SVC syndrome is a congenital anomaly of the development of cardiac structures, in which an extra conductive bundle is formed in the heart, transporting an electrical impulse from the sinus node to the ventricles, bypassing the atrioventricular node, which leads to premature excitation of the ventricles.
By its nature, this is a vice, but it is not immediately revealed. Symptoms in the early stages are minimal. As a rule, the detection of such a phenomenon is an accident detected during electrocardiography. The signs are quite characteristic, so it is almost impossible to confuse the condition.
The disease is also called Wolff-Parkinson-White syndrome, named after the most prominent researchers.
Treatment of the condition has certain prospects at any stage. They are best at the time of detection, when there are no organic defects yet.
The mechanism of pathology development
The essence of the deviation is the formation of an extra pathway in the heart.
This is the normal state of affairs. Cardiac structures have the ability to contract and work autonomously due to the presence of a cluster of active cells that generate an electrical impulse.
This is the so-called sinus node or natural pacemaker. He works constantly. The so-called bundles of His are responsible for conducting signals; they have a branched structure and end at the level of the ventricles.
Against the background of SVC syndrome (Wolf-Parkinson-White), an additional path of impulse movement along the Kent bundle is formed.
Hence the increased activity of cardiac activity, which manifests itself both as tachycardia (contractions that go through a full cycle, however, do not always occur) and other types of arrhythmias (from fibrillation to extrasystole). It all depends on the characteristics of the development of the disease in a particular person.
As the problem progresses, disruptions in the normal functioning of all organs and systems are observed. The heart suffers first, then the blood vessels. Brain, kidneys and liver.
Some relatively mild forms are asymptomatic. Others give a pronounced clinical picture and are associated with an increased risk of sudden death of the patient in the short term.
Forecast
Once WPW syndrome is identified and properly treated, the prognosis is favorable.
Asymptomatic patients with only ventricular pre-excitation on the ECG usually have a very good prognosis. Many develop symptomatic arrhythmia over time, which can be prevented with prophylactic EPS and radiofrequency catheter ablation. Patients with a family history of sudden cardiac death (SCD) or significant symptoms of tachyarrhythmia or cardiac arrest have a worse prognosis. However, after definitive therapy, including curative ablation, the prognosis becomes good again.
Classification
Typifications are mainly topographical in nature. That is, they determine where the excess conducting structure comes from, in which direction it extends and how it interacts with surrounding tissues.
In total there are about 10 varieties, delimited on this basis. This diversity determines the heterogeneity of possible course options and pathological manifestations, as well as prognosis.
For the patient, these classifications are not of great importance, since it is impossible to understand their clinical meaning without special cardiological training, and explanations would take a lot of time.
A large role is given to determining the course of the pathological process.
For this reason it is called:
- Manifesting type. Occurs spontaneously. An episode can be triggered by excessive physical activity, nervous tension, momentary or long-term, consumption of caffeine, tobacco, and psychoactive substances. The type is determined by severe tachycardia; arrhythmic components are possible, but they are relatively rare. The frequency of relapses varies: from several times a year to dozens of cases within one month.
- Intermittent (transient) type. It is determined by similar clinical signs, but they manifest themselves with less force. In addition, arrhythmia occurs more often and is more pronounced, which makes this form more dangerous than the previous one.
- Latent type. He's hidden. There are no symptoms at all, the problem is detected on electrocardiography. Is there a difference in this case between the phenomenon of SVC and the syndrome? Without a doubt. The disease in this form, although it does not make itself felt, continues to progress and destroy the body. The process can take years. Only at the moment when the compensatory mechanisms can no longer cope will the pathology appear.
Another, understandable way to typify the process is based on the localization of the anomalous beam.
Accordingly, there are two types:
- A. Located between the left atrium and ventricle. Normally, the impulse to the latter passes from the sinus through the atrioventricular node. In type A, the signal reaches the anatomical structure earlier, but then the stimulation is duplicated along the normal path, which leads to excess activity. Hence the disturbance of hemodynamics and blood circulation in a large circle.
- B. Localization - between the right atrium and ventricle. The mechanism is identical, but since the right structure contracts, the pulmonary system suffers first.
Clinically, the most severe variant is mixed, when several branches are present. This is an AB type. Treatment is carried out urgently.
Medical reference books
Pre-excitation syndrome
ICD-10: I45.6
Introduction
In 1930, L. Wolff, J. Parkinson and PD White published an article describing 11 patients who suffered attacks of tachycardia, and during sinus rhythm had a short PR interval and a wide QRS complex on the ECG, reminiscent of bundle branch block. After these authors, the syndrome they described was called Wolff-Parkinson-White (WPW) syndrome. WPW syndrome is one of the variants of “pre-excitation” of the ventricles. As defined by Durrer et al. (1970), the term “preexcitation” of the ventricles means that the ventricular myocardium is activated by the atrial impulse earlier than would be expected if the impulse entered the ventricles through the normal specialized conduction system. WPW syndrome is more common than other types of ventricular preexcitation. It is based on a congenital anomaly in the structure of the conduction system of the heart in the form of an additional bundle of Kent, connecting the myocardium of the atria and ventricles directly, bypassing the atrioventricular junction, and capable of rapidly conducting impulses. The conduction anomaly in WPW syndrome is manifested by characteristic ECG changes and a tendency to develop supraventricular tachycardias.
Pathophysiology
The bundles of Kent are formed in the embryonic period in the form of muscle bridges passing through the fibrous ring between the atria and ventricles. The electrophysiological characteristics of the Kent bundles (conduction velocity, refractoriness) differ from the properties of the atrioventricular connection, which creates the prerequisites for the development of arrhythmias through the mechanism of re-entry of the excitation wave (re-entry). The ability of the Kent bundles to rapidly conduct atrial impulses bypassing the atrioventricular junction determines the possibility of an unusually high heart rate during the development of atrial fibrillation/flutter, which in rare cases can cause ventricular fibrillation and sudden death.
Epidemiology
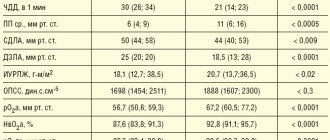
· Ventricular preexcitation occurs in the general population with a frequency of 0.1-0.3%. 60-70% of patients have no other signs of heart disease. · WPW syndrome is more common in men than in women. · The age of patients may vary. Typically, WPW syndrome is detected in childhood or adolescence when seeking emergency care for tachyarrhythmias. The speed of conduction along accessory pathways decreases with age. Cases have been described in which ECG signs of preexcitation completely disappeared over time. · Up to 80% of patients with WPW syndrome experience reciprocal (circular) tachycardia, 15-30% have atrial fibrillation, 5% have atrial flutter. Ventricular tachycardia is rare.\
Mortality
The risk of sudden arrhythmic death in patients with WPW syndrome is very low - about 0.15-0.39% over a follow-up period of 3 to 10 years. Sudden death as the first manifestation of the disease is relatively rare. On the contrary, in 1/2 of people with WPW syndrome who died suddenly, the cause of death was the first episode of tachyarrhythmia. The risk of sudden death increases when certain drugs (digoxin) are used to treat arrhythmias.
Clinical picture
History · Paroxysmal tachycardias in WPW syndrome often occur in childhood, but may first develop in adults. Having begun in childhood, arrhythmia can disappear for a while, then it recurs. If attacks of tachycardia have not stopped after the age of 5 years, the probability of their continuation in the future is 75%. · During an attack of tachycardia, various symptoms are possible - from minor discomfort in the chest, palpitations, dizziness to lightheadedness or loss of consciousness, severe hemodynamic disturbances and cardiac arrest. · Syncope can occur as a result of cerebral hypoperfusion against the background of tachyarrhythmia, or as a result of depression of the sinus node during tachyarrhythmia with the development of asystole after its cessation. · After the end of the paroxysm, polyuria may be observed (stretching of the atria during an attack leads to the release of atrial natriuretic peptide). · Signs of ventricular preexcitation can be detected by random ECG recording in individuals without rhythm disturbances (WPW phenomenon). · Asymptomatic patients rarely become symptomatic after age 40. With increasing age, there is a possibility of developing fibrosis in the area of attachment of the bundle, and therefore it loses the ability to conduct impulses from the atria to the ventricles. Physical findings WPW syndrome has no characteristic physical findings other than those associated with tachyarrhythmias. In young people, symptoms may be minimal even with a high heart rate. In other cases, during an attack there is coldness of the extremities, sweating, hypotension, and signs of congestion in the lungs may appear, especially with concomitant heart defects - congenital or acquired.
Diagnostics
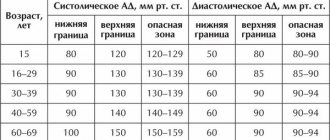
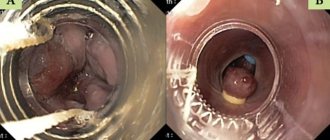
1. Standard ECG WPW syndrome is characterized by the following ECG changes (
): · Short interval pQ < 0.12 s. - the result of accelerated entry of the impulse into the ventricles along the accessory pathway. · Delta wave – a gentle slope in the initial part of the QRS complex (the first 30-50 ms). - reflects the initial excitation of the ventricle through the accessory pathway, which runs away from the specialized conduction system and gives rise to a relatively slow transmission of impulse from fiber to fiber of the myocardium.
· Wide QRS complex > 0.10-0.12 s. - the result of excitation of the ventricles from two directions - leading through the accessory pathway, and immediately following this - through the AV connection. · Secondary changes in repolarization - the ST segment and T wave are usually directed in the direction opposite to the orientation of the delta wave and the QRS complex. Analysis of the polarity of the delta wave in various ECG leads allows us to determine the localization of the accessory pathway. An additional pathway can be manifest or hidden. — Manifest path - the ECG shows the above signs of pre-excitation, the bundle is capable of antegrade impulse conduction (from the atria to the ventricles). — Hidden path - there are no signs of pre-excitation on the ECG (the bundle conducts impulses only in the retrograde direction, from the ventricles to the atria, being the retrograde part of the re-entry circle in orthodromic tachycardia). In some patients, preexcitation may be intermittent (not constant), with a variable ECG pattern in the complexes of one recording or on cardiograms taken several days and even hours apart ().
2. Daily Holter ECG monitoring Allows you to record arrhythmias and detect intermittent ventricular preexcitation.
3. Echocardiography Allows you to evaluate the function of the left ventricle, myocardial contractility in various segments, exclude concomitant heart defects - valve defects, Ebstein's anomaly, corrected transposition of the great vessels, ventricular and atrial septal defects, hypertrophic cardiomyopathy, which can be combined with WPW syndrome.
4. Electrophysiological study (EPS) When examining some patients, a special electrophysiological study may be necessary. EPS can be non-invasive (method of transesophageal electrical stimulation of the heart - TEES) and invasive, endocardial. The last method is the most accurate. EPI allows you to clarify the mechanism of development of tachycardia, determine the localization of the accessory pathway and evaluate its electrophysiological properties (conductivity and duration of the refractory period). Beams with a short refractory period (less than 250-270 ms), and therefore capable of conducting pulses at high frequencies, are potentially dangerous.
Arrhythmias in WPW syndrome
In patients with WPW syndrome, various rhythm disturbances may occur, but the most common are 2 types of tachycardia: reciprocal (circular) tachycardia and atrial fibrillation/flutter.
1. Reciprocal atrioventricular tachycardia: orthodromic, antidromic · In sinus rhythm, impulses from the atria to the ventricles are carried out through both pathways - the atrioventricular connection and the bundle of Kent; there are no conditions for paroxysm of tachycardia. The triggering factor for circular tachycardia is usually an atrial extrasystole, which occurs at a critical moment in the cardiac cycle, namely when a premature impulse can be carried to the ventricles through only one path, due to the refractoriness of the second. · Most often, the Kent bundle is refractory (90-95% of cases), and the ventricles are excited through the atrioventricular connection (orthodromic). After the end of ventricular excitation, the impulse can return to the atria along the accessory pathway, moving in a retrograde direction, and re-enter the atrioventricular junction, closing the circle of tachycardia. With this direction of impulse movement, the tachycardia is called orthodromic reciprocal AV tachycardia. Its features: 1) narrow QRS complex; 2) strict regularity of rhythm; 3) signs of retrograde excitation of the atria behind the QRS complex (P wave - negative polarity in leads II, III and avF) (
).
· Attacks of orthodromic tachycardia can also be observed in patients with hidden bundles of Kent, due to the ability of the accessory pathway to conduct retrogradely. · Antidromic reciprocal AV tachycardia occurs 10-15 times less frequently than orthodromic tachycardia. In this case, the impulse enters the ventricle through the accessory pathway (antidromically) and returns to the atrium through the atrioventricular junction in a retrograde direction. Tachycardia is formed 1) with wide QRS complexes, 2) strictly regular, with a potentially higher rhythm frequency, since the beam has a short refractory period, 3) the retrograde P wave is located in front of the QRS complex, but is usually poorly distinguishable. The ventricular complex in this case represents a continuous delta wave, coinciding in polarity in each lead with the delta wave in sinus rhythm. Such tachycardia is difficult to distinguish from ventricular (
). If the diagnosis is in doubt, this form of supraventricular arrhythmia should be treated as ventricular arrhythmia. · Antidromic tachycardia is more dangerous than orthodromic tachycardia: it is less tolerated and more often transforms into ventricular fibrillation.
2. Atrial fibrillation · Atrial fibrillation occurs in patients with WPW syndrome much more often than in people of the same age in the general population - with a frequency of 11-38%. The predisposition to the development of atrial fibrillation in WPW syndrome is explained by changes in the electrophysiological properties of the atria under the influence of frequent paroxysms of circular tachycardia, and even by the very fact of attachment of the bundle to the atrial myocardium. It is also believed that atrial fibrillation may occur as a result of changes in the atria that accompany WPW syndrome, independent of the presence of the accessory pathway. · Atrial fibrillation is the most dangerous arrhythmia in WPW syndrome, which can degenerate into ventricular fibrillation. The appearance of paroxysms of atrial fibrillation in a patient with WPW syndrome means an unfavorable turn in the course of the disease. The time of onset of atrial fibrillation may vary: it may be the first attack of tachycardia in a patient with WPW syndrome, occur in patients with a long history of reentrant tachycardia, or develop during an attack of reentrant tachycardia. · Normally, the atrioventricular connection acts as a physiological filter on the path of frequent impulses from the atria, passing no more than 200 impulses per minute during atrial fibrillation into the ventricles. In patients with WPW syndrome, impulses flow from the atria to the ventricles using both the AV junction and the bundle of Kent. Due to the short refractory period and the high speed of conduction along the accessory pathway, the number of heart contractions can reach 250-300 or more per minute. In this regard, AF in WPW syndrome is often accompanied by hemodynamic impairment, which is clinically manifested by hypotension and syncope. · Impaired hemodynamics during a paroxysm of AF causes sympathetic activation, which further increases the frequency of conduction along the accessory pathway. Too high a heart rate can cause atrial fibrillation to transform into ventricular fibrillation. · On the ECG during atrial fibrillation in patients with ventricular preexcitation, a frequent irregular rhythm (heart rate more than 200/min) with wide polymorphic QRS complexes of unusual shape is recorded. The originality of the ventricular complexes in this arrhythmia is associated with their confluent nature (the shape of the QRS is determined by the relative participation of the AV junction and the accessory pathway in the excitation of the ventricles). Unlike polymorphic ventricular tachycardia, there is no “torsades de pointes” phenomenon (
).
· Measurement of the shortest RR interval on an ECG taken during an attack of atrial fibrillation in a patient with WPW syndrome is used to assess the degree of risk: the danger is maximum if RRmin ≤ 220-250 ms.
Risk stratification
The optimal treatment strategy for WPW syndrome is determined based on an individual assessment of the risk of sudden death. · Persons with signs of pre-excitation on the ECG who have not suffered tachycardia usually do not require either treatment or additional examination. The exception is professional athletes and representatives of high-risk professions (pilots, drivers, etc.): they are recommended to undergo an electrophysiological examination to determine the properties of the accessory pathway and the associated risk of sudden death. · The intermittent nature of ventricular preexcitation, the disappearance of the delta wave against the background of increased rhythm or during physical activity, as well as after intravenous administration of procainamide or ajmaline, are characteristic of accessory pathways with a long refractory period. Such accessory pathways are usually not capable of conducting impulses frequently if atrial fibrillation/flutter develops. The risk of sudden cardiac death is low. · High-risk markers for WPW syndrome, established in a retrospective analysis of cases of sudden death of patients: 1) the shortest RR interval for atrial fibrillation less than 250 ms; 2) history of symptomatic tachyarrhythmias; 3) multiple accessory pathways; 4) Ebstein's anomaly; 5) familial form of WPW syndrome, cases of sudden death in the family history. · The risk of sudden death can be assessed most accurately by intracardial EPI.
Treatment
Patients with WPW syndrome require treatment during paroxysms of tachycardia and to prevent relapses.
Relief of tachycardias 1. Orthodromic reciprocal tachycardia (narrow QRS complex, frequency - about 200/min, retrograde P is clearly visible behind the QRS complex): treatment is aimed at slowing down conduction in the AV node. · Vagal techniques (performing the Valsalva maneuver, unilateral carotid sinus massage, immersing the face in cold water, applying an ice pack to the face) are more effective at the onset of an attack. · ATP or adenosine intravenously (ATP for adults in a dose of 10-40 mg in the form of a bolus, intravenously quickly, over 3-5 seconds; adenosine 37.5 mcg/kg, intravenously quickly, if necessary - after 2-3 min at double dose – 75 mcg/kg). - do not use for sick sinus syndrome, bronchial asthma, vasospastic angina; — effective in 90% of cases of reciprocal tachycardia with a narrow QRS complex; ineffectiveness is usually associated with inadequate administration technique (rapid bolus administration is necessary due to the short half-life of the drug); - There should be a readiness to carry out defibrillation in the event of the development of another form of tachycardia (especially atrial fibrillation) after the administration of adenosine. · Verapamil intravenously (5 mg IV over 2 minutes, if the arrhythmia persists, repeat after 5 minutes at the same dose to a total dose of 15 mg). - used if tachycardia recurs, or ATP/adenosine is ineffective, or if the patient is taking theophylline; — verapamil is not used for WPW syndrome if the patient has already had episodes of atrial fibrillation.
2. Atrial fibrillation/flutter, antidromic reentrant tachycardia are tachycardias with ventricular preexcitation (wide QRS complex). They often occur with a high heart rate, severe symptoms, hemodynamic disturbances, and, therefore, require immediate cessation. In an urgent situation with unstable hemodynamics, electrical cardioversion is indicated (1st shock energy - 100 joules). If tachycardia is well tolerated, or electrical cardioversion is ineffective, drug therapy is performed. For the treatment of this group of arrhythmias, drugs that lengthen the refractory period of the accessory pathway (procainamide, cordarone) are indicated. Blocking the accessory pathway eliminates ventricular preexcitation, and with it the threat of sudden arrhythmic death. · Novocainamide – in patients without structural myocardial damage (intravenous infusion at a rate of 20 mg per minute until tachycardia is stopped; administration of the drug is stopped when hypotension develops, the QRS width increases by 50% of the original, or when the maximum dose of 17 mg/kg is reached). · Amiodarone – in patients with structural heart disease (loading dose – 5 mg/kg in a 5% glucose solution, IV drip over 20 minutes, then continue administration at a dose of 600-900 mg over 24 hours). NB: Digoxin, verapamil and beta blockers should not be used to treat atrial fibrillation/flutter in patients with WPW syndrome. By slowing down conduction through the atrioventricular junction, these drugs increase the conduction of impulses along the accessory pathway, heart rate and contribute to the transition of arrhythmia to ventricular fibrillation. NB: Lidocaine is also not used in this situation, since it does not prolong the refractory period of the accessory pathway. In patients with ventricular preexcitation, lidocaine may increase the rate of ventricular responses in atrial fibrillation.
Prevention
There are fundamentally two ways to prevent repeated episodes of arrhythmia in patients with WPW syndrome: pharmacological and non-pharmacological. The first approach involves long-term use of antiarrhythmic drugs. For a number of reasons, this route is not optimal: 1) arrhythmias in WPW syndrome are characterized by a high rate of rhythm and are associated with a potential threat to life, while the response to drug therapy is variable and unpredictable; 2) some drugs can paradoxically increase the frequency of paroxysms or the rhythm during episodes of tachycardia; 3) WPW syndrome often occurs in children and young people, in whom long-term use of antiarrhythmics is especially undesirable; 4) one cannot ignore the risk of developing systemic side effects, for example, thyroid dysfunction, photosensitivity or lung damage when taking amiodarone. · If drug therapy is necessary, preference is given to class ІC and III drugs that can block conduction along the accessory pathway (in international recommendations - propafenone and flecainide (IC), sotalol and amiodarone (III); recommendations of Russian authors also include etacizine (IC) and gilurythmal (IA)). Evaluation of the effectiveness of amiodarone in the treatment of patients suffering from tachycardias involving the accessory pathway did not show any advantages compared with class IC drugs and sotalol. These data, as well as the risk of systemic side effects, limit the long-term use of amiodarone in WPW syndrome to prevent paroxysmal tachycardias. The exception is patients with WPW syndrome and structural heart disease.
- Propafenone – 600-900 mg/day per day in 3 divided doses.
- Sotalol – 80-160 (maximum – 240) mg 2 times a day.
- Etatsizin – 25-50 mg 3 times a day.
Amiodarone - after reaching a saturating dose of 10-12 g - 200 mg 1 time per day, daily or with a break 2 days a week.
· Long-term use of beta blockers in WPW syndrome is acceptable, especially if, according to EPI, the accessory pathway is not capable of rapid completion. · Verapamil, diltiazem and digoxin should not be prescribed to patients with ventricular preexcitation, due to the risk of increased ventricular responses if atrial fibrillation develops.
The second way, non-drug, is associated with the destruction of the accessory pathway, either using a catheter (usually by electrical radiofrequency ablation - RFA), or surgically during open-heart surgery. Currently, RFA is becoming the first-line treatment for symptomatic patients with WPW syndrome, gradually replacing both medical and surgical approaches. The effectiveness of initial ablation of the accessory pathway reaches 95%, although in 5% of cases the arrhythmia may recur after elimination of inflammation and edema in the damaged area. In such cases, the accessory tract is usually successfully destroyed when the procedure is repeated. Catheter ablation can sometimes cause complications, and in rare cases, death (0 to 0.2%).
Indications for RFA · Symptomatic reciprocal atrioventricular tachycardia. · Atrial fibrillation (or other symptomatic atrial tachyarrhythmias) with a high frequency of conduction along the accessory pathway. · Asymptomatic patients with ventricular pre-excitation (WPW phenomenon), if the safety of the patient and those around him (pilots, deep-sea divers, etc.) may depend on their professional activities during the spontaneous development of tachycardia. · Family history of sudden death. Thus, for the treatment of patients with WPW syndrome (ECG signs of pre-excitation and symptomatic arrhythmias), especially with hemodynamic instability during arrhythmia paroxysms, RFA of the accessory pathway is the method of choice. In patients with hidden accessory pathways (without pre-excitation on the ECG), with rare low-symtom attacks of tachycardia, the risk is low; the treatment approach may be more conservative and take into account the patient's preferences.
Patient education Patients with WPW syndrome should be informed about the causes of the disease and its possible manifestations. This is especially important for young asymptomatic individuals, in case of detection of ventricular preexcitation for the first time during random ECG recording (WPW phenomenon). It is necessary to recommend that the patient undergo dynamic monitoring with mandatory consultation with a doctor if symptoms appear. It is advisable that a patient with ventricular preexcitation always have an ECG with him with a conclusion. Patients receiving drug therapy should know what medications they are taking. When counseling a patient with WPW syndrome, you need to explain the following: · How to recognize the manifestations of the disease. · How to apply vagal techniques, if necessary. · What may be the side effects of antiarrhythmic drugs if the patient takes them. · The advisability of refusing to engage in competitive sports. · Possibilities of RFA in the treatment of WPW syndrome and indications for its implementation, if any appear in the future. Relatives of a patient with WPW syndrome should be recommended a screening examination to exclude ventricular preexcitation.
What is the difference between the syndrome and the SVC phenomenon?
Essentially these are synonyms. There is only one difference. The wpw phenomenon is spoken of when the patient does not make any complaints about his own health.
The anomaly is discovered incidentally (by chance) during diagnosis for third-party diseases. Occurs in 30-50% of the population in a depressed state. Cardiac structures and the body in general adapt. This does not affect life expectancy in any way.
Regarding the disease. WPW syndrome is a clinically significant entity. But it also occurs in different ways, which gives a good chance of cure and prognosis. The intensity of the clinical picture in the early stages is minimal, progression is slow, and there is time for a full diagnosis and treatment.
Thus, the WPW phenomenon is a clinical finding on the ECG. Patients with deviations need to be looked at carefully. In the absence of symptoms for at least 2-4 months, a person can be considered conditionally healthy. The syndrome determines the need for planned treatment. In the event of an emergency, it is urgent.
Prevention of WPW syndrome
There is no specific prevention of the disease. If an ECG reveals a patient with SVC syndrome, he should be regularly examined by a cardiologist (even if the symptoms do not bother him). If signs of pathology appear, you need to immediately choose the right treatment.
Persons who are related to a patient with WPW syndrome are recommended to undergo a routine examination to exclude the development of this pathology in themselves. Diagnostics should include: daily monitoring of the electrocardiogram, electrocardiogram, electrophysiological methods.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Causes
The main proven factor in the development of the pathological process is a congenital anomaly. Normally, the heart and the entire blood supply system are formed at 3 weeks of pregnancy. Certain factors lead to deviations in the normal formation of the fetus and provoke congenital defects.
It is quite possible that SVC syndrome will not be the only one in the baby’s history. But such a point does not explain the reasons that determine the very possibility of a defect at such an early stage.
Interesting:
An extra vascular bundle develops in everyone, without exception, but by the end of the first trimester it resolves and everything returns to normal.
The immediate factors in the development of the pathogenic phenomenon are:
- Genetic mutations. They can be spontaneous, that is, determined without connection with chromosomal defects of the parents. This is a relatively rare clinical variety. Another option is inheriting certain genes from ancestors. There is a dominant or recessive type - it doesn’t play a big role. It’s just that in this case the likelihood of developing pathology is lower; on the other hand, all known diseases of this kind are much more severe. Often not only cardiac defects are detected, but also generalized problems.
- Stress during pregnancy. Have great clinical significance. The expectant mother should avoid psycho-emotional overload during pregnancy. This does not guarantee the absence of pathologies, but the risks are minimized. At times of stress, large amounts of corticosteroids and catecholamines are released into the blood. Such a reaction is a natural mechanism to negative environmental factors that ensure survival. Compounds like cortisol, norepinephrine and others increase muscle tone, blood pressure, and have some toxic effects when it comes to the development of the child.
- Excessive physical activity. A woman in labor should not sit in one place, but in everything she needs to know when to stop. Abnormal activity will have the same effect as stress, if not more. Spontaneous termination of pregnancy is possible as a result.
- Consumption of tobacco products, alcohol, especially drugs during gestation. Negligent “parents” think little about the health of their own offspring or indulge in addictions and weaknesses due to the difficulty of refusal and fear of withdrawal syndrome. This is a fundamentally wrong practice that has a detrimental effect on the fetus. Whether the child will be born healthy or not - in this case, even the best doctor cannot say.
- Poor quality food and water. It is difficult to determine exactly what role this factor plays. However, a negative effect on the fetus of carcinogenic substances that fast food isolates, so-called “harmful” food, such as fried foods, smoked foods, canned food and dubious semi-finished products. The same way the lack of vitamins and minerals affects a monotonous diet. The menu needs to be adjusted to suit the interests of the unborn child. A nutritionist will help with this.
- Negative environmental factors, including excess ionizing radiation in the area of residence. The body can adapt to the increased background radiation, but later this moment will most likely affect the child’s health. Negative phenomena include air pollution, excess metal salts in drinking water, sun activity and the level of ultraviolet radiation.
- History of somatic diseases. Especially hormonal profile. They not only aggravate the course of pregnancy, sometimes making it unbearable, but also affect the fetus. Treatment is ideally carried out at the stage before pregnancy planning. Hyperthyroidism, deficiency of specific thyroid substances, deficiency or excess of adrenal hormones, and female diseases (ovarian dysfunction with an unstable background) play a major clinical role.
- Hereditary factor. If there was at least one person in the family who suffered from SVC syndrome, the likelihood of passing it on to offspring almost triples. At the same time, doctors can determine whether it is present in the child. Immediately after birth. Conditionality is absolute, that is, with inheritance, there is no possibility of correction in the future. Treatment is already required; prevention will not help. Fortunately, this kind of defect is relatively mild in course, and the frequency of its development is not high.
These reasons need to be considered in their entirety. Moreover, the gynecologist should pay attention to them even at the stage of pregnancy planning or in the early stages of gestation. If necessary, a referral to a specialized specialist is provided.
Advantages of the clinic
Our clinic employs highly qualified specialists. You can use the help of not only cardiologists, but also therapists and other doctors. They will help diagnose and eliminate the underlying and associated pathologies. All professionals comply with medical ethics and guarantee high-quality examination and prescription of adequate therapy. They have wide diagnostic capabilities. Thanks to this, doctors are able to quickly make an accurate diagnosis. Team interaction of staff makes it possible to accompany the patient at all stages of examination and therapy.
Particular attention is paid to a comfortable environment, openness and warmth of the staff, as well as a loyal pricing policy. Anyone can contact our clinic (including patients with limited financial resources). In our clinic you do not spend money on therapy, you invest it in your health.
Contact us!
Our medical center provides the widest range of services. You can always contact us regarding the treatment of diseases in cardiology. We are ready to provide you with] treatment for sick sinus syndrome[/anchor] and treatment for sinoauricular block.
Symptoms
Signs are heterogeneous (vary from one case to another). If we are talking about the hidden form, they are not there at all. Intermittent or primary varieties are determined by the clinical picture of unequal completeness and intensity of symptoms.
A sample list looks like this:
- The most characteristic moment in the presence of an additional impulse path is arrhythmia. There are many options. Ventricular, atrial types (the first are much more dangerous), tachycardia, slowing of cardiac activity, group or single extrasystole, fibrillation. The correct intervals between contractions are rarely maintained. This is a relatively late sign of deviation. It takes more than one year to develop. Evidence in favor of an advanced syndrome. In the initial phase, everything is limited to tachycardia.
- Chest pain of unknown origin. May be related to episodes or represent a truncated version of them. Characterized by burning and pressing sensations. Tingling does not occur. The development of concomitant diseases is possible.
- Dyspnea. Against the background of intense physical activity or in a state of complete rest. Depends on the stage of the pathological process.
- Weakness, drowsiness, decreased ability to work. Especially with the physical nature of the work.
- Cyanosis of the nasolabial triangle. Blue discoloration of the perioral area.
- Pale skin, sweating, feeling of heat, hot flashes.
- Fainting and syncope. Of a regular nature.
- Disturbances in mental activity and memory.
Many of the presented signs are not directly related to SVC syndrome; they are caused by secondary or tertiary conditions that occur in parallel.
It is not difficult to determine where the disease itself ends and its complications begin. WPW is characterized by arrhythmias of varying severity. The remaining signs are purely atypical for her.
How to stop an attack?
Tachycardia is most typical for the described condition. Along the Kent bundles, the impulse returns from the ventricles to the atria, and the AV node sends it back from the atria to the ventricles. Thus, the signal moves in a circle, and the heart rate doubles or triples.
Regardless of the location of the pathological impulse, stabilization measures must be taken.
But it is worth keeping in mind: you cannot try to recover on your own. It's a waste of time.
Therapy depends on the type of rhythm disorder. If you take drugs at your own discretion, you can die from cardiac arrest, heart attack or other complications.
The algorithm is as follows:
- Call an ambulance. Even if the episode occurred for the first time.
- Calm down, pull yourself together.
- Open a window to bring fresh air into the room.
- Remove oppressive items and jewelry.
- Take prescribed medications. If there are none, Anaprilin (1 tablet) in a system with Diltiazem or Verapamil (the same amount) is suitable for stopping an attack of tachycardia. They will help normalize the rhythm, and not just slow it down.
- You can drink tableted motherwort, valerian, phenobarbital-based drugs (Corvalol, Valocordin).
- Lie down, breathe evenly and deeply. You can try using vagal techniques (pressing on the eyeballs with little force, every 5-10 seconds, holding your breath while inhaling with straining, etc.).
Upon arrival of the brigade, tell about your feelings. If a hospital is offered, go for examination.
Diagnostics
It is carried out under the supervision of a cardiologist. In a hospital or outpatient setting. Regardless of the species, there is time to help. Therefore, urgent measures are rarely taken, and only in the presence of complications.
Examination scheme:
- Oral questioning of the patient. Usually it doesn’t give much, especially in the early stages.
- Anamnesis collection. Factors are identified: family history, somatic pathologies, medications taken, habits and others.
- Heart rate measurement.
- Listening to cardiac sound.
- Electrocardiography. It is prescribed primarily after routine activities. Determines the type of functional impairment. With proper qualifications, a doctor can glean a lot of useful information. Combination with EFI is possible.
- Echocardiography. To identify organic disorders of primary or secondary type.
- MRI. To obtain detailed images of the heart. It is carried out relatively rarely, according to indications. If there are suspicions of other defects of cardiac structures.
Coronography, blood tests, stress tests at the discretion of the doctor.
Signs on ECG
Character traits:
- Expansion of the QRS complex (over 0.12 sec). Deformations reminiscent of those associated with a bundle branch block.
- Narrowing of the PQ interval.
Delta wave changes, depending on the type of process:
| Type A | Type B |
| Delta waves are vertical in all precordial leads. The QRS complex at V2 is similar to the letter A, simulating right bundle branch block. | Delta waves are predominantly negative in leads V1-V3 and predominantly positive in leads V4-V6. This may be mistaken for left bundle branch block or left ventricular hypertrophy with deformation. |
The signs of SVC syndrome on the ECG are specific; even a novice cardiologist can decipher them.
Types of premature excitation of the ventricles
The World Health Organization distinguishes:
- The WPW phenomenon. This pathology is characterized by electrocardiographic signs of impulse conduction through additional channels without manifestations of tachycardia.
- WPW syndrome. This pathology is characterized by a combination of preexcitation and tachycardia.
There are several anatomical variants of the condition:
- With extra muscle fibers. They can go through the fibrous junction, left or right junction, from the right or left atrial appendage.
- With specialized muscle fibers that originate from vestigial tissue.
There are also several forms of pathology:
- Manifesting. This form of the disease is characterized by sinus rhythm, the presence of a delta wave and episodes of tachycardia.
- Intermittent. This form of pathology is characterized by sinus rhythm, tachycardia and transient preexcitation.
- Hidden. This form of the disease is characterized by the absence of electrocardiographic signs and episodes of tachycardia.
Treatment methods
Conservative therapy is aimed only at relieving symptoms; in the later stages, it cannot cope with this either, since large doses of antiarrhythmic drugs lead to the opposite effect.
The main way to restore normal heart function is radiofrequency ablation. The essence of the technique is to cauterize the conduction focus. Precision is important. This is a minimally invasive method and allows you to deal with the problem almost immediately.
In the preoperative period, the use of antiarrhythmic drugs (Amiodarone, Hindin), drugs to lower blood pressure is indicated (if indicated, if there is persistent hypertension, the use of such drugs continues after radiosurgery).
The inpatient period lasts from several days to a week. The patient is monitored over time; stabilization of the rhythm outside of organic disorders occurs after 1-2 days.
If there are defects of a secondary or tertiary nature (already caused by excessive activity of the heart), lifelong maintenance therapy using these medications is indicated. This is why it is recommended to start treatment earlier.