© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
The patient cannot always independently interpret the medical terms read in the electrocardiogram protocol. Of course, only a doctor can decipher the cardiogram itself and the resulting conclusion, but what should you do before your appointment? First, decide on the terminology and try to understand for yourself whether your cardiogram is normal or not.
Causes of supraventricular extrasystole
The causes of supraventricular extrasystole are varied, among them the most common are heart diseases:
- The most common cardiac pathology leading to the development of extrasystole is coronary heart disease.
- Almost 95% of patients who have suffered a myocardial infarction are subsequently diagnosed with heart rhythm disturbances, including supraventricular extrasystole.
- Cardiomyopathies: arrhythmogenic, dilated, hypertrophic and restrictive.
- Inflammatory processes in the heart muscle (myocarditis).
- Chronic heart failure.
- Heart defect (congenital and acquired).
Other causes of supraventricular extrasystole are:
- Heart rhythm disturbances may occur while taking medications. Most often, the development of extrasystole is provoked by therapy with arrhythmic drugs, cardiac glycosides, and diuretics. Uncontrolled use of medications or very long treatment is especially dangerous.
- Electrolyte imbalances (magnesium, sodium, potassium).
- Exposure to toxins on the body (smoking, drinking alcohol, drugs).
- Malfunctions of the autonomic nervous system.
- Diseases associated with hormonal disorders (diabetes mellitus, adrenal pathologies, thyrotoxicosis).
- Chronic oxygen starvation of the body. This condition is often observed with sleep apnea, chronic bronchitis, and anemia.
Sometimes the nature of supraventricular extrasystole remains unclear, in which case they speak of an idiopathic heart rhythm disorder.
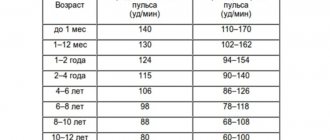
Normal heart rate
heart function is normal - in sinus rhythm
The concept of normosystole usually also refers to the fact that electrical signals that contribute to the sequential electrical excitation of all parts of the heart are generated in the sinus node, which is normally the first-order pacemaker. In all other cases, they speak of pacemaker migration or non-sinus rhythm. These processes are united by the concept of heart rhythm disturbances, or arrhythmias.
Therefore, usually in the ECG conclusion, in addition to the characteristics of the heart rate (HR), in the first place there is a mention of whether the patient has sinus rhythm or not. If the patient sees the term “normosystole” in the protocol, then most likely this means that he has not only a correct, normal heart rhythm, but also a sinus rhythm - that is, it comes from the sinus node, as it should be normally. (Nevertheless, there are formulations of “normosystole” with an even heart rate, but non-sinus rhythm - more on this at the end of the article).
Who has it?
Supraventricular extrasystole (SE) occurs in 60-70% of people . Normally, it can also occur in clinically healthy patients.
The presence of supraventricular extrasystole (SVES)
does not mean that a person is sick.
SE is more often registered in adults and older children , since young children are not yet able to describe their sensations and do not really understand what is happening to them.
In newborns and young children, supraventricular extrasystole is detected during an ECG during medical examination, general examination, or in connection with an alleged disturbance in the functioning of the heart (congenital defects, a sharp deterioration in the child’s condition in the absence of external factors).
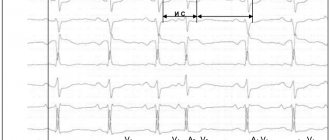
Normosystole with atrial fibrillation
Of all rhythm disturbances, only this type of arrhythmia, such as fibrillation or atrial flutter, is divided into normo-, tachy- and bradysystolic variants. In this case, the diagnosis “atrial fibrillation, normosystole” indicates a pathology in the form of arrhythmia, but with a normal final heart rate.
normosystolic form of atrial fibrillation - despite the “waves” of atrial flutter/fibrillation, contraction of the ventricles of the heart occurs at a normal frequency
In this case, we are talking about both a permanent form of atrial fibrillation, when a person lives for a long time (months and years) with an irregular or non-sinus rhythm, and a paroxysmal form (paroxysm - attack), when a non-sinus rhythm occurs suddenly and may well recover spontaneously or with the help of medications. Diagnostic criteria are similar to those for normo-, brady- and tachysystole in sinus rhythm - from 60 to 80, less than 60 and more than 80 beats per minute, respectively.
With a permanent form of atrial fibrillation, normosystole is usually more easily tolerated by patients in terms of the sensation of interruptions in the work of the heart, since bradysystole is fraught with a decrease in cardiac output and resulting fainting, and the heart rate during tachysystole sometimes reaches 200 beats per minute, which can lead to severe circulatory disorders.
Diagnostics and its methods
Most often, the primary diagnosis is an electrocardiogram. Most often, extrasystole is detected during a medical examination and requires a more thorough study of the heart.
Sometimes, if the patient already has symptoms of some kind of heart problems after physical activity, then diagnostic procedures are used that measure the heart rate after physical activity.
In addition to these methods, there is also a classic examination by a doctor, where he measures the patient’s pulse and listens to the work of the heart.
- Why ventricular extrasystole occurs, symptoms and treatment of pathology
Common deviations from the norm (brady- and tachysystole)
Sometimes the ECG conclusion may include a combination of normosystole and irregular sinus rhythm - “normosystole, irregular rhythm.” The latter can occur, for example, with respiratory or sinus arrhythmia. In this case, the rhythm comes from the sinus node (as it should be normally), but there are minor functional fluctuations in the heart rate due to the phases of inhalation and exhalation (normally, when inhaling, the heartbeat speeds up slightly, and when exhaling, it slows down slightly). Therefore, if a patient sees a conclusion about normosystole with an irregular but sinus rhythm, there is no point in panicking.
When a patient experiences an increase or decrease in heart rate, the doctor describes this as tachycardia or bradycardia. But sometimes he may write about tachysystole or bradysystole, which literally means frequent or rare heartbeats, respectively. In this context (assuming sinus ri and “systole” are synonymous.
Again, tachysystole and bradysystole can occur both in a completely healthy person and in various diseases of the heart or other organs. Here everything depends on other nuances obtained from the ECG. But if a person has a sinus rhythm with a slightly slow heart rate (at least 50 per minute) or increased heart rate (90-100) - especially from excitement, then we can talk about normal indicators.
What is supraventricular extrasystole?
Extrasystole is the general concept of extraordinary (arrhythmic) heart contractions. According to localization they are divided into the following types:
- supraventricular extrasystole (supraventricular);
- ventricular extrasystole (ventricular);
- antiventricular extrasystole (atrioventricular).
The foci of supraventricular extrasystoles are located in the atria, that is, above the ventricles. Hence the name arrhythmia. The atrioventricular form is characterized by the appearance of ectopic (arising in the wrong place) contractions in the septum between the atrium and the ventricle or between the ventricles. Ventricular extrasystole is localized in the ventricles. The consequence of supraventricular and ventricular extrasystoles is often changes in the muscle tissue of the heart (myocardium).
Classification of atrial extrasystole is made according to many parameters. By number of pulses per minute:
- single (number of unscheduled layoffs 1 – 5);
- paired (two pulses in a minimum period);
- group (several reductions per period);
- multiple (over 5 extraordinary impulses).
Based on the number of sources of impulse generation, they are distinguished between monotypic (one source) and polytopic (more than one source of excitation). If there is a certain pattern in the passage of normal contractions and extraordinary ones, then they speak of organized extrasystole. If this alternation is chaotic, then it is called disorganized. Division by etiology (origin) of arrhythmia:
- organic extrasystole is caused by pathological changes in the heart, which in particular includes sinus extrasystole;
- functional, resulting from other disorders in the body.
Extrasystole on ECG
Extrasystole leads to the fact that the heart cannot fully contract. And this in turn can cause supraventricular tachycardia and fibrillation.
Characteristic signs
If the arrhythmic state is not a consequence of a tense psycho-emotional state and indicates the presence of a specific illness, then it has a number of symptoms. Superventricular and ventricular extrasystole manifest themselves as follows:
- shortness of breath appears and it seems that there is a catastrophic lack of air;
- dizzy;
- the body suddenly weakens;
- sweat is released intensely;
- a person is overcome by panic and a feeling of discomfort;
- a strong feeling of extraordinary blows of a sharp nature;
- “throws me into a fever” for no apparent reason.
Important! Doctors emphasize that it is important not to ignore the feeling of cardiac arrest. It is because of this that panic begins, anxious feelings appear, the patient is afraid of something and suddenly turns pale.
The main danger of extrasystole is that it may not appear for a long time, but at the same time actively develop, thereby increasing the risk of additional heart diseases. For this reason, at the slightest sign you should immediately contact a cardiologist, even if it is a single extrasystole. The doctor will be able to confirm or refute the diagnosis and, if necessary, prescribe the correct treatment.
Prognosis, complications and consequences
According to some experts, frequent supraventricular extrasystole after a few years can lead to the development of heart failure, atrial fibrillation and cause a change in the configuration of the atria.
The prognosis for SE is favorable. This disease does not lead to sudden death, unlike ventricular extrasystole in combination with organic heart damage.
- Extrasystole - what is it, causes and methods of treatment
What do you need to know about treatment?
Diagnosis is carried out on the basis of patient complaints and the results of an examination, during which auscultation of the pulse is performed. Information about the patient’s lifestyle, heredity, previous diseases, and bad habits is also important. Laboratory tests include general and biochemical blood tests, as well as urine tests to determine hormone levels. Instrumental diagnostics:
- ECG;
- EFI;
- Holter monitoring;
- ultrasonography;
- load tests.
Treatment of superventicular arrhythmia has two directions: conservative and surgical. Moreover, if the disease does not interfere with normal life in any way, no medications or surgeries are prescribed. Regular examinations are sufficient to exclude complications.
Before prescribing a medicine, the doctor determines whether it is appropriate. Sometimes treating rare attacks of extrasystole with antiarrhythmic drugs can be dangerous, because this group of drugs has many side effects. Otherwise, drugs are still prescribed. They can help normalize the functioning of the heart muscle, thereby reducing stress. Drugs that control blood pressure levels are often used in treatment.
When drug therapy is powerless, one type of surgical intervention is prescribed. This may be open surgery or radiofrequency catheter ablation. Any procedure is carried out only as prescribed by the attending physician and under conditions of strict monitoring of the patient’s current condition. Those people who seek medical help on time have a chance for a full recovery.
Diagnostics
To confirm the diagnosis and clarify the severity of the disease, additional diagnostic methods are needed:
- taking an electrocardiogram (ECG) at rest and during the next attack of arrhythmia
- 24/7 ECG recording is performed (Holter ECG monitoring)
- according to indications, further examination is required to exclude the symptomatic nature of arrhythmic syndrome
- according to indications, it is possible to conduct an endocardial electrophysiological study of the heart in a hospital setting