the following results:
- reduce the automaticity of the sinus node;
- reduce the excitability of the heart muscle;
- prevent the occurrence of ectopic contractions;
- normalizes the frequency of contractions of the heart muscle;
- inhibits atrioventricular conduction;
- reduces the oxygen demand of cardiomyocytes.
By blocking adrenergic receptors, anaprilin reduces blood pressure in hypertension resulting from disruption of the endocrine and excretory systems (essential and renal hypertension).
Composition and release forms
Anti-pressure tablets Anaprilin are available in dosages of the active substance in concentrations of 10 and 40 mg. To date, an injection form of the product has been developed, which is available in ampoules of 0.25%.
The medication is available in a plastic jar, which can contain 10, 40, 50, 60, 100 tablets.
The active substance in the drug is propranolol hydrochloride, which is used to lower blood pressure levels. The composition also includes additional components:
- microcrystalline cellulose;
- calcium stearate;
- talc;
- corn starch;
- colloidal silicon dioxide;
- hypromellose.
A wide range of dosages of tablet forms of the drug makes it possible for patients to select the required amount depending on the prescribed dosage regimen.
For what conditions is it used?
The blood pressure medicine Anaprilin is prescribed by a specialist when diagnosing the following conditions:
- Increased blood pressure due to essential or symptomatic hypertension.
- Treatment of coronary heart disease, angina pectoris, myocardial infarction after stabilization of vital signs.
- Irregular heart rhythm with a significant increase in heart rate.
- A disorder of the autonomic nervous system, when patients experience frequent attacks of panic attacks.
- Portal hypertension due to liver cirrhosis.
- Essential tremor.
The drug is effective in the initial stages of hypertension, therefore suitable for treating young patients
The drug is prescribed for high blood pressure, when the disease is complicated by left ventricular hypertrophy and rhythm disturbances. In addition, the drug serves as an effective prevention of migraine, which accompanies attacks of arterial hypertension.
Tachycardia
Thyrotoxicosis
Iron deficiency
Climax
Menopause
9339 12 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Tachycardia: causes of occurrence, in what diseases it occurs, diagnosis and treatment methods.
Definition
Tachycardia is a condition in which the heart rate is more than 100 beats per minute. Tachycardia is not an independent disease, but is a symptom (manifestation) of certain diseases. In addition to rapid heartbeat, this condition is characterized by shortness of breath, weakness, chest pain, and sometimes loss of consciousness.
If shortness of breath and chest pain worsens, you should immediately seek medical help.
Types of tachycardia
One of the classifications divides tachycardia into physiological and pathological.
Physiological tachycardia is characterized by the absence of damage to the heart muscle and cardiac pathways. This type of tachycardia can be called compensatory, since it develops in response to an increase in the body’s need for oxygen, for example, during sports, psycho-emotional stress, being at high altitudes, etc.
Physiological tachycardia is characterized by the following manifestations:
- changes in heart rate are transient (not permanent);
- there is an obvious connection with a provoking factor (stress, severe anxiety, physical activity);
- upon completion of the action of the provoking factor, the heart rate gradually returns to normal;
- there are no pathologies from the cardiovascular system (for example, congenital heart defects, previous heart attacks, damage to the heart valve apparatus and other heart rhythm disorders).
Pathological tachycardia is observed in the following diseases and conditions:
- Hyperfunction of the thyroid gland (hyperthyroidism, thyrotoxicosis, diffuse toxic goiter).
- Diseases of the adrenal glands with their hyperfunction and, as a result, increased release of adrenaline into the blood.
- Damage to the conduction pathways of the heart due to a heart attack, congenital pathology of the heart valve apparatus.
- Presence of anemia (decreased blood hemoglobin level).
- Damages of the heart muscle (for example, myocarditis, pericarditis).
- Hormonal changes in the body (pregnancy, menopause).
Possible causes of tachycardia
Tachycardia with
hyperfunction of the thyroid gland
is more often observed in women than in men. An increase in thyroid hormone levels is reflected in the sinus node, which is located in the right atrium. It generates electrical impulses that cause myocardial contractions. When hormone levels are high, they reproduce chaotically, affecting the heart. As a result, the heart rate increases and tachycardia occurs.
Adrenal cortex dysfunction, or Addison's disease
, in which the adrenal glands cannot produce enough hormones. Their deficiency leads to the fact that the kidneys begin to quickly excrete sodium and water in the urine, dehydration of the body occurs, the water-electrolyte balance is disturbed, the blood thickens, circulation and blood supply to peripheral tissues slow down. Against the background of these changes, pathological changes in the cardiovascular system occur.
For anemia
the increase in the number of heart contractions is due to the need to maintain the required level of oxygen in the blood in conditions of hemoglobin deficiency.
Let us recall that hemoglobin is a carrier of oxygen to tissues and is found in red blood cells.
When hemoglobin levels decrease, an increase in heart rate allows blood and oxygen to be “driven” to the tissues faster, which makes it possible to partially maintain the required level of oxygenation. There are several types of anemia, including those associated with bone marrow pathology (for example, aplastic anemia, leukemia), with a lack of microelements (iron deficiency, B12 and folate deficiency anemia), anemia due to blood loss (chronic and acute).
If you suspect the development of anemia due to acute blood loss, you should immediately seek medical help.
Tachycardia
in pregnant women is caused by both an increase in the need of the mother and fetus for oxygen, and an increase in the consumption of serum iron, folate, and cyanocobalamin.
Tachycardia may develop while taking certain medications
, drinking
coffee
and
caffeine-containing products
, energy drinks containing
taurine, smoking
.
Which doctors should I contact?
If you suspect a pathology of the thyroid gland or adrenal glands, you should contact an endocrinologist. To treat conditions associated with cardiac dysfunction, see a cardiologist. If you have anemia, see a therapist or hematologist. Pregnant women are observed in the antenatal clinic, where an obstetrician-gynecologist can promptly identify the pathology and prescribe treatment.
Diagnosis and examinations for tachycardia
When a patient presents with symptoms characteristic of tachycardia, it is necessary to find out whether the tachycardia is the root cause of the deterioration in well-being that prompted the patient to see a doctor, or whether it is secondary and there is an underlying disease.
If there is a suspicion of thyroid pathology, the level of thyroid hormones in the blood (T3 - triiodothyronine, T4 - thyroxine and their free fractions) and the level of thyroid-stimulating hormone are determined.
Pharmacological properties
After taking the drug, B-adrenergic receptors are inhibited, resulting in a decrease in the intracellular concentration of calcium ions, due to which the heart rate slows down, myocardial excitability decreases, and the number of heart contractions decreases.
Due to its antiarrhythmic effect, regular use of the drug helps reduce the number of deaths after a heart attack
What pharmacological effect can be achieved with regular use of the medication:
- Hypotensive. Helps reduce minute blood volume, reduces upper and lower pressure, stimulates peripheral vessels. Reduces the activity of the renin-angiotensin system in patients with impaired renal function. The therapeutic effect is achieved 14 days after administration.
- Antianginal. Reduces the need of heart cells for oxygen, slows down the heart rate, thereby improving the capacity of the heart. However, in patients with chronic heart failure, myocardial oxygen demand may increase, which is due to increased diastolic pressure in the left ventricle.
- Antiarrhythmic. Reduces the increased activity of the sympathetic nervous system, prevents spontaneous excitability of the sinus pacemaker. By reducing the heart's need for oxygen, ischemic manifestations are reduced.
The active components are quickly absorbed into the bloodstream, due to which the pressure stabilizes in a short time. Propranolol is excreted by the kidneys in the form of metabolites.
Pharmacodynamics
Non-selective beta blocker. It has antianginal, hypotensive and antiarrhythmic effects. By non-selectively blocking beta-adrenergic receptors (75% beta1- and 25% beta2-adrenergic receptors), it reduces the formation of cAMP from ATP stimulated by catecholamines, as a result of which it reduces the intracellular supply of calcium, has a negative chrono-, dromo-, batmo- and inotropic effect (reduces the frequency heart contractions, inhibits conductivity and excitability, reduces myocardial contractility). At the beginning of the use of beta-blockers, the total peripheral vascular resistance increases in the first 24 hours (as a result of a reciprocal increase in the activity of alpha-adrenergic receptors and the elimination of stimulation of beta2-adrenergic receptors in the vessels of skeletal muscles), but after 1-3 days it returns to the original level, and with long-term administration it decreases. The hypotensive effect is associated with a decrease in cardiac output, sympathetic stimulation of peripheral vessels, a decrease in the activity of the renin-angiotensin system (important in patients with initial hypersecretion of renin), the sensitivity of the baroreceptors of the aortic arch (there is no increase in their activity in response to a decrease in blood pressure) and an effect on the central nervous system. The hypotensive effect stabilizes by the end of 2 weeks of the course.
The antianginal effect is due to a decrease in myocardial oxygen demand (due to the negative chronotropic and inotropic effect). A decrease in heart rate leads to prolongation of diastole and improved myocardial perfusion. By increasing end-diastolic pressure in the left ventricle and increasing the stretch of ventricular muscle fibers, it can increase oxygen demand, especially in patients with chronic heart failure.
The antiarrhythmic effect is due to the elimination of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased cAMP content, arterial hypertension), a decrease in the rate of spontaneous excitation of sinus and ectopic pacemakers and a slowdown of atrioventricular conduction. Inhibition of impulse conduction is observed predominantly in the antegrade and to a lesser extent in the retrograde directions through the atrioventricular node and along additional pathways. According to the classification of antiarrhythmic drugs, it belongs to group II drugs. Reducing the severity of myocardial ischemia - by reducing myocardial oxygen demand, post-infarction mortality can also be reduced due to the antiarrhythmic effect.
The ability to prevent the development of headaches of vascular origin is due to a decrease in the severity of dilation of cerebral arteries due to beta-blockade of vascular receptors, inhibition of platelet aggregation and lipolysis caused by catecholamines, a decrease in platelet adhesiveness, prevention of activation of blood coagulation factors during the release of adrenaline, stimulation of oxygen supply to tissues and a decrease in renin secretion. The reduction in tremor with the use of propranolol may be due to the blockade of beta2-adrenergic receptors. Increases the atherogenic properties of blood. Strengthens uterine contractions (spontaneous and caused by drugs that stimulate the myometrium). Increases bronchial tone.
Pharmacokinetics
It is quickly and fairly completely (90%) absorbed when taken orally and is relatively quickly eliminated from the body. Bioavailability after oral administration is 30-40% (the “first pass” effect through the liver, microsomal oxidation), with long-term use it increases (metabolites that inhibit liver enzymes are formed), its value depends on the nature of the food and the intensity of hepatic blood flow. Metabolized by glucuronidation in the liver. The maximum concentration in blood plasma is achieved after 1-1.5 hours. It is highly lipophilic and accumulates in lung tissue, brain, kidneys, and heart. Penetrates through the blood-brain and placental barriers into breast milk. Communication with blood plasma proteins - 90-95%. Volume of distribution: 3-5 l/kg. It enters the intestine with bile, is deglucuronidated and reabsorbed. The half-life is 3-5 hours, during a course of administration it can be extended to 12 hours. Excreted by the kidneys - 90%, unchanged - less than 1%. It is not removed by hemodialysis.
Mechanism of action in hypertension
Before starting a therapeutic course, patients are interested in the question of the effectiveness of the prescribed medication, and does it reduce blood pressure at high levels?
The hypotensive mechanism of action of this drug is due to its ability to block beta-adrenergic receptors of the myocardium and other tissues, which is an integral part of lowering blood pressure. Inhibition of renin production contributes to decreased secretion of angiotensin 2, which leads to a decrease in blood pressure and determines the effectiveness of the antihypertensive effect of pills.
Mechanism of action of the drug for hypertension
The vasodilating effect of Anaprilin is based on the following mechanisms:
- impact on vascular receptors;
- pronounced adrenergic blocking activity;
- increases the release of nitric oxide from endothelial cells;
- expansion of the vascular lumen;
- increased production of vasodilating factors (prostaglandins, prostacyclins);
- decreased production of norepinephrine by sympathetic nerve fibers;
- decreased permeability of blood vessels to potassium and sodium ions.
Mechanism of action of the drug
Anaprilin is a pharmaceutical widely used in the treatment of cardiac and related pathologies.
It is a non-selective (β1, β2) adrenergic blocker and has a hypotensive, antianginal and antiarrhythmic effect. Synonyms (analogues) – Propranolol, Obzidan, Inderal, Propamin. Non-selective β-blockers can affect β1 (located directly in the heart) and β2 (on the walls of blood vessels) adrenergic receptors.
By competitively blocking β1 receptors, anaprilin reduces blood pressure inside the ventricles, the influence of the sympathetic nervous system and catecholamines on the heart.
Blocking the sympathoadrenal influence causes a decrease in heart rate, a weakening of the force of heart contractions and a drop in cardiac output. As a consequence of the above, the myocardial oxygen demand and excitability decrease, intracardiac impulse conduction slows down, which subsequently eliminates myocardial hypoxia.
Does anaprilin reduce blood pressure?
Anaprilin affects pressure in the vascular bed by reducing minute blood volume in the case of systematic use. Also, the antihypertensive effect of β-AB is facilitated by blockade of the β1 receptor in the juxtaglomerular apparatus of the kidneys (reduces the release of renin into the bloodstream and the formation of angiotensin-2).
Additional effects of anaprilin on organs:
Membrane stabilizing effect - reduces lipolytic activity, time consumption for oxidative phosphorylation of fats;- Antioxidant effect;
- Improvement of oxyhemoglobin dissociation;
- Antiplatelet effect – release of endothelial prostacyclin;
- Bronchospasm;
- Depression of the central nervous system, libido, erection;
- Reduced intraocular pressure;
- Reducing glucose levels, increasing cholesterol, suppressing the intensity of lipolysis;
- Suppresses the transformation of thyroxine into triiodothyronine;
- Increased tone and contractile activity of the myometrium.
Selection of the optimal dose
Before starting a treatment course, the patient needs to determine the daily dose of the drug, which will help eliminate hypertension and ensure stable blood pressure and pulse rate. It will also determine whether or not the drug can be used at elevated blood pressure levels when the heart rate is normal.
The dosage and frequency of administration are determined depending on the severity of hypertension, the presence of concomitant pathologies and the age of the patient
It is possible to achieve a decrease in pressure much later than normalization of sinus rhythm, which depends on the concentration of the active substance. It is recommended to take Anaprilin for high blood pressure with a full treatment course of at least 21 calendar days. The intervals between doses are 1–2 months.
The dosage of the drug depends on the indications:
- With high blood pressure. The starting dose of the drug is 80 mg, which must be divided into 2 doses. If the drug does not reduce blood pressure, the dosage is increased to 120–160 mg per day, that is, 40 mg should be taken in 3–4 doses.
- With high heart rate. At the initial stage of treatment, the daily dose is divided into 20 mg, which are drunk 3 times a day. In the absence of a therapeutic effect, the dose is increased to 80–120 mg per day.
With a normal number of heartbeats and high blood pressure, the drug is used to prevent migraine attacks and tremor. The starting dose is 20 mg 3 times a day, and the maximum allowable dose is 160 mg.
First aid for tachycardia
The normal heart rate (HR) for a healthy adult is 60–80 beats per minute. To calculate your heart rate, you need to place the index and middle fingers of one hand on the wrist of the other and count the pulse rate for 15 seconds, then multiply the resulting number by 4.
If the heartbeat exceeds 90 beats, tachycardia begins. However, not every attack requires calling a doctor. For example, physiological (natural) causes of increased heart rate go away on their own if the provoking factor is eliminated - reduce physical activity, stabilize the emotional state, quit smoking, etc.
Pathological variants of tachycardia begin for no apparent reason and are accompanied by symptoms of oxygen starvation, decreased blood pressure and a feeling of fear. This condition can stop on its own, but in some cases an attack of tachycardia occurs due to serious pathology (heart or respiratory failure, hypertensive crisis). And then the rhythm of the heart can only be adjusted in the hospital.
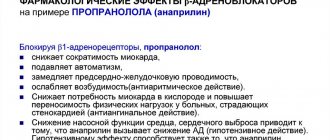
Disruption of the normal heart rate (HR) can lead to serious complications such as:
- heart attack;
- stroke;
- acute heart failure;
- thrombophlebitis;
- injuries resulting from fainting.
An attack of tachycardia for no apparent reason requires a visit to the doctor, even if the episode of increased heart rate goes away on its own
What to do during an attack of tachycardia
- 1
Take a horizontal position. This will take the load off the heart and blood vessels. - 2
Release the chest and neck - unfasten the buttons, loosen the collar, remove the tie. Tight clothing restricts breathing, so the pressure needs to be loosened. - 3
Place a pillow under your neck. Throwing back the head can cause circulatory problems, which is unacceptable in conditions of tachycardia. - 4
Provide fresh air flow. When the heart rate increases, the body experiences oxygen starvation, so an open window can alleviate the condition. - 5
Drink a glass of cold water in small sips. Hot drinks, coffee or strong tea are prohibited, and douse yourself with cold water. - 6
Cool your face - for example, place a towel soaked in cold water on your forehead and temple areas. - 7
Perform breathing exercises. A cycle of repeating slow, deep breaths, holding your breath for 5 to 8 seconds, and exhaling slowly can slow your heart rate. - 8
If signs of panic appear, you should take a sedative. - 9
If an attack of tachycardia does not occur for the first time, you should take antiarrhythmic drugs prescribed by your doctor.
For tachycardia at a young age, massage of the neck and back of the head is acceptable. This method is contraindicated for the elderly due to the high risk of heart attack and stroke.
When to call the doctor
If the tachycardia is caused by a serious heart pathology, the first aid measures described above may not be sufficient. If tachycardia does not go away within 15–20 minutes, especially while taking antiarrhythmic drugs, you should immediately call an ambulance.
Other reasons to call a doctor
- Heart rate is 120 beats per minute or higher.
- Intense pain behind the sternum, which is accompanied by pallor, sweating, fear of death and a burning sensation spreading to the left arm, lower jaw or abdomen.
- Tachycardia is accompanied by severe headache and a feeling of numbness in the limbs or half of the face.
- The attack occurred during pregnancy.
Features of drug cancellation
If it is necessary to take a break from treatment with Anaprilin, the dose should be reduced gradually until complete withdrawal, since abrupt cessation of use of the drug can cause withdrawal syndrome.
Abrupt refusal to take medication can cause an attack of angina, tachycardia and increased blood pressure
Experts recommend discontinuing the use of the medication in the following cases:
- Reducing the number of heart contractions to 50 beats/min.
- At low pressure, when systolic blood pressure drops to 100 mm. rt. Art.
- Development of bronchial spasm.
- Disturbance in the functioning of the liver excretory system.
- Depressive state.
- Ventricular arrhythmia.
The optimal withdrawal period is considered to be 14 days from the moment the patient reduces the dosage until the patient completely stops using the tablets. As a rule, the dose is reduced by 10–40 mg every 6–7 days.
special instructions
The use of the drug during pregnancy is permitted in cases where the benefits to the woman’s body outweigh the potential risks to the fetus. During the treatment course, it is necessary to constantly monitor the child’s condition, since the following complications may occur:
- decrease in the number of heart contractions;
- decrease in glucose concentration in the bloodstream;
- intrauterine growth retardation.
A few days before the expected birth, Anaprilin should be discontinued.
Active substances are absorbed into breast milk, so women should switch their baby to artificial feeding
Elderly patients should take the drug with caution. Thus, once every three months, the concentration of glucose in the bloodstream of diabetics is monitored and the functional state of the kidneys is monitored.
Anaprilin
Beta blockers should not be used in patients with untreated chronic heart failure until the condition has stabilized.
Before using the drug, patients with heart failure (early stages) must use cardiac glycosides and/or diuretics.
Monitoring of patients taking the drug should include monitoring heart rate and blood pressure (daily at the beginning of treatment, then once every 3-4 months), recording an electrocardiogram.
In elderly patients, it is recommended to monitor renal function (once every 4-5 months).
In case of increasing bradycardia (less than 60 beats/min), arterial hypotension (systolic blood pressure less than 100 mm Hg), atrioventricular block, bronchospasm, ventricular arrhythmias, severe liver and/or kidney dysfunction in elderly patients, it is necessary reduce the dose of the drug or stop treatment.
Use the drug with caution in patients with first degree atrioventricular block.
The patient should be trained in the method of calculating heart rate and instructed about the need for medical consultation if the heart rate is less than 60 beats/min.
It is recommended to discontinue therapy if depression caused by taking beta-blockers develops.
Patients who use contact lenses should take into account that during treatment with beta-blockers, there may be a decrease in the production of tear fluid.
Treatment of coronary heart disease and persistent arterial hypertension should be long-term - taking the drug is possible for several years.
Discontinuation of treatment is carried out gradually, under the supervision of a physician: abrupt withdrawal can dramatically increase myocardial ischemia, anginal syndrome, and worsen exercise tolerance. Cancellation is carried out gradually, reducing the dose by 25% every 3-4 days for 2 weeks or more.
When deciding on the use of the drug Anaprilin in patients with psoriasis, one should carefully weigh the expected benefits and the possible risk of exacerbation of psoriasis.
In thyrotoxicosis, propranolol may mask certain clinical signs of thyroid hyperfunction (for example, tachycardia). Abrupt withdrawal in patients with hyperthyroidism is contraindicated as it can worsen symptoms.
Isolated reports of myasthenia gravis have been reported during propranolol therapy. If muscle weakness occurs, consult a doctor. In patients with diabetes mellitus, the drug is used under the control of blood glucose concentration (once every 4-5 months). Use with caution simultaneously with hypoglycemic agents, since hypoglycemia may develop during prolonged breaks in food intake, as well as during insulin therapy. Moreover, its symptoms such as tachycardia or tremor will be masked due to the action of the drug. The patient should be instructed that the main symptom of hypoglycemia during treatment with the drug is increased sweating. There is also a risk of hyperglycemia when taking oral hypoglycemic agents.
When taking clonidine concomitantly, it can be discontinued only a few days after discontinuation of the drug.
Beta blockers may increase sensitivity to allergens and the severity of anaphylactic reactions. Propranolol may cause severe reactions to a number of allergens when administered to patients with a history of severe anaphylactic reactions to these allergens. These patients may not respond to the usual doses of epinephrine (adrenaline) used to treat anaphylactic shock.
For pheochromocytoma, it is used only in combination with alpha-blockers. Concomitant use with antipsychotics (neuroleptics) and tranquilizers is contraindicated.
Drugs that reduce catecholamine levels (for example, reserpine) may enhance the effect of propranolol. Therefore, patients taking combinations of drugs should be under constant medical supervision to detect arterial hypotension and bradycardia.
During treatment, intravenous administration of verapamil and diltiazem should be avoided.
Use with caution in combination with psychotropic drugs, for example, MAO inhibitors, when their course is used for more than 2 weeks.
A few days before general anesthesia with chloroform or ether, it is necessary to stop taking the drug (increased risk of depression of myocardial function and the development of arterial hypotension). It is necessary to warn the anesthesiologist that the patient is taking Anaprilin.
The effectiveness of beta-blockers in smokers is lower than in non-smoking patients. The drug Anaprilin should be discontinued before testing the content of catecholamines, normetanephrine and vanillylmandelic acid in the blood and urine, and titers of antinuclear antibodies.
Therapy with the drug should be suspended if there is a respiratory infection of the lower respiratory tract accompanied by difficulty breathing. The use of beta2-agonists and inhaled glucocorticosteroids is allowed. Resumption of use of the drug is possible only after the patient has completely recovered. In case of repeated infection, as well as in the case of isolated bronchospasm, the use of the drug should be stopped completely.
It is not recommended to drink alcohol during treatment.
Beta-blockers should be used with caution in patients with peripheral circulatory disorders, as these symptoms may worsen.
Natural licorice should be avoided: foods rich in protein may increase the bioavailability of propranolol.
Propranolol may give a positive result in a doping test.
Side effects
If recommendations for dosing of the drug are not followed, side effects from various systems may occur:
- Cardiovascular (circulatory disorders, arterial hypotension, increasing symptoms of heart failure).
- Hematopoietic (leukopenia, thrombocytopenia).
- Nervous (sleep disorder, dizziness, depression, malaise).
- Respiratory (coughing attacks, shortness of breath, pharyngitis, bronchospasm).
- Gastrointestinal (nausea, vomiting, diarrhea, pain in the epigastric region).
- Skin manifestations (rashes, itching, partial hair loss).
- Visual tract (dry eye mucosa, pain, decreased visual acuity).
Today, Anaprilin remains one of the most common and effective antihypertensive drugs, which at the same time help normalize heart rhythm. However, the medicine has a number of negative effects that affect the activity of all organs and systems. Therefore, for arterial hypertension, the course of treatment should be accompanied by periodic intervals that prevent a decrease in sensitivity to the active components and reduce the number of side effects.
Indications for use
The primary indications are:
Coronary heart disease (unstable angina, post-infarction cardiosclerosis);- Essential or renal hypertension;
- Heart rhythm disturbances (sinus and paroxysmal tachycardias, tachyarrhythmias, ventricular extrasystoles);
- Congestive heart failure;
- Glaucoma;
- Migraine headaches;
- Sympathoadrenal crises;
- Diencephalic syndrome, accompanied by pronounced heartbeat, pulsation in the head;
- Essential tremor;
- Thyrotoxicosis;
- Pheochromatocytoma (in combination with α-blockers);
- Phobic disorders, obsessive states;
- Primary weakness of labor, threat of bleeding in the early postpartum period.
IHD . β-blockers have a more pronounced anti-ischemic effect, which is comparable to nitrates, Ca2+ antagonists, therefore they are included in the first line of treatment for various types of angina. Prescribing anaprilin reduces the number of uses of nitroglycerin and increases tolerance to physical activity.
Myocardial infarction. In the acute period, β-AB is prescribed to relieve a painful attack, limit the area of necrosis, and prevent the occurrence of fatal arrhythmias. The use of anaprilin on days 5-12 of the development of myocardial infarction significantly reduces the mortality rate.
Arterial hypertension. Therapy with β-blockers in combination with diuretics reduces the likelihood of stroke by 40%. It is advisable to use anaprilin in the early stages of the development of hypertension, especially in the presence of symptoms of sympathicotonia.
Heart failure. By preventing the effect of β-adrenergic stimulation, β-ABs prevent the cardiotoxic effect of catecholamines and improve the structural and functional state of the myocardium. In combination with antiarrhythmic and anti-ischemic effects, anaprilin prevents myocardial and vascular remodeling.
Rhythm disturbances. The effectiveness of anaprilin in the prevention and relief of supraventricular tachycardia and paroxysmal atrial fibrillation has been demonstrated.