Examination and treatment
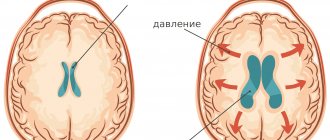
Intracranial hypertension is an increase in pressure exerted by cerebrospinal fluid moving along the brain pathways.
This pathology is included in the list of the most common brain diseases and is a dangerous disease that has a destructive effect on its structures. More often, hypertension is a secondary disease that develops against the background of various factors, including traumatic or oncological etiology. According to statistics from neurologists around the world, representatives of the stronger sex are more susceptible to intracranial hypertension, although in children it is diagnosed with equal frequency in both boys and girls.
Important: high blood pressure can be provoked not only by cerebrospinal fluid, but also by arterial blood or the substrate of a brain tumor.
Get diagnosed with intracranial hypertension at Clinic No. 1:
- Fundus examination
- Ultrasound of cerebral vessels
- X-ray of the head
- EEG
- Angiography
For one-time payment for services - 20% discount
Call
Reasons for development
Under normal conditions, a healthy person's brain is surrounded by intracerebral fluid. This fluid moves non-stop at a certain speed, affecting the brain with a certain level of normal pressure. At the same time, an important point to understand is the “circulation” of the cerebrospinal fluid: part of the liquid is absorbed into the blood, while new cerebrospinal fluid is produced, replacing the total volume of fluid to a normal value. If the absorption of cerebrospinal fluid slows down, or its production becomes excessively active, the volume of liquid at some point begins to exceed the norm. An obvious consequence of this will be an increase in pressure during the movement of intracerebral fluid.
Intracranial hypertension can also develop in newborns. The reason for this, as a rule, is hydrocephalus of any etiology. Among newborns with fluid hypertension in the skull, a large percentage of premature babies.
In adult patients, intracranial hypertension can develop even against the background of swelling of the brain tissue, for example, as a result of traumatic brain injury, meningitis - an infection of the meninges, sarcoidosis, or other diseases of the brain or heart.
Also, long-term use of corticosteroids, hormonal contraceptives, and antibiotics can lead to an increase in cerebrospinal fluid pressure inside the skull.
Reanimatology School of Professor Sergei Vasilievich Tsarenko
An instrumental indicator reflecting the development of brain dislocation and the effectiveness of therapeutic efforts to prevent it is the value of ICP. Most authors consider the value to be 20-25 mmHg. critical level of ICP. However, our experience shows that an objective assessment of the critical level requires an integrated approach - ICP monitoring, CT scanning and assessment of the neurological status, especially the dynamics of dislocation symptoms. We have repeatedly observed patients without clinical and instrumental signs of brain dislocation and with higher ICP values. The opposite is also true. In our practice, there were cases when dislocation symptoms developed at ICP levels lower than 20-25 mm Hg.
There are two fundamentally possible ways to reduce ICP to create a correspondence between the intracranial contents and the space inside the skull. The first way is to increase the space to accommodate the increased volume of the brain by performing decompressive craniotomy. Currently, the previously widely recommended methods of internal decompression - tentoriotomy and falxotomy - are not used. Experience has shown that the negative impact of surgical trauma on the state of the brain outweighs the possible positive effect.
The second way to reduce ICP is to reduce the volume of one of the intracranial components: brain, blood, cerebrospinal fluid and additional pathological formations. The most radical remedy is the removal of intracranial hematomas and areas of irreversibly damaged brain matter (detritus). According to modern requirements, potentially reversible lesions of the brain should be preserved (V.V. Lebedev, V.V. Krylov, 2000).
The next way to reduce the volume of intracranial ingredients is to reduce the excess blood and cerebrospinal fluid in the cranial cavity. A classic, but not universal, measure is to elevate the patient’s head (30-45°). If changes in the patient's head position are ineffective as a means of reducing ICP, it is necessary to clarify the possible causes of intracranial hypertension.
The reasons that cause an increase in ICP are as follows. The first cause of ICH is excessive physical activity of the patient and (or) struggle with a respirator. In this case, they begin with the correction of mechanical ventilation parameters. To stop motor activity and the associated increase in intrathoracic and intracranial pressure, sedatives and narcotic analgesics are administered. It is also possible to use muscle relaxants. However, we try to do this only when absolutely necessary, since the administration of a muscle relaxant makes the patient completely dependent on the medical staff. Any problems with the respiratory equipment (decrease in respiratory rate due to leakage of the respiratory mixture, accidental opening of the respirator circuit and non-compliance of respiratory support parameters with the patient’s requirements) can be fatal for the patient.
This is especially dangerous in emergency hospitals, which often operate under conditions of massive patient admissions and staff shortages. The use of muscle relaxants can dramatically change the minute volume of breathing, cause the accumulation of carbon dioxide and increase ICP instead of decreasing it. JK Hsiang et al. (1994), in a retrospective analysis of case histories of 514 patients with severe TBI, demonstrated that regular and early use of muscle relaxants in 239 patients led to an increase in the duration of their stay in the intensive care unit (from 4.9 to 7.8 days) and a more frequent development of purulent septic complications, especially pneumonia (from 15 to 29%), compared with patients who did not receive relaxants. It should be noted that the increase in the frequency of pneumonia is not surprising, since suppression of the cough reflex contributes not only to the prevention of episodes of intracranial hypertension, but also to impaired sputum evacuation. In addition, after using these drugs, prolonged muscle relaxation, myopathy and even polyneuropathy may develop.
The requirements for an ideal sedative used in the treatment of neurocritical care patients can be formulated as follows: • It must have a short effect so as not to exclude for a long time the possibility of dynamic control of the neurological status. •It should not cause serious hemodynamic disorders.
Typically, a combination of several drugs satisfies these requirements. The most successful is the combination of propofol and a short-acting narcotic analgesic (for example, fentanyl). The only medical problem that arises with the use of this combination is a decrease in blood pressure, so additional administration of a sympathomimetic or ketamine is often necessary. Another serious problem, but only an economic one, is the high cost of this combination of drugs. There are serious objections to the use of ketamine for TBI in the literature. As a rule, authors declare that ketamine increases ICP (EG Cold, BL Dhal, 2002). A detailed analysis of these statements turns out that the authors themselves did not study the effects of ketamine on intracranial hypertension, but heard or read that it increases cerebral blood flow. This is true. Having a sympathomimetic effect, ketamine should increase cerebral blood flow. But, as with the use of pressor amines, blood flow to the brain may decrease or not change! Our clinic is currently conducting a study aimed at clarifying the effects of various analgesics and sedatives on intracranial pressure and oxygenation of the affected brain. So far we do not have enough data to make practical recommendations.
Other possible, but cheaper combinations of sedatives: •Midazolam (Dormikum) or diazepam (Relanium, Sibazon) in combination with ketamine. •Droperidol in combination with ketamine. •Barbiturates – thiopental or hexenal in combination with ketamine. •Sodium hydroxybutyrate (gamma-hydroxybutyric acid, GHB) in combination with midazolam (or diazepam). •Promedol in combination with midazolam (or diazepam). The usual dosage regimens for these drugs are given in Table 10. The indicated doses are approximate and in some patients they may be higher.
Table 10. Usual dosage regimens for sedatives (taking into account their combined use)
Sedatives, in addition to hemodynamic disorders, can also suppress the cough reflex and worsen control over the neurological status, which makes one to be careful when using these drugs and, if possible, limit their use.
The second cause of ICH is the overflow of cerebral vessels with blood (cerebral hyperemia). If, according to an invasive or non-invasive assessment of hemoglobin oxygen saturation in venous blood flowing from the brain, an increase in this indicator of more than 75% is recorded, then a diagnosis of cerebral hyperemia is made. Most often, hyperthermia causes brain hyperemia. To correct hyperthermia (if it is more than 38°C), it is possible to use non-narcotic and narcotic analgesics, as well as sometimes antipsychotics (droperidol). After the administration of these drugs, it is necessary to promptly correct a possible decrease in systemic blood pressure. In addition to pharmacological agents, the use of physical cooling methods is effective: rubbing the skin with 40-50° ethyl alcohol, wrapping in wet sheets, cold water enemas, installing ice packs over large vessels, blowing fans onto the patient, intravenous administration of cooled infusions.
If hyperthermia is not the cause of cerebral hyperemia and intracranial hypertension, then moderate hyperventilation is used to treat this condition, the goal of which is to achieve a SvO2 or rSO2 value of 55%. The advantages and disadvantages of the optimized hyperventilation method are not yet completely clear and require further study.
Most likely, brain hyperemia leads to an increase in ICP when the patient is transferred from a semi-sitting position to a horizontal one. The upside down position is dangerous due to impaired blood drainage from the cerebral veins, so some authors even suggest abandoning catheterization of the internal jugular vein (A. Williams, SM Coine, 1993). J. Meixenberger et al. (1997), studying CPP, ICP and ptiO2 in patients with TBI, found that in a horizontal position, blood pressure and ptiO2 do not change compared to the head elevated by 30°, while ICP increases. In this regard, they consider the horizontal position undesirable when treating patients with TBI.
Our own research also confirms the danger of a horizontal position in the neuroresuscitation period. In almost all patients, raising the head of the bed by 30° led to a decrease in ICP. Under conditions of controlled hypervolemia, this maneuver did not significantly affect blood pressure, so CPP increased. In approximately 50% of patients, an effective measure to reduce ICP was further elevation of the head up to a semi-sitting position.
Of course, in order to judge the effectiveness and necessity of this measure in everyday clinical practice, it is necessary to measure ICP. We observed several patients in whom raising the head of the bed led to a paradoxical increase in ICP. A possible explanation for the discovered fact was the peculiarities of the location of hematomas and foci of brain contusion, as well as the venous outflow from the skull. Since these cases are isolated, in normal practice the standard position of the patient in bed in the neuroresuscitation period is with the head end of the bed elevated by 30-45°. It is necessary to try to limit as much as possible the time the patient remains in a horizontal position if tracheostomy and central venous catheterization are necessary.
The third cause of ICH is impaired cerebrospinal fluid outflow from the cranial cavity. The role of this factor in the genesis of intracranial hypertension can be established based on CT data. When performing a CT scan, signs of obstructive hydrocephalus are revealed, expressed in an increase in ventriculocranial indices and the absence of visualization of the third and (or) fourth ventricles of the brain. In this case, as an emergency measure, use 60-1-2 mg/kg of furosemide and 0.5-1.5 g/kg of mannitol (200-400 ml of 15-20% solution). With excessive accumulation of cerebrospinal fluid in the cranial cavity, both hyperosmolal drugs and saluretics can reduce ICP by blocking cerebrospinal fluid production by the choroid plexuses of the brain. However, this measure is temporary and not effective enough. The use of dehydrating agents may have negative consequences for cerebral circulation due to the development of hypotension and hypovolemia. The method of choice is surgical treatment. Indications for ventricular drainage in TBI arise when the structures of the posterior cranial fossa are damaged, compressing the III and IV ventricles of the brain and impeding the outflow of cerebrospinal fluid, as well as in some cases with ventricular hemorrhage.
As a method of reducing ICP, external ventricular drainage is used in some cases in the absence of occlusive hydrocephalus. The goal is the same - to remove liquor. However, this method is unsafe due to the possibility of infection. In addition, it cannot always be used in patients with TBI due to a sharp decrease in the cerebrospinal fluid spaces - the ventricles and cisterns of the brain. In such conditions it is difficult to install drainage. Moreover, even if this manipulation is successful, problems arise with the removal of cerebrospinal fluid due to the small size of the ventricles.
The fourth cause of ICH is seizures. During convulsions, motor agitation occurs and the synchronization of breathing attempts and the operation of the respirator is disrupted. According to our observations, this can cause an increase in ICP to 60-80 mm Hg. Art. In addition, breathing disorders lead to hypoxia, which is another damaging factor. The factor of brain hyperemia cannot be discounted, since it is known that convulsions activate cerebral metabolism. During seizures, there is an almost 100-fold mismatch between the brain's need for oxygen and its supply. Because of such a negative effect of seizures on the affected brain, we will dwell on the issues of anticonvulsant therapy in more detail.
The fifth cause of ICH is an increase in cerebral ischemia and edema. The leading role of these pathological factors is assumed in cases where there is no evidence of the participation of the previous four. In this case, CT shows signs of pronounced transverse and axial dislocation, large areas of ischemia and edema.
This ICH mechanism is the most difficult to correct. If, according to ICP monitoring and (or) based on an analysis of the neurological picture, increasing intracranial hypertension is diagnosed, then proceed as follows: administer 0.5-1.5 g/kg mannitol for 40-60 minutes. Instead of mannitol, you can use a 3-10% solution of sodium chloride in a volume of 100-200 ml, administered over 30-40 minutes. In 70-80% of cases, a temporary positive effect is achieved - there is a decrease in ICP for 2-3 hours, followed by a gradual increase. Unfortunately, instrumental reduction in ICP after administration of mannitol and hypertonic sodium chloride solution is not accompanied by clinical improvement in all patients.
After using hyperosmolar drugs, polyuria develops within 60-120 minutes. The development of polyuria dictates the need to increase the rate of infusion support to 8-10 ml/kg•h in order to avoid the development of hypovolemia and hypotension. The recommendations of some authors for the use of furosemide after mannitol, supposedly “... to obtain an additive effect and prevent the nephrotoxic effects of a hyperosmolar drug...” seem far-fetched to us. Furosemide does not affect fluid content in the brain. The severity of the nephrotoxic effect of mannitol is determined by the exposure of the drug to the epithelium of the renal tubules. To reduce the duration of this exposure, it is better to increase primary urine secretion through fluid resuscitation and increased renal perfusion than to administer furosemide, which itself may be a nephrotoxic agent.
Currently, there is renewed interest in the use of barbiturates.
It is possible that the mechanism of action of barbituric coma is not only a decrease in the brain's needs for oxygen and nutrients, but also the simultaneous development of vasoconstriction, accompanied by a decrease in ICP. To create a barbituric coma, doses of thiopental up to 4-8 g/day are used, achieving suppression of EEG activity (“burst suppression”). Most researchers believe that it is not necessary to achieve complete suppression of EEG activity, but only about a 50% level. In other words, they consider it sufficient and safer to achieve such an EEG pattern when electrical activity is recorded during half the monitoring time, and “electrical silence” is observed the rest of the time. The extent to which this approach to the use of barbiturates is effective in improving the quality and quantity of life of patients with TBI remains unclear. ‹Ventilation parameters.Up6.2.4. Treatment and prevention of seizures. ›
Symptoms of the disease
Increased intracranial pressure can be recognized by various signs.
- Headache of varying intensity. More often at night, since in a supine position the production of cerebrospinal fluid is activated and its absorption slows down.
- With increased cerebral fluid pressure, a person suffers from nausea and frequent vomiting. Moreover, this is not related to the digestive process. What is typical only for this pathology is that even after vomiting, relief does not come, since the pressure in the brain does not change.
- Nervousness, irritability for no reason, sometimes bordering on aggression, fatigue, even if this condition was not preceded by significant physical activity. This symptomatology is explained by the negative impact of hypertension on a person’s psycho-emotional state.
- Fluctuations in blood pressure, increased sweating, tachycardia, fatigue, chills, short-term fainting, and other symptoms inherent in vegetative-vascular dystonia can also develop when cerebrospinal fluid puts excessive pressure on the brain.
- With chronic intracranial hypertension, a person's sexual desire decreases. This is typical for patients of any gender.
Get diagnosed with intracranial hypertension at Clinic No. 1:
- Fundus examination
- Ultrasound of cerebral vessels
- X-ray of the head
- EEG
- Angiography
For one-time payment for services - 20% discount
Call
Diuretics
Drugs for intracranial pressure with a diuretic effect involve achieving a diuretic effect, due to which the volume of cerebrospinal fluid in the cranium will decrease, and the signs of increased ICP will subside. The rate of excretion of urine and liquid with salts increases due to inhibition in the renal tubules, due to which tissue swelling subsides.
Diuretics are divided into saluretics and osmotic agents. Osmotic drugs are designed to increase pressure in the renal tubules, as a result of which fluid will be excreted many times faster. Saluretics include loop diuretics (Furosemide) and carbonic anhydrase inhibitors (Diacarb, Acetazolamide).
Furosemide is the most common diuretic
Diagnosis of high cerebral pressure
Patients with suspected hypertension are immediately prescribed an MRI. Also carried out:
- Fundus examination is a painless diagnostic method that reveals papilledema, a characteristic sign of hypertension.
- Doppler ultrasound examination of cerebral vessels will reveal if there are “obstacles” in the path of cerebrospinal fluid flow.
- Head X-ray is a simple and accurate method for diagnosing the condition of the brain; it can be performed with or without contrast.
- An electroencephalogram (EEG) is a non-invasive test aimed at measuring the electrical activity of brain cells.
- Angiography.
Diagnostic methods
When the first signs of an abnormality appear, a neurological examination and history taking are performed. If ICH is suspected, invasive measurement of intracranial pressure is prescribed. A needle connected to a pressure gauge is inserted into the spinal canal or cranial cavity. This manipulation is painful, as it involves instrumental penetration.
An alternative that can cope with the diagnosis of ICH is magnetic resonance imaging. The hardware method is absolutely painless and does not involve violating the integrity of living tissues. The patient is placed in a machine that takes pictures of the internal structures. MRI allows not only to detect the main abnormality - intracranial pressure, but also to assess the degree of damage to the central nervous system.
MRI scans reveal the volume of fluid in the cavities, the condition of the vascular network and large arteries, the extent of displacement of brain areas, and areas with impaired blood circulation. Thanks to high resolution and maximum clarity, specialists can detect the root cause of the disease: hematomas, tumors, cysts, foci of inflammation, infection, etc.
Treatment of high intracranial pressure
Living with increased intracranial pressure is quite difficult, and also dangerous. If the disease is not treated, the patient develops hormonal imbalance, the nervous regulation system is disrupted, and intellectual abilities decrease.
The basis of the treatment program is the use of drugs that reduce the production of cerebrospinal fluid and activate the process of its absorption. In severe cases, doctors decide on the need for surgical bypass surgery.
Make an appointment with a neurologist
Experienced specialists conduct consultations in the neurological department of the private Multidisciplinary Medical Hospital. Get rid of unpleasant symptoms and prevent complications caused by increased intracranial pressure by completing a course of treatment.
Information on prices for initial and repeated paid appointments with a neurologist is presented on our website. You can make an appointment with a specialist at a convenient time by phone or using the online form on our website.
Moscow, st. Krasnodarskaya, house. 52, bldg. 2
+7
We work on weekdays and weekends from 8.00 to 21.00
Our specialists
Kuznetsova Evgenia Alexandrovna
- Osteopathic doctor
- pediatrician
- chiropractor
- baby yoga instructor
The cost of the initial appointment is 2200 rubles.
Ladunova Sofya Petrovna
- Chiropractor
- Osteopathic doctor
- visceral therapist
- specialist in massage and kinesio taping.
The cost of the initial appointment is 2200 rubles.
Ladunova Sofya Petrovna
- Chiropractor
- Osteopathic doctor
- visceral therapist
- specialist in massage and kinesio taping.
The cost of the initial appointment is 2200 rubles.
Khokhlov Alexander Vitalievich
- Osteopathic doctor
- visceral therapist
- apitherapist, hirudotherapist.
The cost of the initial appointment is 2500 rubles.