Transfusion of blood products and blood components in cancer patients
Have you been denied chemotherapy due to poor blood counts?
Have you decided to undergo chemotherapy with a reduced dosage due to low hemoglobin? Do you require a transfusion of red blood cells (suspension)? Do you need a platelet transfusion? How should a blood transfusion be performed for cancer? Have you received an individual selection of blood products? How safe is blood transfusion? Can you get infected with HIV or hepatitis? How will the body react to someone else's blood? Will there be any complications? Is it possible to refuse the procedure or replace it with something else? Below you will find answers to these and many other questions. The answer is given by Tatyana Evgenievna Dobrosotskaya, hemotransfusiologist, head of the department of anesthesiology and resuscitation of the International Clinic Medica24.
Every day we are approached by several patients who were denied planned chemotherapy at the oncology clinic at their place of residence due to poor blood counts. Most often these are reduced red blood counts - low levels of red blood cells or hemoglobin, or less commonly, “poor” blood clotting indicators, in particular low platelet levels.
Since most chemotherapy drugs damage blood cells and inhibit hematopoietic growth in the bone marrow, a blood transfusion—essentially replacing dead blood cells with donor cells—is the only way to correct the situation. There are a lot of pitfalls and tricks in blood transfusion for cancer that you should know if you receive this medical care for a fee.
Transfusion of blood products and its components, blood products, as well as blood substitutes is carried out according to strict medical indications. Like any complex procedure, it should be trusted only to professionals. The international clinic Medica24 is a modern blood transfusion care for patients.
Principles of blood transfusion at the International Clinic Medica24
- mandatory individual selection of blood for transfusion using gel tests directly at the blood bank;
- multi-year contracts with all major blood banks in Moscow guarantee an uninterrupted supply of blood products of any group and any Rh factor;
- a special procedure for the blood transfusion procedure, which dramatically increases the safety of blood transfusion for cancer patients;
- own bank of blood components for emergencies;
- the presence of a fully staffed emergency department and intensive care unit to guarantee the fight against any possible complications;
- expanded indications for transfusion of blood components in patients with cancer.
What blood products are used for blood transfusion?
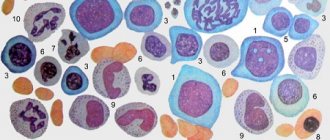
Donor blood in its pure form is rarely transfused, only in military field conditions. The most commonly used blood components, as well as preparations prepared from them:
- erythrocyte mass, as well as erythrocyte suspension, “washed” erythrocytes;
- platelet mass;
- leukocyte mass, leukocyte suspension;
- plasma immunoglobulin preparations
The first two types are usually used for massive bleeding, as well as for chronic anemia, and for tumors with extensive tissue destruction.
Donor leukocytes help fight immunodeficiency conditions, in which the risk of very severe concomitant infection is extremely high. Leukocyte mass is currently used quite rarely.
Plasma is used for the prevention and treatment of the consequences of massive bleeding such as disseminated intravascular coagulation syndrome, as well as in the complex treatment of blood clotting disorders.
Immunoglobulin preparations are used for primary immunodeficiencies, such as HIV, and for secondary ones against the background of long-term chemotherapy with inhibition of the hematopoietic function of the bone marrow.
In addition, blood transfusions are part of the patient's active preparation for major surgical interventions, carried out in order to reduce the risks of severe complications during surgery.
Sign up for a blood transfusion procedure around the clock!
Message sent!
expect a call, we will contact you shortly
Clinical picture and symptoms of hemolytic shock
The clinical picture of transfusion shock covers the following signs that appear at the onset of this condition:
- increasing anxiety;
- the occurrence of short-term excitement;
- pain syndrome localized in the thoracic and lumbar region, as well as in the abdomen;
- the patient feels chills and cold;
- rapid and difficult breathing;
- blue discoloration of the skin and mucous membranes.
Pain in the lower back is called a “marker” symptom or pathognostic manifestation characteristic of hemolytic shock. In this condition, circulatory disorders occur, characterized by:
- arterial hypotension;
- the appearance of sticky cold sweat;
- cardiac arrhythmia with signs of acute heart failure;
- rapid heartbeat accompanied by pain.
The state of transfusion shock is characterized by sustained hemolysis due to the breakdown of red blood cells. The acquisition of a brown color in urine and a high protein content (according to tests) is also a characteristic symptom. There is also a violation of the blood clotting process, the clinical manifestation of this symptom is manifested in profuse bleeding.
Rare symptoms are:
- increased body temperature;
- redness or, conversely, paleness of the skin on the face;
- nausea and vomiting;
- marbling of the skin;
- the appearance of seizures;
- fecal and urinary incontinence.
Symptoms during a procedure performed under anesthesia may not appear at all or may be mild. Careful observation by doctors of the blood transfusion procedure and emergency care when such a complication occurs is the key to its successful elimination.
What are the indications for blood transfusion for cancer?
Absolute indications for blood transfusion include acute blood loss (more than 15% of circulating blood volume) as a result of surgery or massive internal bleeding, severe long-term surgery with extensive tissue damage or blood loss.
The remaining indications are relative, including anemia (hemoglobin level less than 70 g/dl), the addition of inflammatory diseases with severe intoxication, slow healing of postoperative wounds due to the development of a chronic inflammatory process, and a cycle of radiation therapy.
However, indications for blood transfusion may be expanded. For example, a platelet concentrate transfusion is carried out when the platelet level drops below 20*10^9/l, but in case of a threat of bleeding or before chemotherapy, it is recommended to carry out a transfusion when the level is already below 30*10^9/l.
In what cases do cancer patients need blood transfusions?
Most practicing doctors, if asked whether blood transfusions are necessary for cancer, will refuse. Few will clarify that if there is a side process in the form of anemia, then it is necessary to transfuse erythromass. If complications arise in the form of a coagulation disorder, then it is necessary to transfuse the platelet concentrate.
In cancer, there are long-term serious changes in the blood system - anemia and disruption of the hemostasis system. The former can be explicit or hidden. Obvious anemization occurs in cancers accompanied by damage to the mucous membranes and minimal or significant bleeding, primarily cancers of the rectum, colon and sigmoid colon, stomach cancer, cancer of the uterus, vagina, and cervix.
In acute cases, these cancers can also cause heavy bleeding. Chronic anemization most often has a hidden nature, since it is accompanied by a disturbance in the synthesis of the structural component of erythrocytes - hemoglobin, which causes the formation of defective erythrocytes and their entry into the bloodstream; disturbances in the system for rejecting defective red blood cells in the liver and reticuloendothelial system, primarily in the spleen.
As a result, formally, with a superficial glance at a general blood test, it looks normal, however, the red blood cells function poorly, they are defective, they have little hemoglobin, or it is defective, and as a result, a lack of oxygen supply to the tissues leads to chronic hypoxia of all cells of the body.
Hemostasis disorders develop in a similar way, caused by damage to the organs that produce platelets, as well as those responsible for the synthesis of proteins-clotting factors. The result is an increase in the permeability of all mucous membranes and the development of chronic bleeding. As a result, a “vicious circle” develops, from which there is no way out. The greater the chronic blood loss, the worse the compensation mechanisms work.
Chemotherapy drugs and radiation therapy have a depressing effect on all types of cells in the body, but most actively on red bone marrow cells. This accelerates the negative “vicious circle”, and patients with cancer require transfusions of blood and blood components to normalize the patient’s condition and prevent complications such as bleeding and severe infections.
At the Medica24 International Clinic, blood component transfusions are prescribed for borderline low hemoglobin and platelet values.
This allows you to avoid the development of complications of chemotherapy, radiation therapy and prevent them during major operations.
Donor blood is needed by patients after complex operations that are accompanied by large blood loss. Such patients may require massive blood transfusion - a transfusion in which, over a short period of time (up to 24 hours), donor blood in an amount of up to half of the total volume of circulating blood (up to 2-2.5 liters) is introduced into the patient’s bloodstream.
It is almost impossible to obtain such a quantity of blood from one donor, and as a result, blood of different shelf life from different donors, when transfused to one patient, leads to the development of massive blood transfusion syndrome.
We prevent this syndrome through individual selection of blood products and planned operations. In addition, in such cases, we actively use thawed and washed red blood cells.
Publications in the media
Hemorrhagic shock (a type of hypovolemic shock) is caused by uncompensated blood loss - a decrease in blood volume by 20% or more.
Classification: • Mild (loss of 20% of bcc) • Moderate (loss of 20–40% of bcc) • Severe (loss of more than 40% of bcc).
Compensatory mechanisms • Secretion of ADH • Secretion of aldosterone and renin • Secretion of catecholamines.
Physiological reactions • Decreased diuresis • Vasoconstriction • Tachycardia.
Pathogenesis . The patient’s adaptation to blood loss is largely determined by changes in the capacity of the venous system (containing up to 75% of blood volume in a healthy person). However, the possibilities for mobilizing blood from the depot are limited: with a loss of more than 10% of the bcc, the central venous pressure begins to fall and the venous return to the heart decreases. Small output syndrome occurs, leading to decreased perfusion of tissues and organs. In response, nonspecific compensatory endocrine changes appear. The release of ACTH, aldosterone and ADH leads to the retention of sodium, chloride and water by the kidneys, while increasing potassium losses and decreasing diuresis. The result of the release of epinephrine and norepinephrine is peripheral vasoconstriction. Less important organs (skin, muscles, intestines) are switched off from the bloodstream, and the blood supply to vital organs (brain, heart, lungs) is preserved, i.e. centralization of blood circulation occurs. Vasoconstriction leads to deep tissue hypoxia and the development of acidosis. Under these conditions, proteolytic enzymes of the pancreas enter the blood and stimulate the formation of kinins. The latter increase the permeability of the vascular wall, which promotes the passage of water and electrolytes into the interstitial space. As a result, red blood cell aggregation occurs in the capillaries, creating a springboard for the formation of blood clots. This process immediately precedes the irreversibility of shock.
Clinical picture . When hemorrhagic shock develops, there are 3 stages.
• Compensated reversible shock. The volume of blood loss does not exceed 25% (700–1300 ml). Tachycardia is moderate, blood pressure is either unchanged or slightly reduced. The saphenous veins become empty and the central venous pressure decreases. A sign of peripheral vasoconstriction occurs: coldness of the extremities. The amount of urine excreted is reduced by half (at a normal rate of 1–1.2 ml/min).
• Decompensated reversible shock. The volume of blood loss is 25–45% (1300–1800 ml). The pulse rate reaches 120–140 per minute. Systolic blood pressure drops below 100 mm Hg, and pulse pressure decreases. Severe shortness of breath occurs, partly compensating for metabolic acidosis through respiratory alkalosis, but can also be a sign of shock lung. Increased coldness of the extremities and acrocyanosis. Cold sweat appears. The rate of urine output is below 20 ml/hour.
• Irreversible hemorrhagic shock. Its occurrence depends on the duration of circulatory decompensation (usually with arterial hypotension over 12 hours). The volume of blood loss exceeds 50% (2000–2500 ml). The pulse exceeds 140 per minute, systolic blood pressure drops below 60 mm Hg. or not determined. There is no consciousness. Oligoanuria develops.
TREATMENT . In hemorrhagic shock, vasopressor drugs (epinephrine, norepinephrine) are strictly contraindicated, since they aggravate peripheral vasoconstriction. To treat arterial hypotension that develops as a result of blood loss, the procedures listed below are performed sequentially.
• Catheterization of the main vein (most often the subclavian or internal jugular according to Seldinger).
• Jet intravenous administration of blood substitutes (polyglucin, gelatinol, rheopolyglucin, etc.). Fresh frozen plasma is transfused, and, if possible, albumin or protein. For moderate and severe shock, blood transfusion is performed.
• Combating metabolic acidosis: infusion of 150–300 ml of 4% sodium bicarbonate solution.
• GK simultaneously with the start of blood replacement (up to 0.7–1.5 g of hydrocortisone IV). Contraindicated in cases of suspected gastric bleeding.
• Relieving spasm of peripheral vessels. Considering the presence (usually) of hypothermia, warming the patient.
• Aprotinin 30,000–60,000 units in 300–500 ml of 0.9% sodium chloride solution intravenously.
• Inhalation of humidified oxygen.
• Broad-spectrum antibiotics for wounds and septic diseases.
• Maintain diuresis (50–60 ml/h) •• Adequate infusion therapy (until the CVP reaches 120–150 mm H2O) •• If infusion is ineffective - osmotic diuretics (mannitol 1–1.5 g/kg in 5% glucose solution IV in a stream), if there is no effect - furosemide 40-160 mg IM or IV.
• Cardiac glycosides (contraindicated in case of conduction disorders [complete or partial AV block] and myocardial excitability [the occurrence of ectopic foci of excitation]). If bradycardia develops, use b-adrenergic receptor stimulants (isoprenaline 0.005 g sublingually). If ventricular arrhythmias occur, lidocaine 0.1–0.2 g IV.
ICD-10 • R57 . 1 Hypovolemic shock
How is the blood transfusion procedure performed?
The blood transfusion procedure itself is practically painless. It uses standard disposable blood transfusion systems with needles for the cubital (ulnar) veins. If we have a central venous catheter, which we install in all patients in the intensive care unit, as well as in critically ill patients who can be admitted to the intensive care unit from the ward, blood products are administered through the central catheter.
In addition, for patients with cancer undergoing long-term chemotherapy treatment, we strongly recommend the installation of venous port systems (ports) at the initial visit, which will save the veins and which are specially designed for the administration of blood products and chemotherapy drugs over several months.
The duration of the procedure for transfusion of blood and blood components ranges from 30 to 60 minutes when transfusing platelet concentrate (platelet mass), since usually 1-2 doses of 50-60 ml are transfused, up to 2-4 hours, in case of transfusion of 3-4 doses of red blood cells, since its volume per dose is on average 300-350 ml.
Transfusion of platelet concentrate is usually carried out in a blood transfusion room, accompanied by a procedural nurse, whose task is to monitor the patient’s well-being. When receiving red blood cell transfusion, the wait during the procedure can be alleviated by staying in the day hospital ward.
Algorithm of actions for blood transfusion shock
The nurse’s actions at the first manifestations of transfusion shock should be as follows:
- What is cardiogenic shock, emergency care for the victim
- Immediately stop the transfusion. Disconnecting the dropper. The needle remains in the vein for subsequent manipulations.
- An emergency infusion of saline solution begins. The dropper with it is connected to the same needle, since after removing it there is a risk of spending a lot of time inserting a new one.
- The patient is given humidified oxygen through a special mask.
- In an emergency, a laboratory worker is called to perform a rapid blood test, determining the level of hemoglobin, the number of red blood cells, and hematocrit indicators (the ratio of the liquid and cellular parts of the blood).
- A urinary catheter is inserted to monitor urine output. A urine test is sent to the laboratory.
If possible, the patient's central venous pressure is measured, electrocardiography is performed, and the acid-base balance is determined. Hemoglobin in plasma can be quickly detected using the Baxter test.
It is carried out 10 minutes after the start of the transfusion. 10 ml of blood is taken from the patient, the tube is closed and placed in a centrifuge. If, after shaking, the separated plasma is pink in color, destruction of red blood cells can be suspected.
Features of the blood transfusion procedure at the International Clinic Medica24 for cancer patients?
The lion's share of our patients are patients with cancer who receive multiple chemotherapy treatments and, in most cases, have undergone multiple operations, so for them there is a special procedure for routine blood transfusion. We do not allow violations of this order.
To avoid the risks of hemolysis or intravascular coagulation, we make sure to individually select the dose of erythromass and platelet concentrate using gel tests in a blood bank. To do this, the patient comes to us the day before, 1-2 days in advance, and we do rapid blood tests in the presence of the patient.
The results of rapid tests make it possible to clarify the presence or absence of indications for blood transfusion and a preliminary assessment of the required number of doses of drugs. In addition, after collecting blood from the patient, and having received an advance payment for blood products, we send blood samples for gel tests, as well as for checking hemostasis (clotting system) indicators of the blood, and infectious safety (tests for syphilis, HIV, hepatitis).
Upon receipt of individually selected blood products, within 3-24 hours from the moment of receiving the results of rapid tests, we conduct a test for the biological compatibility of each individual blood product and each individual dose with the patient’s blood. Tests are carried out both in vitro (in a special plate) and by administering a small, usually 2-5 ml, microdose of blood to the patient. In the absence of a pyretic or allergic reaction, we administer the first dose. Subsequent doses of blood are administered at intervals, from 20 to 40 minutes, to avoid complications.
After completing the blood transfusion procedure, we take blood for a control examination in order to assess the effectiveness of blood transfusion and blood components. The patient must be examined by a hemotransfusiologist before, during and after blood transfusion. All observation data are entered into the blood transfusion card.
Another secret of our clinic when transfusing blood to cancer patients is the active use of steroid hormones to “cover up” possible side effects of blood transfusion, as well as the use of colony-stimulating factors - drugs that help the body produce red and white blood cells on its own.
Types of treatment procedures
All therapeutic measures for blood transfusion shock are divided into 3 stages:
Emergency anti-shock therapy - to restore normal blood flow and prevent serious consequences. It includes:
- infusion therapy;
- intravenous administration of antishock drugs;
- extracorporeal methods of blood purification (plasmapheresis);
- correction of the function of systems and organs;
- correction of hemostasis (blood clotting);
- treatment of acute renal failure.
Symptomatic therapy – carried out after stabilization of the patient’s condition during the recovery period (recovery).
Preventive measures - identifying the cause of the development of shock and eliminating similar errors in the future, strict adherence to the sequence of transfusion procedures, conducting compatibility tests, etc.
What complications occur with blood transfusion?
Blood transfusion is equivalent to minor surgery, although it has greater risks.
The main causes of complications during blood transfusion are negligence, errors in determining the group by the doctor, violation of the transfusion rules by the procedural nurse.
IMPORTANT: A special place is occupied by complications in cancer patients who refuse individual selection of blood and blood components. The fact is that even in those patients who have not previously had a blood transfusion, the body’s immune system is highly depleted, and the body can produce allergic and other similar reactions, including blood hemolysis. Therefore, one of our secrets is the mandatory individual selection of blood for transfusion using gel tests directly in the blood bank.
When introducing an untested or uncombined blood product or blood component before transfusion, transfusion shock may develop as a result of acute hemolysis (destruction) of the transfused blood. With multiple repeated transfusions without individual selection and verification of individual biological compatibility, pyrogenic and allergic reactions are observed.
In the event of a gross violation of the needle insertion technique by the treatment nurse, violations of the blood transfusion technique (improper filling of the transfusion system), or sudden movements on the part of the patient, an air embolism may develop, for which the immediate entry of 2-3 cubic cm of air into the vein is sufficient.
Thromboembolism develops when the rules for storing and transporting blood are violated, resulting in the formation of clots. Such blood cannot be used, however, if a medical institution violates this prohibition and in order to save money, an actually spoiled or expired blood product can lead to the death of the patient.
Treatment options
Treatment of hemolytic shock and emergency care involve several types of procedures:
- Methods of infusion therapy (infusion of rheopolyglucin, polyglucin, gelatin preparations to stabilize blood circulation and restore microcirculation). Treatment includes the administration of a 4% soda solution to create an alkaline reaction in the urine, which prevents the formation of hemin.
Depending on the level of central venous pressure, an appropriate volume of polyion solutions is transfused, removing free hemoglobin and preventing fibrin degradation.
- Medication methods are used as first aid. They involve the use of classical drugs to recover from a state of shock - prednisolone, aminophylline, Lasix. Antiallergic medications, for example, tavegil, and narcotic analgesics (promedol) are also used.
- Extracorporeal method. This treatment involves removing free hemoglobin, toxins and other products that disrupt the functions of body systems from the patient’s body. Plasmapheresis is used.
- Correcting the functions of systems and individual organs - the use of medications depending on the pathology.
- Correction of the blood coagulation system in renal failure - treatment to restore kidney function.
Prevention of hemolytic shock consists of:
- strict adherence to the rules of blood transfusion;
- storing it correctly;
- thorough examination of donors;
- correct conduct of serological tests.
Prevention is a very important condition when carrying out blood transfusions!
Who can become a donor? Can I give my blood to my relative?
In most cases, the blood type of relatives, even the first degree of kinship, does not match. That is why there are blood banks that accumulate blood of various phenotypes. In addition to the almost universally known ABO blood group system (I, II, III, IV) and the Rh factor (positive / negative), there are more than 40 different blood groups. Therefore, at the international clinic Medica24 we carry out individual phenotyping of each dose of blood transfused to the patient.
We will answer all questions regarding blood transfusion. Call!
Message sent!
expect a call, we will contact you shortly
Is it possible to refuse a blood transfusion?
Before carrying out any procedure or operation at the international clinic Medica24, the patient is always explained in detail the need to perform any intervention. In our work, we are guided by the principle of “reasonable sufficiency”: if there are objective indications for a blood transfusion, or if major operations or chemotherapy or radiation therapy are planned, then we carry out this procedure. If the indications are relative, or no significant interventions are planned, or the body’s reserves have not yet been exhausted, then we recommend refraining from blood transfusions.
In all cases, we recommend that patients listen to the opinion of our specialist doctor and their attending physician.
The risks of refusing a blood transfusion are always higher than the risk of the blood transfusion itself.
Why does the clinic always have blood of any type and any Rh factor?
The international clinic Medica24 is one of the largest private blood consumers in Moscow. We have been closely cooperating for many years with the largest blood banks in the country - the Federal State Budgetary Institution Blood Center of the Federal Medical-Biological Agency of Russia, the Moscow Regional Blood Transfusion Station, the Blood Center of the First Moscow State Medical University named after I.M. Sechenov, since in accordance with the legislation of the Russian Federation (Law of the Russian Federation of June 9, 1993 N 5142-I “On the donation of blood and its components”), blood procurement, receipt of blood components and their storage are carried out exclusively by state budgetary institutions.
The release of drugs from blood banks to our clinic is carried out in the mode of selecting a match between the phenotype of the donor’s blood and the blood of the recipient (patient), determining the presence of Kell antibodies, as well as after individual selection of the compatibility of blood components in the blood bank using gel tests.
The presence of permanent long-term contracts with blood banks allows us to satisfy our requests most quickly and with priority, compared to any other blood consumers.
What should you check with your healthcare provider before agreeing to a blood transfusion?
The Medica24 International Clinic employs hemotransfusiologists with many years of experience in blood transfusion stations, advises specialists from the Blood Center of the I.M. Sechenov First Moscow State Medical University on an ongoing basis, and also carries out linear and remote quality control of the medical care provided. for blood transfusion.
The basis for the work of the transfusiology department of the International Clinic Medica24 is a license for “transfusiology in outpatient and inpatient settings” issued by the Moscow Department of Health.
Due to the possibility of developing serious and dangerous complications during blood transfusion, we strongly recommend that patients undergo it in a hospital setting that includes an intensive care unit.
The material was prepared by Tatyana Evgenievna Dobrosotskaya, Deputy Chief Physician for ICU at the International Clinic Medica24.
Hemorrhagic Shock Clinic
Hemorrhagic shock is manifested by weakness, dizziness, nausea, dry mouth, darkening of the eyes, and with increasing blood loss - loss of consciousness. Due to compensatory redistribution of blood, its quantity decreases in the muscles, the skin is manifested by pale skin with a gray tint; cold, damp limbs. A decrease in renal blood flow is manifested by a decrease in diuresis, subsequently with impaired microcirculation in the kidneys, with the development of ischemia, hypoxia, and tubular necrosis. As the volume of blood loss increases, the symptoms of respiratory failure increase: shortness of breath, irregular breathing rhythm, agitation, peripheral cyanosis.
There are four degrees of severity of hemorrhagic shock:
- I degree of severity is noted when the BCC deficiency is 15%. The general condition is satisfactory, pale skin, slight tachycardia (up to 80-90 beats/min), blood pressure within 100 mm Hg, hemoglobin 90 g/l, central venous pressure is normal.
- II degree of severity - BCC deficiency up to 30%. The general condition is moderate, complaints of weakness, dizziness, darkening of the eyes, nausea, pale and cold skin. Blood pressure is 80-90 mm Hg, central venous pressure is below 60 mm water column, tachycardia up to 100-120 beats / min, diuresis is reduced, hemoglobin is 80 g / l and below.
- III degree of severity occurs when the BCC deficiency is 30-40%. The general condition is serious. There is severe lethargy, dizziness, pale skin, acrocyanosis, blood pressure below 60-70 mmHg, central venous pressure drops (20-30 mmHg and below). Hypothermia, rapid pulse (130-140 beats/min), and oliguria are observed.
- IV degree of severity is observed when the BCC deficiency is more than 40%. The condition is very serious, there is no consciousness. Blood pressure and central venous pressure are not determined, the pulse is noted only in the carotid arteries. Breathing is shallow, rapid, with a pathological rhythm, mobile excitation, hyporeflexia, and anuria are noted.