Functional insufficiency of the tricuspid valve, as a rule, is understood as its insufficiency without organic changes in the elements, against the background of dilatation and dysfunction of the right ventricle, dysfunction of the left ventricle, pulmonary hypertension, which occur with pathology of the mitral and, less commonly, aortic valves. According to the authors [3, 6], functional insufficiency of the tricuspid valve occurs in 8-35% of those operated for mitral or aortic valve disease. In the Framingham study [11], functional tricuspid regurgitation occurred in 16.7% of the general population. At the same time, tricuspid regurgitation is one of the predictors of progression of chronic heart failure and increased mortality after adequate correction of valve defects of the left heart [4, 5, 7]. Currently, in our country there remains a fairly significant group of patients with valvular heart defects of rheumatic etiology, amounting to about 50% [1]. In this regard, it seems important to evaluate the relationship between functional tricuspid valve insufficiency and right ventricular myocardial dysfunction and determine their impact on the condition of patients with rheumatic mitral valve disease.
The purpose of the study was to determine the effect of functional tricuspid insufficiency on the results and course of the disease in patients operated on for rheumatic mitral valve disease.
Tricuspid valve defects
Tricuspid valve defects
Tricuspid valve defects are a group of heart diseases that include tricuspid valve insufficiency, tricuspid stenosis, and tricuspid valve defects with predominant stenosis.
The tricuspid valve is located between the right ventricle and the atrium. Its role is to control the flow of blood from the atrium to the right ventricle.
Tricuspid valve insufficiency leads to its abnormal functioning, as well as failure of the entire heart muscle. The two main types of this pathology include:
- the tricuspid valve does not close tightly or does not close at all, causing blood to flow in the opposite direction;
- stenosis (narrowing) of the tricuspid valve, in which the valve flaps are very stiff and do not open wide enough, causing a restriction in blood flow.
Tricuspid valve defects can be caused by:
- infections, such as infective endocarditis or rheumatism;
- expansion of the right ventricle due to increased rigidity of the tricuspid valve ring;
- increased pressure in the valve;
- Less common causes include birth defects, tricuspid valve prolapse, trauma, carcinoid heart disease, tumors, Ebstein's anomaly, and trauma.
If tricuspid valve insufficiency is caused by rheumatism, then the disease usually occurs in combination with pathology of the aortic or mitral valve.
Material and methods
A retrospective analysis of the results of treatment of 56 patients with rheumatic mitral valve disease, operated on in the cardiac surgery department No. 1 of the State Budgetary Institution of Healthcare with Special Clinical Clinical Hospital No. 1 in the period from 2005 to 2010 was carried out. Patients with concomitant interventions, such as operations on the aortic valve and ascending aorta, myocardial revascularization, rhythm restoration interventions were not included in the study.
The majority of patients were women ( n
=47; 84%), average age 55.9±8.2 years. The average NYHA functional class was 3.4±0.5. In 25 (45%) patients, long-term rhythm disturbances in the form of atrial fibrillation or atrial flutter were detected. 21 (38%) patients had a previous history of closed mitral commissurotomy. The left ventricular ejection fraction averaged 58.5±9.7%. The table shows the main clinical characteristics of patients before surgery.
Clinical characteristics of patients before surgery
All patients underwent mitral valve replacement using standard techniques under conditions of artificial circulation, normothermia, cold blood cardioplegia, with cannulation of the ascending aorta and vena cava. In 50 (89%) patients a mechanical prosthesis was implanted, in 6 (11%) - a biological one. In 37 (66%) cases, tricuspid valve annuloplasty was performed: 7 patients underwent support ring repair, and 30 patients underwent DeVega annuloplasty. The average degree of tricuspid regurgitation before surgery was 0.8±0.8: in patients with annuloplasty - 0.9±0.9, without annuloplasty - 0.4±0.5 ( p
=0.029).
The average index of the diameter of the fibrous ring in patients was 18.6±2.4 mm/m2 (in patients with annuloplasty - 18.8±2.4 mm/m2, without annuloplasty - 18.2±2.4 mm/m2; p
=0.38); systolic pressure in the pulmonary artery - 42.7±12.3 mmHg. The decision to perform tricuspid valve repair and its variant was made by the operating surgeon.
Between November 2013 and January 2014, all patients underwent an examination, including examination by a cardiologist, electrocardiography, questionnaires, and echocardiography. The median follow-up period was 58.5 months (36–105 months). To assess right ventricular dysfunction, the echocardiographic protocol additionally included measurement of the amplitude of tricuspid annulus motion (TAPSE) and its peak systolic velocity (TAPSV) [8, 9].
Statistical processing of the data was carried out using the SPSS Statistics 17.0 program. To compare qualitative characteristics, Fisher's test or χ2 was used. When comparing quantitative characteristics, analysis of variance or Student's test was used. If the data did not conform to a normal distribution, Mann–Whitney analysis was used for comparison. To determine the relationship between characteristics, use the Spearman rank correlation method. Differences were considered statistically significant at p
<0,05.
Diagnostics
Tricuspid stenosis is usually diagnosed during a routine medical examination. While listening to a child with a phonendoscope, the doctor hears a systolic murmur caused by abnormal blood flow through the valve. A specialist can determine other signs by measuring the pulse and the development of abnormal pulsation in the neck.
Diagnostic studies include the following procedures:
- echocardiography;
- electrocardiography;
- chest x-ray;
- transesophageal echocardiography;
- cardiac catheterization;
- radionuclide scanning;
- Magnetic resonance imaging.
Mitral valve prolapse 1st degree
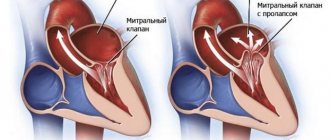
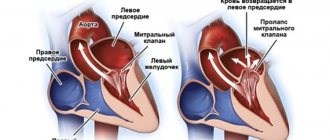
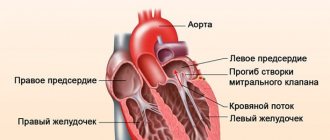
The mitral valve is located on the border between the atrium and the ventricle. Thanks to it, blood flows in one direction. If there are no abnormalities, the valve fits tightly, preventing backflow of blood. Mitral valve prolapse is a condition in which there is sagging of the valve. In this case, sagging of any leaflet may be observed, but grade 1 prolapse of the anterior leaflet of the mitral valve is usually detected.
What are the risk factors?
First degree mitral valve prolapse develops due to structural disorders of the connective tissue. As a result of these changes, the valves cannot resist the reverse flow of blood to the required extent and bend into the atrium cavity.
There are 3 degrees of pathology depending on the amount by which the valves diverge. Mitral valve prolapse with regurgitation of the 1st degree is a condition when blood moves in the opposite direction in a small volume, since the deviation of the valves is 3-6 mm. As a rule, due to a slight deviation, grade 1 mitral valve prolapse without regurgitation is diagnosed. This condition is not dangerous and can be considered as a variant of the norm.
Symptoms are more pronounced in grade 2 pathology. In this case, the doors diverge by 6 to 9 mm.
8
24/7
The most dangerous is grade 3 mitral valve prolapse, in which the protrusion of the leaflets exceeds 9 mm. This option is dangerous, as it leads to hypertrophy of the left ventricle and atrium, resulting in impaired heart function.
Causes
The reasons why grade 1 mitral valve prolapse develops are divided into congenital and acquired.
Congenital may be caused by a genetic mutation during the formation of connective tissue. We are talking about such cases with Marfan and Ehlers-Danlos syndrome. Also, this anatomical change can be inherited.
To acquired ones, i.e. Factors that had a negative impact after birth include the following:
- valve defects of a rheumatic nature;
- arterial hypertension and left ventricular hypertrophy;
- infective endocarditis;
- detachment of the chord due to trauma to the chest;
- chord avulsion due to myocardial infarction.
The most common reason for the development of grade 1 mitral valve prolapse is rheumatic disease. This is an autoimmune reaction that occurs as a result of exposure to certain types of bacteria. Simultaneously with damage to the mitral valve, other valves and joints are also negatively affected.
Symptoms
Mitral valve prolapse of the 1st degree does not manifest itself with severe symptoms. Abnormalities may be indicated by pain in the left side of the chest. The duration of pain varies in each case. It can last a few minutes or several days.
There is no dependence on physical activity, but pain can be triggered by emotional stress.
Other signs that may occur include:
- feeling of lack of oxygen, desire to take a deeper breath;
- arrhythmias;
- headaches and dizziness;
- temperature rise to low-grade levels.
It happens that grade 1 mitral valve prolapse is detected during pregnancy during an ECG. In the absence of regurgitation, this condition is not dangerous for either the mother or the fetus. However, in any case, a pregnant woman should regularly visit a cardiologist to monitor her condition.
Mitral valve prolapse increases the risk of developing gestosis in pregnant women. This condition is dangerous because the fetus does not receive enough oxygen, which leads to growth retardation and the risk of premature onset of labor. In such cases, birth is performed by caesarean section, which reduces the likelihood of complications.
8
24/7
Diagnostics
If you complain of chest pain, you should contact a cardiologist. If regurgitation is severe, a specialist will be able to detect the disorder by listening with a stethoscope.
To obtain more informative data, the following methods are used:
- Ultrasound;
- ECG;
- Doppler.
The main diagnostic method is echocardiography. It allows you to assess the degree of sagging of the valves and the volume of reverse outflow of blood. In addition, secondary changes occurring in the myocardial tissue are visible: chamber dilatation, leaflet hypertrophy, pathology of the annulus fibrosus.
An electrocardiogram is an additional research method. The ECG reflects changes in rhythm, ischemia, and myocardial hypertrophy.
In the process of making a diagnosis, it is necessary to carry out differential diagnosis with the following conditions:
- heart defects – acquired and non-acquired;
- myocarditis of an infectious nature;
- MPP aneurysm;
- prolapse of the 3-leaf valve;
- mitral insufficiency;
- pathology of the interventricular septum.
Treatment
Grade 1 mitral valve prolapse is a condition that does not require treatment if there are no symptoms. In other cases, treatment is prescribed taking into account the patient’s age, gender, and existing symptoms.
As a rule, the following groups of drugs are used:
- sedatives - since the symptoms are caused by disorders of the functioning of the autonomic nervous system;
- beta blockers - aimed at restoring heart rhythm;
- anticoagulants - preventing the formation of blood clots.
The main place in the treatment of early-stage prolapse is adjusting the patient’s lifestyle. It is necessary to choose the optimal level of both physical and mental stress. Protecting the body from emotional overstrain and stress is carried out with the help of sedatives in combination with consultations with a psychotherapist. For physical activity, visiting the pool is recommended. You should also contact a specialist who can create an individual set of physical therapy exercises.
Load regulation is of particular importance when grade 1 mitral valve prolapse is diagnosed in a child. It is important to ensure that the child does not experience any mental or physical stress, as this will lead to an increase in symptoms and the transition of the pathology to the next stage.
Both adults and children are recommended to relax from time to time in specialized sanatoriums, where they will have the opportunity to combine relaxation with undergoing the necessary procedures: acupuncture, massages, etc. Visiting sanatoriums is recommended at least once a year.
At the initial stage of the pathological process, folk remedies can be used. The use of decoctions of motherwort, sage, and St. John's wort is indicated as sedatives. Ginseng infusions will also have a general strengthening effect on the body.
Drugs that may be prescribed:
- Cinnarizine – intended to improve blood microcirculation;
- Cardiometabolites – improve metabolic processes;
- Beta blockers - normalize heartbeat;
- Vitamin and mineral complexes.
Surgical intervention is not used at the initial stage of prolapse.
If there are no symptoms, the patient does not need treatment. The only limitation that exists is control over physical activity. However, it is necessary to regularly visit a cardiologist to monitor the condition and exclude progression of the disease.
Complications
Mitral valve prolapse rarely causes complications - in only 2% of cases.
Possible complications include:
- mitral regurgitation of acute or chronic form - caused by reverse blood flow;
- endocarditis, which can lead to rupture of chords or separation of valve fragments;
- thromboembolism;
- arrhythmias.
Stage 1 mitral valve prolapse is not dangerous due to these complications, but we must not forget that this pathology is prone to progression.
Forecast
Mitral valve prolapse with regurgitation of the 1st degree usually does not lead to circulatory disorders, so the prognosis is favorable if the pathology is detected in time and adequate treatment is prescribed. With an adequate work and rest schedule, changes do not negatively affect the patient’s quality of life.
8
24/7
Prevention
Since mitral valve prolapse is often a congenital anomaly, prevention is discussed only in terms of preventing the development of complications.
In order to reduce the impact of negative factors, the following measures are used:
- regularly visiting a cardiologist and undergoing the necessary examinations;
- complete rest;
- transition to a healthy diet;
- physical therapy exercises to strengthen the heart muscle;
- timely and complete treatment of infectious diseases;
- control of the level of physical and mental stress;
- undergoing sanatorium-resort treatment;
- giving up bad habits - alcohol and nicotine addiction;
- taking medications must be agreed with a doctor;
- protection from stressful situations.
Patients can engage in the following sports:
- sport shooting;
- curling;
- golf;
- bowling;
- karate;
- gymnastics;
- volleyball;
- basketball;
- billiards.
In fact, with the first degree of mitral prolapse there are no strict restrictions. You shouldn't just do weightlifting. Excessively high loads increase the pressure exerted by the blood flow, which can result in increased sagging of the valve leaflets.
Regular visits to a cardiologist will eliminate the further development of pathology. Worsening of the situation requires the prescription of drug treatment.
Treatment
Drug treatment of tricuspid stenosis
Your doctor may recommend regular monitoring of your tricuspid valve disease, with or without predominant stenosis. Clinic visits during which medical examinations are performed may occur once a year or more frequently, depending on your doctor's orders. Diagnostic tests are repeated at certain intervals.
Medicines may also be prescribed by a doctor to relieve symptoms of the disease. Medicines include drugs to relieve symptoms of heart failure or control irregular heart rhythms.
results
During the observation period (compared to the initial values), the functional class (NYHA) decreased to 2.3±0.7 ( p
<0.001), left ventricular contractility improved (ejection fraction - 62.3±10.2%;
p
=0.046), pressure in the right ventricle decreased (35.8±13.6 mm Hg;
p
=0.006).
In the early postoperative period, the average degree of tricuspid regurgitation in patients was 0.3±0.4. In the mid-term period - 1.0±0.6 in patients after annuloplasty - 0.9±0.5, without annuloplasty - 1.3±0.8 ( p
=0.025).
During observation, the diameter of the right atrium did not change significantly: 40.7 ± 8.6 mm before surgery and 38.6 ± 6.6 mm in the mid-term period ( p
= 0.814);
but the size of the right ventricle increased - 34.8±3.8 and 38.8±6.3 mm, respectively ( p
<0.001).
The annulus fibrosus diameter index also did not change significantly relative to the baseline (18.6±2.4 mm/m2 before surgery and 17.9±2.8 mm/m2 during follow-up, p
=0.158).
However, in patients with annuloplasty it was 17.2±2.4 mm/m2, and in patients without annuloplasty it was 19.4±2.8 mm/m2 ( p
=0.004).
A comparative analysis of a number of indicators was carried out in the subgroup of patients with and without annuloplasty. During observation, in patients who underwent annuloplasty, a significant decrease in the diameter index of the tricuspid valve fibrous ring was revealed - 18.8 ± 2.4 mm/m2 before surgery and 17.1 ± 2.4 mm/m2 during observation (95% CI 0.6—2.8, p
=0.003).
While in patients without annuloplasty, dilatation of the fibrous ring was observed - 18.2 ± 2.4 mm/m2 and 19.4 ± 2.8 mm/m2, respectively ( p
= 0.165).
In addition, during the studied period of time, no progression of regurgitation was detected in patients with tricuspid valve annuloplasty - 0.9 ± 0.9 before surgery and 0.9 ± 0.5 during observation ( p
= 1.0), and in patients who did not undergo annuloplasty, a progression of regurgitation was found - 0.4±0.5 and 1.3±0.8, respectively (95% CI 0.5-1.3,
p
<0.001).
At the same time, there was no statistical difference in the functional status of patients. In patients who underwent tricuspid valve annuloplasty, the subsequent NYHA functional class was 2.2 ± 0.6, and in patients without annuloplasty it was 2.4 ± 0.7 ( p
= 0.269).
In all patients, the average TAPSE during observation was 14.8±2.3 mm, TAPSV - 10.0±2.0 cm/s. There were no statistically significant differences in these parameters in patients with or without tricuspid annuloplasty. In the mid-term period, TAPSE and TAPSV were below normal, indicating persistent right ventricular dysfunction despite correction of mitral disease [8, 9]. Correlation analysis revealed a close relationship between the tricuspid valve annulus fibrosus index and right ventricular dilation ( r
= 0.518,
p
< 0.001), as well as less pronounced connections between the tricuspid valve annulus fibrosus index and the degree of tricuspid regurgitation (
r
= 0.269,
p
= 0.045) , tricuspid annulus fibrosus index and NYHA functional class before surgery (
r
=0.272,
p
=0.043), between right ventricular dilatation and left ventricular ejection fraction
( r
=–0.306,
p
=0.022). In the study group of patients, no dysfunction of the mitral prosthesis was observed.
Symptoms and diagnosis of tricuspid valve insufficiency in children in Israel
The etiology of tricuspid valve dysfunction differs into primary and secondary, that is, congenital (organic) and acquired (functional). In the first case, the valve leaflets are affected, they become deformed, wrinkled or calcified. In the second, the valve apparatus is damaged (papillary muscles, chordae tendineae, fibrous ring).
Signs of tricuspid insufficiency:
- blue-yellow complexion;
- puffiness;
- dyspnea;
- cardiopalmus;
- rapid fatigue with low load;
- pain and feeling of heaviness in the right hypochondrium;
- pulsation of neck veins;
- flatulence;
- nausea, vomiting.
In addition to external symptoms, the patient exhibits stagnation in the circulatory system, which is manifested by the accumulation of fluid in the pleural cavity, edema, ascites, and enlarged liver.
| To make an accurate diagnosis, Hadassah doctors prescribe a comprehensive examination. |
Before starting an instrumental or hardware study, the cardiologist conducts a physical examination, analyzes the nature of complaints of malaise and inquires about previous diseases.
The whole process takes from 3 to 7 days. The diagnostic findings brought with you are reviewed, after which an additional check is performed. The laboratories of the Hadassah MC are equipped with high-precision equipment, which eliminates false diagnoses. Often, previously identified pathology is not confirmed.
The following are prescribed for examination:
- Auscultation - listening allows you to determine the heart tone and the presence of arrhythmia.
- Electrocardiogram (ECG) - determines hypertrophy or overload of the right heart chambers, rhythm and conduction disturbances (AV block, tachycardia, atrial fibrillation), the size of the right atrium and ventricle.
- Phonocardiogram - reveals systolic murmur.
- X-ray - detects changes in the size of the atrium and vena cava.
- Echocardiography (EchoCG) is an ultrasound method for recognizing regurgitation, morphological and functional changes in the myocardium and valvular apparatus accompanying congenital heart disease.
- Computed tomography (CT) - the study allows you to study the organ from different angles, accurately visualizes all parameters, and, if necessary, displays a section in any plane.
The completeness of the clinical picture is complemented by the collection of tests (CBC, OAM, biochemical and immunological tests), which can indicate the inflammatory process, deviations from standard indicators in case of damage to internal organs, the content of antibodies and C-reactive protein.
After studying the results of the diagnostic course, the medical council draws up a treatment plan.