Has restrictions during pregnancy
Prohibited during breastfeeding
Has restrictions for children
Has restrictions for older people
Has limitations for liver problems
Has limitations for kidney problems
Pressure changes in blood vessels increase the load on the myocardium, which often results in heart attack and death. To prevent the progression of hypertension and relieve the myocardium, cardiologists use antihypertensive drugs of different pharmacological groups. For the treatment of heart pathologies, drugs are prescribed in complex treatment and monotherapy. Quite often, doctors prescribe Anaprilin and Enalapril to lower the blood pressure index.
In this article, we will figure out what the difference is between Enalapril and Anaprilin.
Review of Anaprilin and Enalapril
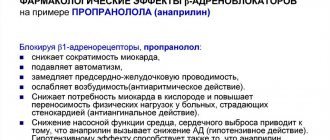
The active ingredient in Anaprilin is propranolol. One tablet contains propranolol 10.40 mg. Anaprilin is a non-selective beta-blocker. Properties of this medication:
- antihypertensive;
- antiarrhythmic;
- antianginal.
These properties of the drug make it possible to use it in the treatment of cardiac pathologies with disturbances of heart rhythm and cardiac conduction, aggravated by hypertension.
Pharmacological effects of the drug
At the initial stage of therapy with β-blockers, the resistance of the peripheral parts of the blood flow system increases, but within 2-3 days it returns to its original level and gradually begins to decrease. This medication is prescribed for unstable hypertension of unknown etiology, when blood pressure surges occur chaotically and without clear reasons.
Normalizing blood pressure improves the patient’s well-being and reduces the risks of myocardial infarction and ischemic stroke.
Enalapril belongs to the pharmacological group of antihypertensive medications - ACE inhibitors (angiotensin-converting enzyme). The active ingredient in this product is enalapril in dosages of 5, 10 and 20 mg. This is a synthetic medication aimed at lowering the blood pressure index.
For decades, Enalapril has remained one of the most effective medications prescribed in the complex treatment of cardiac and vascular pathologies. This drug is not intended for self-medication; it can only be taken as prescribed by the attending physician with a clearly established dosage. The drug has diuretic properties.
Anaprilin
Beta blockers should not be used in patients with untreated chronic heart failure until the condition has been stabilized.
Before using the drug, patients with heart failure (early stages) must use cardiac glycosides and/or diuretics.
Monitoring of patients taking the drug should include monitoring heart rate and blood pressure (daily at the beginning of treatment, then once every 3-4 months), recording an electrocardiogram.
In elderly patients, it is recommended to monitor renal function (once every 4-5 months).
In case of increasing bradycardia (less than 60 beats/min), arterial hypotension (systolic blood pressure less than 100 mm Hg), atrioventricular block, bronchospasm, ventricular arrhythmias, severe liver and/or kidney dysfunction in elderly patients, it is necessary reduce the dose of the drug or stop treatment.
The drug should be used with caution in patients with first degree atrioventricular block.
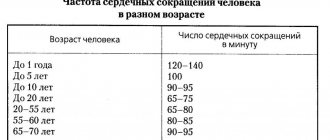
The patient should be trained in the method of calculating heart rate and instructed about the need for medical consultation if the heart rate is less than 60 beats/min.
It is recommended to discontinue therapy if depression caused by taking beta-blockers develops.
Patients who use contact lenses should take into account that during treatment with beta-blockers, there may be a decrease in the production of tear fluid.
Treatment of coronary heart disease and persistent arterial hypertension should be long-term - taking the drug is possible for several years.
Discontinuation of treatment is carried out gradually, under the supervision of a physician: abrupt withdrawal can dramatically increase myocardial ischemia, anginal syndrome, and worsen exercise tolerance. Cancellation is carried out gradually, reducing the dose by 25% every 3-4 days for 2 weeks or more.
When deciding on the use of the drug Anaprilin in patients with psoriasis, one should carefully weigh the expected benefits and the possible risk of exacerbation of psoriasis.
In thyrotoxicosis, propranolol may mask certain clinical signs of thyroid hyperfunction (for example, tachycardia). Abrupt withdrawal in patients with hyperthyroidism is contraindicated as it can worsen symptoms.
Isolated reports of myasthenia gravis have been reported during propranolol therapy. If muscle weakness occurs, consult a doctor. In patients with diabetes mellitus, the drug is used under the control of blood glucose concentration (once every 4-5 months). Use with caution simultaneously with hypoglycemic agents, since hypoglycemia may develop during prolonged breaks in food intake, as well as during insulin therapy. Moreover, its symptoms such as tachycardia or tremor will be masked due to the action of the drug. The patient should be instructed that the main symptom of hypoglycemia during treatment with the drug is increased sweating. There is also a risk of hyperglycemia when taking oral hypoglycemic agents.
When taking clonidine concomitantly, it can be discontinued only a few days after propranolol is discontinued.
For pheochromocytoma, it is used only in combination with alpha-blockers. Do not use simultaneously with antipsychotic drugs (neuroleptics) and tranquilizers.
Beta blockers may increase sensitivity to allergens and the severity of anaphylactic reactions. Propranolol may cause severe reactions to a number of allergens when administered to patients with a history of severe anaphylactic reactions to these allergens. These patients may not respond to the usual doses of epinephrine (adrenaline) used to treat anaphylactic shock.
Drugs that reduce catecholamine reserves (for example, reserpine) may enhance the effect of beta-blockers, so patients taking combinations of drugs should be under constant medical supervision to detect arterial hypotension and bradycardia.
During treatment with propranolol, intravenous administration of verapamil and diltiazem should be avoided.
Use with caution in combination with psychotropic drugs, for example, MAO inhibitors, when used for a course of more than 2 weeks.
A few days before general anesthesia with chloroform or ether, it is necessary to stop taking the drug (increased risk of depression of myocardial function and the development of arterial hypotension). It is necessary to warn the anesthesiologist that the patient is taking propranolol.
In smokers, the effectiveness of beta-blockers is lower.
The drug should be discontinued before testing the content of catecholamines, normetanephrine and vanillinmandelic acid in the blood and urine; antinuclear antibody titers.
Therapy with the drug should be suspended if there is a respiratory infection of the lower respiratory tract accompanied by difficulty breathing. The use of beta2-agonists and inhaled glucocorticosteroids is allowed. Resumption of use of the drug is possible only after the patient has completely recovered. In case of repeated infection, as well as in the case of isolated bronchospasm, the use of the drug should be stopped completely.
It is not recommended to drink alcohol during treatment (a sharp decrease in blood pressure is possible). Beta-blockers should be used with caution in patients with peripheral circulatory disorders, as these symptoms may worsen.
Avoid using natural licorice during treatment; Protein-rich foods can increase bioavailability.
Propranolol may give a positive result in a doping test.
The principle of action of the drugs
There is a misconception that Anaprilin and Enalapril are the same thing. However, these 2 drugs belong to different pharmacological groups and have different principles of action on the body.
Anaprilin is a non-selective beta-blocker. Propranolol blocks β1-adrenergic receptors and β2-adrenergic receptors, which helps inhibit the formation of ectopic foci in the atria, and also blocks focal neoplasms in the ventricles and atrioventricular node. The drug slows down the passage of an impulse through the Kent beam, which reduces the speed of passage of excitation. This principle helps reduce:
- Heart rate, which reduces the oxygen demand of cardiomyocytes;
- renin secretion;
- clearance in the kidneys, as well as the load on glomerular filtration;
- cardiac output, which is the basis for lowering blood pressure.
The medication also inhibits the process of lipolysis in subcutaneous tissue and prevents an increase in the concentration of free cholesterol molecules in the blood (an increase in the atherogenic coefficient occurs).
In patients with coronary artery disease, the frequency and intensity of attacks of stable and unstable angina are reduced, as well as the body's endurance increases, well-being improves and the need for nitrates decreases. The drug is prescribed as secondary prevention of heart attacks. The cardioprotective effect prevents a second heart attack and reduces the risk of death by 50%.
A single dose of tablets reduces systolic blood pressure and diastolic blood pressure, but the hypotensive effect of the drug appears after 2 weeks of use.
Absorption occurs in the digestive tract - 90% of the dose taken, 99% metabolism occurs in liver cells. The maximum concentration in plasma is 1-2 hours after taking the tablet, binding to plasma proteins is 90-95%. Passes through the placental barrier and is diagnosed in breast milk. The half-life is from 3 to 5 hours, 90% is excreted in the form of metabolites through the kidneys.
The effect of Enalapril is aimed at inhibiting the activity of angiotensin and increasing the activity of renin. Effective inhibition of ACE activity is achieved 2-4 hours after the tablet has been taken.
Indications for use and dosage of Enalapril
The reduction process begins an hour after taking the medication, and the peak effect of the medication occurs after 4-6 hours. The duration of the therapeutic effect depends on the dosage of the drug, as well as on the duration of the medication course. The hypotensive effect lasts for 24 hours.
The drug is absorbed by 60% in the digestive tract, metabolism occurs in liver cells. 90% of the active ingredient is excreted through the kidneys with urine, and 10% with feces.
Modern approaches to the treatment of atrial fibrillation
Lecture transcript
XXVI All-Russian Educational Internet Session for doctors
Total duration: 22:08
Oksana Mikhailovna Drapkina, executive director of the Internet Session, secretary of the interdepartmental council on therapy of the Russian Academy of Medical Sciences:
— The next lecture introduces us to the interesting world of arrhythmia. Professor Doshitsyn Vladimir Leonidovich. "Modern approaches to the treatment of patients with atrial fibrillation."
00:13
Doshitsyn Vladimir Leonidovich, professor:
- Dear Colleagues!
There are many aspects and controversial issues in the problem of solving patients with atrial fibrillation. Let me today dwell on controversial issues, which in many of their aspects do not have a generally accepted interpretation.
First of all, let me remind you that atrial fibrillation is one of the most significant arrhythmias. Its prevalence, according to modern data, in the general population reaches 2%. In elderly and senile people it is up to 10%. This arrhythmia is one of those that always requires some kind of intervention.
This arrhythmia causes a significant increase in the risk of embolic complications. Embolism associated specifically with atrial fibrillation accounts for more than half of all cardiac embolisms. Mostly these are strokes. But there may be atrial fibrillation associated with arterial embolism: renal, lower extremities, mesenteric, including from the pulmonary circulation - pulmonary artery embolism.
The presence of atrial fibrillation increases the risk of thromboembolism by 5 times. In patients with rheumatic diseases, especially mitral ones - 20 times.
New aspects of the classification, which was proposed last year by the European Society of Cardiology. The well-known, newly identified arrhythmia remains unknown where it will lead. It may become permanent. May be paroxysmal or persistent.
The most controversial issue is the difference between paroxysmal and persistent. Two criteria for distinction have been proposed. The first is temporary – 7 days (less paroxysmal, more persistent). The second is the ability to self-limit (supposedly characteristic of paroxysmal and not characteristic of persistent).
There's quite a bit of confusion here. Short episodes of less than seven days, resolving from medications, injections, and so on, were classified by some as persistent. Longer-lasting and self-terminating - to paroxysmal.
Now the European Society of Cardiology proposes to focus mainly on the time criterion. Less than seven days – paroxysm, more – persistent. It is proposed to identify another form - long-persistent. It can last for many months or even more than a year. But it allows the tactics of rhythm restoration (rhythm control), if it is possible, for example, to influence the cause of atrial fibrillation, the underlying disease.
The permanent form is when we are no longer talking about this possibility, but are talking only about the tactics of controlling the rhythm frequency.
03:35
It is well known that we can adhere to two tactics for managing a patient with recurrent, that is, paroxysmal or persistent fibrillation. The first tactic is most appealing to the patient and the doctor. This is the restoration and maintenance of sinus rhythm. But another strategy is also valid - maintaining the number of heartbeats (anticoagulant, antiplatelet therapy) while maintaining atrial fibrillation, subject to an acceptable quality of life.
There have been a lot of studies comparing these two strategies. Ultimately, to date, these studies have shown no fundamental difference (in terms of basic life prognosis) in these two management tactics. Both are valid. The doctor has to choose his own tactics.
On the basis of which a specific doctor, a specific patient determines whether he will restore the patient’s rhythm with atrial fibrillation or not.
I would like to start here with the last line. Subjective tolerance of arrhythmia by the patient. Does the patient want to restore the rhythm? In one case, he simply craves it and categorically insists. In another case, he does not feel the arrhythmia and is critical of the doctor’s urgent desire to restore his sinus rhythm. This is one of the most important criteria. If the patient does not want, does not feel arrhythmia, his quality of life is acceptable for him, then this is one of the most important points in choosing tactics for controlling the rhythm frequency, and not controlling the arrhythmia itself.
Second line from bottom. Possibility of influencing etiology. If there is such an opportunity (and very often there is), then we take advantage of this opportunity. This is the most important condition for an effective impact on the quality of life and the ability to maintain sinus rhythm. If this is not possible (some kind of congenital defect where surgical intervention is impossible), there is no real chance of maintaining sinus rhythm. More acceptable tactics are to control the frequency and quality of life.
Third point from the bottom. The risk of “normalization” thromboembolism (for example, stroke when sinus rhythm is restored). When is such a stroke at its highest? If there are blood clots in the left atrium. If there have already been episodes of thromboembolic complications (in particular, stroke, transient ischemic attacks, and so on). The high risk of “normalization” thromboembolism forces us to prefer the tactics of not restoring the rhythm, but rather the tactics of controlling the frequency when the arrhythmia persists. It is not always possible to reduce the risk of “normalization” thromboembolism using active anticoagulant therapy.
07:06
How easy it is to maintain and restore sinus rhythm with the help of antiarrhythmic drugs. If it works out easily, then this is in favor of the fact that we can use rhythm control tactics. If you have to do it with great difficulty, very often, use large doses, then this is rather evidence in favor of the fact that you will have to choose tactics to control the rhythm frequency.
Further. Frequency and duration of arrhythmia episodes. In general, how long is the medical history? Over time, a persistent arrhythmia is established. Typically, arrhythmia progresses in such a way that attacks and episodes become more frequent, lengthen, and are less easily controlled. This is facilitated by the presence of pronounced organic changes in the heart. These are the factors that the doctor has to take into account when deciding whether he will or will not restore the rhythm. But still, it is natural for both the doctor and the patient to restore and maintain the rhythm.
What opportunities do we have for this? The European Society of Cardiology issued recommendations last year. Drugs with proven effectiveness. Shown here are those that are registered in Russia. In fact, there are more of them listed. But among them there are many that are not used in our country.
First-line drugs with proven effectiveness. "Propafenone" ("Propanorm") and "Amiodarone" ("Cordarone"). In principle, both can be used orally and intravenously. But we don't have intravenous "Propafenone" yet. Oral "Cordarone" is not very convenient for relief, since it acts slowly and you have to give quite large doses. In reality, it's a "Pill in your pocket" of "Propafenone" and intravenous introduction of Cordarone.
In addition, less effective and more toxic drugs. As for insufficiently studied ones, this is perhaps not entirely accurate. Especially for our country, because Novokain-amid and Quinidine have been used for many decades. They are used less often. The grade of recommendation and level of evidence is lower.
09:49
What we really have. In addition to what is named (“Cordarone” and “Propafenone” intravenous), there is also “Nibentan”, which is now used quite rarely. Oral "Propafenone", "Cordarone" and "Quinidine".
Is there anything beyond this. Doctors also use “Pill in your pocket” for relief. Let's say there is "Ritmilen", which used to be used quite often. There are beta blockers “Obzidan”, “Anaprilin” (“Anaprilin”), which are also used (in any case, they are often recommended by practical doctors).
But it has been proven that these drugs are still less effective. Basically, two drugs are actually recommended today. These are "Propanorm" and "Cordarone".
There are several schemes. I want to pay special attention to the “Pill in your pocket” strategy, because it allows you to stop paroxysms on an outpatient basis without hospitalization.
Italian authors have proposed two possible schemes. One of them is active (on the right). This is a single dose of 3-4 tablets of "Propafenone" (450 - 600 mg orally). The efficiency here is estimated at 88%.
And another, more cautious scheme, when the doctor for some reason is afraid to immediately give such a large single dose. The first dose is two tablets orally. After an hour, if there is no effect, take another tablet (150 mg). After another 4-6 hours, if there is no effect, take another tablet. The overall efficiency is below 56%.
I want to emphasize that if the patient is not familiar with this drug, then at the very first dose it should be given not 300 mg, but one tablet - 150 mg. Unpredictable effects are possible with any antiarrhythmic drug.
12:08
Maintaining sinus rhythm. The latest recommendations from the European Society of Cardiology name five drugs. Among them are “Cordarone”, “Dronedarone” or “Multab” or “Cavenit”, which is not registered with us. "Propanorm", "Sotalol" ("Sotalol") and "Sotalex" ("Sotalex").
In fact, there are four drugs that we can use, we have them in pharmacies. “Cordaron”, “Propanorm”, “Sotalex”, and now “Multab” (“Dronedaron”) has appeared. We don’t have much experience with Multab yet. We just have quite a solid experience in international research. In our country it has not yet been sufficiently studied.
"Cordarone", "Propafenone" and "Sotalol" have been studied quite well. They have approximately comparable efficiency. These three drugs have been proven to have a significant preventive effect.
In practice, doctors sometimes use other drugs. In our country, there is experience in using “Ethacyzin” and “Allapinin”. Previously, Ritmilen (Disopyramide) was used quite widely.
Disopyramide is now used very rarely in European countries, which is mainly due to its frequent side effects. "Allapinin" and "Etatsizin" have a significantly smaller international evidence base. Maybe over time this base will appear and they will take some place. But today this is not included in international recommendations and is only mentioned in domestic recommendations.
A big controversial issue. Can we use first class drugs (in particular, Propafenone) to relieve and prevent episodes of atrial fibrillation in patients with arterial hypertension and chronic forms of coronary heart disease.
There were studies "CAST-1", "CAST-2" and others, which showed that in patients with acute myocardial infarction, patients with heart failure, there was a deterioration in life prognosis with long-term use of these drugs.
In fact, it has been proven that acute myocardial infarction, low ejection fraction and severe heart failure according to the New York classification of stages 3-4 are contraindications for the use of class 1 C drugs.
Meta-analyses of the same CAST studies showed that if these drugs are effective in small doses and in short courses (the so-called “mild suppression”), and this also applies to ventricular ari, it is accompanied by an improved prognosis. Not a deterioration, but, on the contrary, an improvement. If these drugs (class 1C) are given in combination with beta blockers, then the risk of death is reduced, that is, the negative effect is neutralized.
15:45
To date, this provision is still valid. Class 1 antiarrhythmics are recommended mainly for patients without significant organic changes in the heart.
However, the question remains: what are pronounced organic changes in the heart? Explanation given in a number of authoritative literary sources. This refers to acute forms of coronary heart disease, severe signs of heart failure with a decrease in ejection fraction and severe left ventricular hypertrophy (LVH) with an increase in wall thickness of more than 14 mm.
If there is none of this, but there is simply arterial hypertension and a stable course of chronic ischemic heart disease, then this is not a categorical contraindication to the prescription of class 1 drugs for relief and in small doses for prevention.
In this regard, a very large study “Prostor” was conducted in Russia last year. It aimed to study the effectiveness and safety of Proponorm in patients with transient atrial fibrillation in the presence of moderate signs of heart failure with preserved systolic function of the left ventricle.
Centers Moscow, Moscow region, Novosibirsk, Irkutsk, Ryazan, Chelyabinsk, Nizhny Novgorod. The names of the leaders are shown, there were a lot of performers. More than one hundred people were included in the study. Randomization of 4-6 weeks of basic therapy, arterial hypertension and coronary heart disease, which included thiazide diuretics, ACE inhibitors, beta-blockers, statins, antiplatelet agents, if necessary, indirect anticoagulants. Then randomization to either “Propanorm” or “Cordarone” for 12 months.
17:53
The randomization groups of either Propanorm or Cordarone were comparable. Approximately the same percentage of the degree of arterial hypertension, and the degree of heart failure, and the characteristics of atrial fibrillation.
Results. Preventive effectiveness of “Propanorm” and “Cordarone” after 6 and 12 months. The height of the columns is comparable, but statistically insignificantly different. Both drugs were effective.
Cancellation rate due to side effects, early dropout. In total, 26 patients were on Cordarone, 25.2% on Propafenone. The main side effect is prolongation of the QT interval and withdrawal due to the threat of a proarrhythmic effect.
Based on this study, conclusions were drawn. "Propafenone" is a class 1 antiarrhythmic that does not worsen hemodynamic parameters in patients with moderately severe heart failure and preserved left ventricular systolic function.
The antiarrhythmic effectiveness of Propafenon is not inferior to the antiarrhythmic effectiveness of Cordarone. Statistically insignificant difference.
Thus, in the absence of post-infarction cardiopathy with reduced ejection fraction, Propafenone can be used as an arrhythmic drug. It is advisable to use it in combination with beta blockers. This improves safety and increases efficiency. Finally, Propafenone is better tolerated compared to Cordarone.
This study shows the fundamental possibility of using class 1 drugs in patients with moderately severe organic disease, including coronary heart disease. I want to emphasize that we are talking about using moderate doses. This does not necessarily imply long-term, continuous use of drugs. Although in the study these drugs were given continuously.
20:11
In addition to what has been studied, beta-blockers and calcium channel blockers, in particular Verapamil, are used to prevent relapses. This has been proven. Calcium channel blockers (that is, Verapamil), ACE inhibitors are drugs that have a strong evidence base as actually acting, reducing the frequency of arrhythmia relapses.
Less studied groups of drugs that also have a certain evidence base in terms of effectiveness for preventing relapses. Angiotensin receptor antagonists, statins and Omega-3 polyunsaturated fatty acids in the form of the drug "Omakor".
This is a new direction, which today has its controversial aspects, but also a sufficient evidence base. It's the drug. Not food additives, not fish oil, but “Omacor” (as it’s called in Europe) and “Lovaza” (in the USA).
Ethyl esters: eicosapentaenoic and docosahexaenoic acid, collected in one capsule. With long-term course use, there is evidence that this drug enhances Antiari, Propatheon and other antiarrhythmics of various classes in the sense of preventing relapses of ventricular fibrillation. This drug is also captivating because it has virtually no side effects, that is, at the placebo level. Well tolerated.
These aspects are not generally accepted today (many of them are controversial), but I wanted to touch on them and highlight them.
Thank you for attention.
Indications and contraindications
The scope of application of beta blockers and ACE inhibitors is the same - hypertension and cardiac pathologies. The beta blocker Anaprilin and the ACE inhibitor Enalapril are prescribed for the following diseases:
- hypertonic disease;
- unstable angina;
sinus type tachycardia in hyperthyroidism;- ventricular tachycardia;
- ventricular and atrial fibrillation;
- extrasystole;
- essential type tremor;
- systemic atherosclerosis;
- abstinence of alcohol etiology;
- prevention of migraine pain;
- lipid imbalance;
- systolic hypertension in elderly patients.
Contraindications for use are:
- intolerance to the components of ACE inhibitors and beta blockers;
- history of Quincke's edema;
- porphyria;
- stenosis of the renal arteries and disorders in the kidney cells;
- azotemia;
- severe hypotension - systolic pressure less than 90;
- cardiogenic shock;
- stenosis of the aortic valve or aortic walls;
- pregnancy in a woman and lactation period;
- age up to 18 years.
Aortic valve stenosis
Use with caution in therapy for the following diseases:
- myocardial ischemia;
- cerebrovascular pathologies;
- liver and kidney failure;
- hemodialysis procedure;
- diabetes mellitus type 1 and 2;
- immunosuppressant therapy;
- old age after 65 years.
Children under 18 years of age are prohibited from taking medications because the risk of developing kidney pathologies and hypotension is high.
The use of medications during pregnancy is possible only when the therapeutic effect is much higher than the possible risk of harm to the fetus. Treatment should be carried out in a hospital setting, but the drugs must be discontinued 3 days before birth. Possible risks of impact on the fetus are growth retardation, intrauterine development of bradycardia, hypotension, hypoglycemia.
If there is an urgent need to prescribe drugs during lactation, then the newborn should be transferred to artificial feeding.
Instructions for use
Anaprilin tablets must be taken orally, without being tied to meals. The dosage of the drug is prescribed by the attending physician in accordance with blood pressure indicators, as well as instrumental diagnostics of heart function (ECG, EchoCG).
Standard dosages for taking Anaprilin for various pathologies:
- hypertension - a dose of 80 mg of propranolol, divided into 2 doses (morning dose and evening dose). If after 14 days of use there is no sustained decrease in the blood pressure index, then it is necessary to add another dose of the drug (40 mg), or a dosage regimen of 80 mg twice a day is allowed. The maximum permissible dosage per day is 320 mg;
Hypertonic disease - for cardiac pathologies - the initial dose is 20 mg 3 times a day, if necessary, the dosage is increased to 120 mg per day. The permissible dose of medication per day is 240 mg;
- for the prevention of migraine pain and for the treatment of tremor – 120-160 mg.
Enalapril is prescribed for the following diseases:
- renovascular hypertension - the initial dosage of enalapril per day is 5 mg. The maximum permissible dosage of medication per day is 20 mg. Most often, this dosage is prescribed twice a day (morning and evening);
- for cardiac failure, the initial dose is 2.5-5 mg. Over 7-10 days, the dosage is slowly increased and can reach 10-40 mg;
- in case of complex treatment with diuretics – 2.5 mg;
- in elderly patients, the dose of enalapril is from 1.25 to 2.5 mg.
Dosage forms of the drug
The medication is intended for oral administration and parenteral administration. Anaprilin is produced:
- In the form of white tablets: with a concentration of 10 and 40 mg of the active substance. Auxiliary and formative components of pills: talc, hypromellose, starch, MCC, silicon dioxide, calcium stearate. The packaging of the drug contains from 10 to 10 pieces, packaged in blisters.
- In the form of a water-based injection solution. A transparent liquid with a concentration of 0.1% is packaged in glass ampoules of 1 and 5 ml, packed in cardboard packs of 10 or 100 pcs. The drug with 25% of the active substance is available in a dosage of 1 ml. One package contains 10 ampoules.
The active ingredient of Anaprilin is propranolol hydrochloride. This compound has a pronounced hypotensive effect, dilates blood vessels, and prevents heart rhythm disturbances. Included in drugs for the treatment of angina attacks and other cardiac pathologies.
Main differences, effectiveness and safety
What is the difference between Enalapril and Anaprilin? The main difference between the two medications is that these medications belong to different groups of drugs, but both have a hypotensive effect. Enalapril is an ACE inhibitor, and Anaprilin is a beta blocker. Therefore, these medications have different mechanisms of action. Since they have different points of influence, medications lead to a decrease in the load on the myocardium and arterial membranes, which lowers blood pressure.
What is better to choose, Anaprilin or Enalapril? According to doctors' observations, Enalapril is more effective than Anaprilin in monotherapy, but in complex therapy with ACE inhibitors and beta blockers, the therapeutic effect is much higher, which makes it possible to reduce the dosage of medications and shorten the duration of the drug course by 2-3 times.
Side effects
ACE inhibitors and beta blockers are well tolerated by the body both as monotherapy and in combination. Possible side effects from taking both medications are the same and are presented in the table.
| Organ systems | Frequently occurring adverse reactions | Adverse reactions that occur infrequently | Rare side effects |
| Hemostatic system and lymph |
|
| |
| Metabolism |
|
|
|
| Nervous system and psyche |
|
|
|
| Blood circulation system and heart |
|
|
|
| Respiratory system |
|
|
|
| Digestive organs |
|
|
|
| Skin |
|
|
|
| Kidneys and urinary system |
|
| |
| Reproductive system |
|
|
Interaction of medications with other medications and analogues
To take medications, it is important to know their compatibility with other medications and the development of adverse reactions of the body to their use. Results of taking Enalapril and Anaprilin together with other medications:
- non-steroidal anti-inflammatory medications reduce the hypotensive effect of medications;
- hyperkalemia is provoked by taking diuretics, which conserve potassium in the body;
- analgesics and antibacterial medications reduce the hypotensive property;
- The effectiveness of medications is enhanced by the combined use of calcium antagonists and nitrates.
The most popular analogues of Enalapril with identical composition and active ingredients are:
- Swiss analogue of Renitek.
- Czech medicine Enarenal.
- Enap N, produced in Slovenia.
Popular analogues of Anaprilin are:
- Propranolol is a German-made medication that is prescribed for high blood pressure, various types of angina, and myocardial infarction.
- Sotahexal is a German analogue that is prescribed for high blood pressure, as well as cardiac pathologies of impaired conduction of impulses and heart rhythm.
For what diseases is Anaprilin indicated?
The drug is prescribed in the following cases:
- for chronic hypertension;
- coronary heart disease, angina pectoris;
- renal hypertension;
- arrhythmias provoked by rheumatic lesions of the heart muscle: sinus, parochymal, atrial fibrillation, extrasystole;
- as part of rehabilitation therapy: for myocardial infarction, intoxication with digitalis and other medications that disrupt the heart rhythm;
- in the complex treatment of thyrotoxicosis;
- with open-angle glaucoma;
- with essential tremor;
- for the prevention of migraines and cerebrovascular accidents.
With the exception of cases of poisoning with potent drugs, Anaprilin is recommended to be taken regularly. The therapeutic effect is achieved after the first dose and increases over time. By the end of the second week, a persistent hypotensive effect is observed.