Intracranial hypertension - what it is, causes and treatment
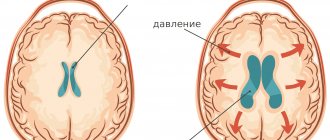
Intracranial hypertension is increased pressure in the cranium. Intracranial pressure (ICP) is the force with which intracerebral fluid presses on the brain.
Its increase is usually due to an increase in the volume of the contents of the cranial cavity (blood, cerebrospinal fluid, tissue fluid, foreign tissue). ICP may periodically increase or decrease due to changes in environmental conditions and the body's need to adapt to them. If its high values persist for a long time, intracranial hypertension syndrome is diagnosed.
The causes of the syndrome are different, most often these are congenital and acquired pathologies. Intracranial hypertension in children and adults develops with hypertension, cerebral edema, tumors, traumatic brain injuries, encephalitis, meningitis, hydrocephalus, hemorrhagic strokes, heart failure, hematomas, abscesses.
Basic Concepts
Intracranial pressure is the difference between pressure in the cranial cavity and atmospheric pressure. Normally, this figure in adults ranges from 5 to 15 mmHg. The pathophysiology of intracranial pressure follows the Monroe-Kelly doctrine.
This concept is based on the dynamic balance of three components:
- Brain;
- Cerebrospinal fluid;
- Blood.
A change in the pressure level of one of the components should lead to a compensatory transformation of the others. This mainly occurs due to the properties of blood and cerebrospinal fluid to maintain a constant acid-base balance, that is, to act as buffer systems. In addition, brain tissue and blood vessels have sufficient elasticity, which is an additional option for maintaining this balance. Due to such protective mechanisms, normal pressure inside the skull is maintained.
If any reasons cause a breakdown in regulation (the so-called pressure conflict), intracranial hypertension (ICH) occurs.
In the absence of a focal cause for the development of the syndrome (for example, with moderate overproduction of cerebrospinal fluid or with slight venous discirculation), benign intracranial hypertension is formed. Only this diagnosis is present in the international classification of diseases ICD 10 (code G93.2). There is also a slightly different concept - “idiopathic intracranial hypertension”. In this condition, the etiology of the syndrome cannot be established.
Symptoms
In young children, intracranial hypertension can remain compensated for quite a long time due to the softness of the bones and the presence of elastic sutures between them, this explains the long-term subclinical course of the disease. Signs of pathology in infants may include restless behavior, screaming, refusal to eat, vomiting, bulging fontanel and suture dehiscence. With chronic hypertension, children lag behind in neuropsychic development.
In older patients, the clinical picture is typical; its severity depends on the form of the disease. In the acute course of intracranial hypertension, the symptoms in adults will be striking:
- severe headache of a bursting nature throughout the skull, especially in the symmetrical frontal and parietal areas, most often disturbing in the morning after getting out of bed, increasing when bending the head and coughing;
- feeling of pressure on the eyes;
- nausea, sometimes sudden vomiting without preliminary nausea, especially in the morning;
- transient visual disturbances in the form of fog or “floaters” before the eyes, double vision, loss of visual fields;
- noises in the head, dizziness;
- neurological picture - the appearance of focal symptoms from different pairs of cranial nerves.
With a sharp increase in ICP, for example, with acute cranial hypertension, there are often disturbances of consciousness up to and including falling into a coma.
The chronic form of ICH usually proceeds more calmly. The headache can be constant, of moderate intensity with periods of intensification. The deterioration of the patient's general condition occurs gradually: insomnia, irritability, weather sensitivity, chronic fatigue. Sometimes crises may occur with increased blood pressure, headache, vomiting, respiratory distress and short-term impairment of consciousness.
Benign intracranial hypertension in most cases is manifested by transient visual disturbances, which often precede the appearance of headaches of varying intensity; focal symptoms include bilateral damage to the abducens pair of cranial nerves, which innervate the eye muscles and are responsible for turning the eye outward. Mild ICH may not produce pronounced symptoms for a long time, moderate intracranial hypertension manifests itself more strongly when atmospheric pressure decreases, making people especially sensitive to weather conditions. The severe form is life-threatening.
Reasons for development
Most often, increased intracranial pressure occurs due to impaired circulation of cerebrospinal fluid (CSF). This is possible when its production increases, its outflow is disrupted, and its absorption deteriorates. Circulatory disorders cause poor flow of arterial blood and its stagnation in the venous section, which increases the total volume of blood in the cranial cavity and also leads to increased intracranial pressure.
In general, the most common causes of intracranial hypertension may be:
- tumors of the cranial cavity, including metastases of tumors of other localizations;
- inflammatory processes (encephalitis, meningitis, abscess);
- congenital anomalies of the structure of the brain, blood vessels, the skull itself (infection of the cerebrospinal fluid outflow tract, Arnold-Chiari anomaly, and so on);
- traumatic brain injuries (concussions, bruises, intracranial hematomas, birth injuries, and so on);
- acute and chronic cerebrovascular accidents (stroke, thrombosis of the dural sinuses);
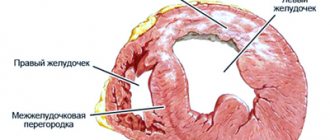
- diseases of other organs that lead to difficulty in the outflow of venous blood from the cranial cavity (heart defects, obstructive pulmonary diseases, neoplasms of the neck and mediastinum, and others);
- poisoning and metabolic disorders (poisoning with alcohol, lead, carbon monoxide, its own metabolites, for example in liver cirrhosis, hyponatremia, and so on).
These, of course, are not all possible situations leading to the development of intracranial hypertension. Separately, I would like to say about the existence of so-called benign intracranial hypertension, when an increase in intracranial pressure occurs seemingly without cause.
Preparations containing amino acids
Preparations with amino acids help not only reduce intracranial pressure, but also accelerate the production of vital enzymes and reduce the load on the brain. These drugs include Glycine - it improves metabolic processes (metabolism in tissues), has an unexpressed sedative and hypnotic effect, and makes memory sharper.
When should you take Glycine:
- in stressful and conflict situations;
- with decreased concentration, attention and performance;
- during the recovery period after a head and brain injury;
- when under difficult conditions of physical and mental labor.
To improve brain function and get rid of regular headaches, the doctor can prescribe the drugs Cerebrolysin and Citrulline simultaneously with Glycine
Symptoms
The formation of clinical hypertension syndrome and the nature of its manifestations depend on the localization of the pathological process, its prevalence and speed of development.
Intracranial hypertension syndrome manifests itself with the following symptoms in adults:
- Headache of increased frequency or severity (increasing headache), sometimes awakening from sleep, often forced positioning of the head, nausea, and repeated vomiting. It can be complicated by coughing, a painful urge to urinate and defecate, and actions similar to the Valsalva maneuver. Possible disturbances of consciousness and convulsive seizures. With prolonged existence, visual impairment occurs.
- History may include trauma, ischemia, meningitis, cerebrospinal fluid shunt, lead intoxication or metabolic disorder (Reye's syndrome, diabetic ketoacidosis). Newborns with cerebral ventricular hemorrhage or meningomyelocele are predisposed to intracranial hydrocephalus. Children with blue heart disease are predisposed to an abscess, and children with sickle cell disease may have a stroke leading to intracranial hypertension.
Objective signs of intracranial hypertension are swelling of the optic disc, increased cerebrospinal fluid pressure, increased osmotic pressure of the extremities, and typical x-ray changes in the bones of the skull. It should be borne in mind that these signs do not appear immediately, but after a long time (except for increased cerebrospinal fluid pressure).
There are also signs such as:
- loss of appetite, nausea, vomiting, headache, drowsiness;
- inattention, decreased ability to awaken;
- papilledema, upward gaze paresis;
- increased tone, positive Babinski reflex;
With a significant increase in intracranial pressure, disturbances of consciousness, convulsive attacks, and visceral-vegetative changes are possible. With dislocation and herniation of brain stem structures, bradycardia, respiratory failure occur, pupillary response to light decreases or disappears, and systemic blood pressure increases.
Which doctor will help determine the level of ICP?
The level of cranial pressure is diagnosed for the purpose of prevention in patients with pathologies that can lead to its increase. In addition, cranial pressure is measured according to indications, that is, in the presence of certain symptoms.
To determine the indicators, you should contact a neurologist and ophthalmologist. The neurologist will initially conduct an examination, during which he evaluates complaints about the characteristic symptoms of the disease. After assessing the condition, if necessary, the specialist prescribes additional diagnostic methods and consultation with other specialists. When examined by an ophthalmologist, signs of increased intracranial pressure can be identified:
- dilatation of retinal vessels;
- swelling of the optic nerve head.
Detection of pathological changes requires additional hardware methods to accurately determine the level of ICP. The diagnostic method is selected individually depending on the patient’s condition. In most cases, the measurement is carried out non-invasively.
Intracranial hypertension in children
There are two types of pathology in children:
- The syndrome slowly increases in the first months of life, when the fontanelles are not closed.
- The disease develops rapidly in children after a year, when the sutures and fontanelles have closed.
In children under one year of age, due to open cranial sutures and fontanelles, symptoms are usually mild. Compensation occurs due to the opening of the sutures and fontanelles and an increase in the volume of the head.
The first type of pathology is characterized by the following symptoms:
- vomiting occurs several times a day;
- the baby sleeps little;
- cranial sutures diverge;
- the child cries often and for a long time without reason;
- the fontanelles swell, the pulsation in them cannot be heard;
- veins are clearly visible under the skin;
- children are developmentally delayed and later begin to hold their head up and sit;
- the skull is large for its age;
- the bones of the skull are formed disproportionately, the forehead protrudes unnaturally;
- When the child looks down, a white stripe of the white of the eyeball is visible between the iris and the upper eyelid.
Each of these signs individually does not indicate increased pressure inside the skull, but the presence of at least two of them is a reason to examine the child.
When the fontanelles and cranial sutures close, the manifestations of intracranial hypertension become pronounced. At this time, the child develops the following symptoms:
- constant vomiting;
- anxiety;
- convulsions;
- loss of consciousness.
In this case, you must definitely call an ambulance.
The syndrome can also develop at an older age. In children over two years of age, the disease manifests itself as follows:
- the functions of the sense organs are impaired due to the accumulation of cerebrospinal fluid;
- vomiting occurs;
- in the morning when waking up, bursting headaches appear that put pressure on the eyes;
- when rising, the pain weakens or recedes due to the outflow of cerebrospinal fluid;
- the child is stunted and overweight.
Increased ICP in children leads to disturbances in brain development, so it is important to detect the pathology as early as possible.
How to identify the problem yourself?
It is impossible to determine the level of cerebral pressure at home, since this procedure requires special equipment. Normal values for an adult are 100-150 mm. rt. Art., if they increase, then the person experiences negative symptoms. You can independently identify intracranial hypertension using the following signs:
- regular headaches;
- nausea, vomiting not associated with food intake;
- causeless weakness, fatigue;
- memory loss;
- attention disorder;
- an attack of dizziness is accompanied by fainting;
- decreased peripheral visual acuity;
- sharp fluctuations in blood pressure;
- weak pulse.
The headache is long-lasting and constant, worsening at night and after waking up
The main manifestation of the pathology is intense headaches that are not amenable to medication. The pain syndrome is bursting in nature and is localized in the frontal, occipital, and temporal regions.
Benign intracranial hypertension (BIH)
This is one of the types of ICP, which can be attributed to a temporary phenomenon that is caused by a number of unfavorable factors. The condition of benign intracranial hypertension is reversible and does not pose a serious danger, since in this case the compression of the brain does not occur due to the influence of any foreign body.
The following factors can cause ADHD:
- Hyperparathyroidism;
- Disruptions in the menstrual cycle;
- Discontinuation of certain medications;
- Hypovitaminosis;
- Obesity;
- Pregnancy;
- Overdose of vitamin A, etc.
Benign intracranial hypertension is associated with impaired absorption or outflow of cerebrospinal fluid. Patients complain of headaches that get worse with movement, and sometimes even with sneezing or coughing. The main difference between the disease and classic cerebral hypertension is that the patient does not show any signs of depression of consciousness, and the condition itself does not have any consequences and does not require special treatment.
Monitoring the effectiveness of treatment
After surgical treatment, it is important for doctors to assess the state of the central nervous system and determine the likelihood of relapse. To monitor the quality of treatment, hardware diagnostics - MRI - are also used. It is absolutely safe to carry out such screening several times in a row, since during the examination the body is not exposed to x-ray radiation. The magnetic fields produced by the MR installation do not have a destructive effect on the body.
The scan can be performed in any medical institution that has the necessary technical facilities and trained functional radiologists. In Moscow, hundreds of diagnostic centers located in every district of the city receive services. To quickly find the nearest MRI medical facility, you can use a single city service.
When you click on the link, a search page will open where you can select a diagnostic service and the area where the clinic is located. In response to the request, a complete list of medical institutions will appear, distributed by rating and prices for procedures. Study the information, read reviews, mark the best offers. To make an appointment for a tomography, just call the phone number listed on each page of the site. All service guests who have booked a scanning time through the portal receive a guaranteed discount of 1,000 rubles on any type of diagnosis.
Complications
The brain is a vulnerable organ. Prolonged compression leads to atrophy of the nervous tissue, which means that mental development and the ability to move suffer, and autonomic disorders occur.
If you do not contact a specialist in time, compression will occur. The brain may be forced into the foramen magnum or into the notch of the tentorium cerebellum. This compresses the medulla oblongata, where the centers of respiration and circulation are located. This will lead to the death of a person. Pressing into the notch of the tentorium is accompanied by constant drowsiness, yawning, breathing becomes deep and rapid, the pupils are noticeably constricted. Wedging of the hippocampal hook occurs, a symptom of which is dilation of the pupil or the absence of a light reaction on the side of the damage. An increase in pressure will lead to dilation of the second pupil, disruption of the breathing rhythm and coma.
High intracranial pressure is always accompanied by loss of vision due to compression of the optic nerve.
Diagnostics
For diagnosis, the pressure inside the skull is measured by inserting a needle attached to a pressure gauge into the spinal canal or into the fluid cavities of the skull.
For staging, a number of signs are taken into account:
- It is determined by poor outflow of venous blood from the skull area.
- According to MRI (magnetic resonance imaging) and CT (computed tomography).
- Judged by the degree of rarefaction of the edges of the ventricles of the brain and the expansion of fluid cavities.
- According to the degree of dilation and blood filling of the veins of the eyeball.
- According to ultrasound data of cerebral vessels.
- According to the results of the encephalogram.
- If the ophthalmic veins are clearly visible and heavily filled with blood (red eyes), then we can indirectly say that there is an increase in pressure inside the skull.
In practice, in most cases, for a more accurate diagnosis and the degree of development of the disease, differentiation of the symptoms of clinical manifestations of hypertension is used in combination with the results of a hardware study of the brain.
Treatment in adults
Therapy is carried out after determining the cause that led to the disease.
Cataract is a pathological condition of the lens, manifested by its clouding and deterioration of vision of varying degrees. Cataract is a disease that is more often diagnosed in older people (in 90% of cases). Read more in the article: “treatment of cataracts with folk remedies.”
Surgical removal of the cause
Indications for surgical intervention:
Advertising:
- hydrocephalus;
- ineffectiveness of puncture and medications;
- visual acuity decreases;
- open traumatic brain injury;
- brain tumors, hematoma, aneurysm.
Methods:
- If there is excessive secretion of cerebrospinal fluid due to hydrocephalus, shunting is performed. The method creates an additional pathway for fluid outflow and reduces intracranial pressure. A silicone catheter is installed into the hole in the skull. It is immersed in the ventricle of the brain. The cerebrospinal fluid is drained by a system of silicone tubes and valves, which is fixed in the abdominal cavity. X-rays are used to monitor the operation.
- Endoscopic perforation. Restores the physiological outflow of fluid. The risk of complications and trauma are minimal. The method is used for ICP after injury, if it is necessary to remove the shunt system, or for complications after shunting.
Other manipulations
- Ventricular puncture. Excess cerebrospinal fluid is drained from the ventricle using a long needle. In half of the cases complications arise and additional punctures may be required. The soft tissue is cut and a hole is made in the skull.
- Lumbar puncture. Excess fluid is removed from the spinal canal. The likelihood of brain damage is minimal. The needle is inserted between the lumbar vertebrae. The area is anesthetized with novocaine. A rubber tube connects the needle cannula to a sterile reservoir, which prevents bacteria from entering the spinal canal.
Medication correction
Advertising:
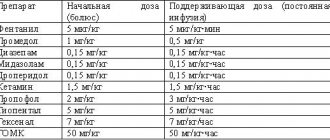
The following medications are used:
| Osmodiuretics | Mannitol | It will help reduce the amount of cerebrospinal fluid and lower ICP. Solution for intravenous administration. Has an anti-edematous effect. |
| Loop diuretics | Furosemide | A fast-acting diuretic that helps with pulmonary and cerebral edema. Has a diuretic effect. Available in tablets. Do not use with gentamicin, cephalosporins, or alcohol. |
| Hormonal agents | Dexamethasone | It has a pronounced anti-allergic, anti-shock, anti-inflammatory effect. Taken for a sharp drop in blood pressure, severe infections, and emergency allergic conditions. Regulates protein, carbohydrate, mineral metabolism. |
| Diakarb | A diuretic drug that has antiglaucoma and antiepileptic effects. The diuretic effect helps reduce moisture production in the structures of the central nervous system. Helps with edema syndrome, glaucoma, epilepsy, increased ICP. | |
| Neuroprotectors | Glycine | Improves brain metabolism in case of disorders, improves mental and physical abilities. Prescribed as a sedative for children and adults. Does not affect healthy tissue. Ineffective as a mental stimulant. |
Dosages, methods and duration of use of drugs are determined by the doctor!
In the absence of complications, they do without medications. They perform manual therapy, osteopathy, and gymnastics.
Diet
Proper nutrition is a necessary condition for normalizing intracranial pressure. Diet 10, 10a is used. They eat 6 times a day. Portions are small and do not burden the gastrointestinal tract.
Limit salt and liquid. The food is boiled, steamed, and consumed pureed. Fried, hot, cold foods, fatty meats and fish, smoked meats, caviar, hard-boiled eggs, fruits with coarse fiber and hard skin, coffee, soda, and kvass are excluded. You should not eat foods that stimulate the central nervous system and cardiovascular system or disrupt the functioning of the gastrointestinal tract.
Advertising:
Is the disease treated with herbs and tinctures? What is the effectiveness of such therapy?
ethnoscience
Folk remedies can activate and improve the functioning of the nervous system, improve blood circulation, and reduce the production of cerebrospinal fluid. Ineffective as a primary treatment.
- Mulberry branches are dried and chopped into pieces. Place two tablespoons in a saucepan, add a liter of cold water, bring to a boil, boil a little, leave for an hour. Strain and drink a glass three times a day. Headaches will become less intense after 10 days.
- Pour 100 ml of tincture of hawthorn, motherwort, valerian, 25 ml of mint tincture, eucalyptus into a dark glass container, mix, add 10 clove sticks, leave to infuse for two weeks. Stir 25 drops in a spoon of water and consume three times a day. The mixture will calm and eliminate spasm of the veins that are responsible for the absorption of cerebrospinal fluid.
- Cut a lemon, squeeze out the juice, add two tablespoons of honey, 100 ml of water. Mix and drink for 20 days.
Treatment of intracranial hypertension
What is the treatment for increased intracranial pressure in adults? If it is benign hypertension, the neurologist prescribes diuretics. As a rule, this alone is enough to alleviate the patient’s condition. However, this traditional treatment is not always acceptable to the patient and cannot always be performed by him. You can’t “sit” on diuretics during working hours. Therefore, special exercises can be performed to reduce intracranial pressure.
A special drinking regime, a gentle diet, manual therapy, physiotherapeutic procedures and acupuncture also help very well with intracranial hypertension. In some cases, the patient manages even without drug treatment. Signs of the disease may disappear within the first week from the start of treatment.
A slightly different treatment is used for cranial hypertension caused by some other disease. But before treating the consequences of these diseases, it is necessary to eliminate their cause. For example, if a person has developed a tumor that creates pressure in the skull, the patient must first get rid of this tumor, and then deal with the consequences of its development. If it is meningitis, then there is no point in treating with diuretics without simultaneously combating the inflammatory process.
In very severe cases (for example, cerebrospinal fluid block after neurosurgical operations or congenital cerebrospinal fluid block), surgical treatment is used. For example, a technology has been developed to implant tubes (shunts) to drain excess cerebrospinal fluid.
PS: A decrease in intracranial pressure (hypotension) is caused by dehydration (vomiting, diarrhea, large blood losses), chronic stress, vegetative-vascular dystonia, depression, neurosis, diseases accompanied by circulatory disorders in the vessels of the brain (for example, ischemia, encephalopathy, cervical osteochondrosis ).
Physiological norm and determination of intracranial pressure
The human skull is a cavity in which the brain is located. To protect it from injury, as well as to maintain its normal operation, there are sections filled with liquid. First of all, the liquid fraction is represented by blood, which is located in the vessels. There is also cerebrospinal fluid (cerebrospinal fluid) present here. It is synthesized in special choroid plexuses and enters the skull through the spinal canal, then is located in the ventricles of the brain and is removed through the venous sinuses. This fluid is necessary for the transport of oxygen and nutrients that are used by brain cells to maintain performance.
Intracranial pressure is a complex value that consists of several factors:
- brain pressure (normally it occupies no more than 85% of the skull space);
- blood - up to 8%;
- spinal cerebrospinal fluid - up to 7%.
Blood and cerebrospinal fluid are in constant motion. If blood circulates through the vascular bed, then spinal fluid moves through the ventricles of the brain and along the spinal canal. These fractions are continuously synthesized, enter the cranium and move further along the vascular bed. When they are in the skull, they put pressure on the inside of the blood vessels and ventricles of the brain. For this reason, intracranial pressure is present in every person, and its value can change every minute. An increase or decrease in this indicator may indicate both pathology and normal physiological processes in the human body.
Bottom line
Thus, intracranial hypertension is a pathological condition that can occur in a variety of diseases of the brain and more. It requires mandatory treatment. Otherwise, a wide variety of outcomes are possible (including complete blindness and even death).
The earlier this pathology is diagnosed, the better results can be achieved with less effort. Therefore, you should not delay visiting a doctor if you suspect increased intracranial pressure.
Beta blockers
Selective beta blockers are intended specifically for the treatment of intracranial pressure. Some of them, for example, Corinfar and Tenorica, have a prolonged effect, they need to be drunk only once every 24 hours, so this form is convenient for older people. List of effective drugs from this group:
- Nebivolol;
- Metoprolol;
- Atenolol;
- Betaxolol;
- Bisoprolol.
Drugs from the beta blocker group are identified by names ending with the syllable “lol”. They should be taken on the recommendation of a doctor, in the required dosage and with the prescribed frequency.