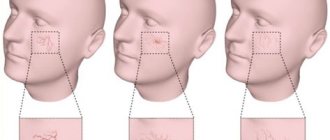
A gentle blush and glowing skin are the result of self-care and good blood circulation on the face. But rosy cheeks are not always a sign of health. Unfortunately, sometimes unpleasant red dots and spider veins begin to appear on the skin. This is rosacea. It can appear all over the body. But such “stars” on the face (in fact, these are dilated blood vessels) worry us most of all. And then we turn to medical cosmetology to remove the capillary network on the face. This redness is caused by dilated blood vessels that extend almost to the surface of the skin. Most often, this pathology overtakes those with thin and delicate skin. They should be especially careful when carrying out many procedures, chemical peels and using strong scrubs. Sensitive skin reacts most acutely to such intervention. And besides this, such a vascular network on the face does not have the best effect on our perception of our own appearance.
Modern cosmetologists offer an effective means of combating the manifestations of rosacea, allowing you to restore a healthy natural glow and an even, fresh complexion. Removing blood vessels with a laser is a painless and safe way to get rid of spider veins.
In this article, we will study in detail what rosacea is, why it manifests itself, what methods besides laser therapy exist to remove it and achieve ideal skin, and is it easy to remove the vascular network on the face?
Cuperosis and vascular network on the face
As we mentioned earlier, this is a superficial manifestation of blood vessels on our skin. Many things can provoke this effect. An elementary increase in temperature, a contrasting transition after a winter street and frost into a warm room, excitement, stress or another reaction of the body when blood circulation increases and blood vessels lose their elasticity and expand. All this can appear on the surface of the skin in the form of unpleasant reddish “patterns”. They are often accompanied by side effects that further negatively affect the condition of the skin: the skin “burns” and dries, peeling and itching appear. Sometimes such irritation even leads to skin injury. All this is very sad and does not contribute to a good mood and confidence in one’s beauty.
Make an appointment at the clinic on Vasilyevsky Island
Sign up
Vascular network on the face: causes and treatment
The manifestation of rosacea is a fairly common phenomenon that affects both women and men all over the planet. The latter, perhaps, do not show this so much, which is why the weaker sex often turns to doctors and cosmetologists, because for a woman a woman’s appearance plays an important role in her inner sense of self.
Internal reasons for the appearance of such a mesh include:
- state of the vascular system;
- diseases and pathologies of the endocrine system;
- genetic predisposition and heredity;
- pathologies of internal organs (for example, the liver, gastrointestinal tract and even the heart);
- use of hormonal drugs and contraceptives;
- high blood pressure.
Even stress can provoke an intensification of these causes and a worsening of the situation: strong feelings are not the best tool for stable and smooth functioning of our heart and blood pressure. It has been proven that nervous situations have no less weak effect on the stomach and pancreas.
For those who smoke and drink alcohol (both of which also greatly affect the vascular system), the manifestation of blood vessels and the appearance of “stars” is a common occurrence. It’s not surprising that bad habits affect the functioning of our body and appearance. Nicotine and alcohol get inside and slowly destroy a healthy body. It's really sad when the effect of this exposure affects the skin.
Let's now touch on the external factors that cause vascular networks to appear on the face. How to get rid of their influence and help your vascular system work better - this topic deserves a separate discussion. Previously, we have already briefly listed the external causes of the appearance of “stars” and unnatural redness of the face, now we will study them in more detail. After all, if you eliminate them or reduce them to a minimum, you can, together with special cosmetic procedures, get rid of rosacea and visible blood vessels on sensitive skin.
It's no secret that both hot and cold water have a strong effect on our blood circulation and blood vessels. Many have been taught that a contrast shower is wonderful and useful. It is true, but not for everyone. For thin, delicate skin, it can become stressful and provoke unhealthy manifestations such as spider veins. Surely you are familiar with the feeling of heat on your cheeks when you enter a warm room from the cold? In essence, this effect is very similar to a contrast shower and also contributes to the appearance of rosacea.
If you are exposed to active sun too often and stay in direct sunlight for a long time, you, unfortunately, can also get spider veins. “What,” you ask, “shouldn’t sunbathe at all?” You can sunbathe, get natural ultraviolet light and vitamin D - all you need is:
- apply protective agents;
- soften and moisturize the skin afterwards;
- cover your face;
- Avoid the sun when the sun is at its zenith.
Such “tanning” is especially dangerous in countries that are closer to the equator. The influence of the sun is most dangerous there, and the consequences can be sad and result not only in the “stars” of blood vessels on the face and body, but also in blisters and burns. You need to be more careful with the bathhouse and steam room - places where external heat also accelerates the blood in our body.
We described the external temperature effect and partially answered the question of why vascular networks appear on the face. However, that's not all. Even the use of a strong and active scrub if used incorrectly, chemical peeling can injure the skin, make it thinner and weaker, severely disrupt the top layer, allowing red blood vessels to come to the surface. But the risk of rosacea may also occur for those who protect themselves from the sun and scrubs. The group of potential “victims” also includes those who lead a sedentary lifestyle, are overweight, or, conversely, expose themselves to excessive physical activity. All this has a direct connection with blood circulation, the heart and the load on blood vessels.
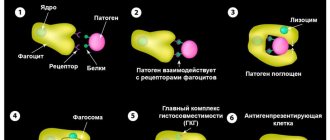
Vascular tumors account for 1 to 7% of all benign human tumors [1–3]. The bulk of human hemangiomas (from 60 to 80%) are localized in the head region [5, 6]. The histological structure of these tumors is very diverse. There are many detailed and complex histological classifications. In clinical practice, doctors use a simplified division of hemangiomas into cavernous, branched (arterial, venous and mixed), capillary and fibroangiomas. In addition to these angiomas, which are usually benign, malignant ones (hemangioendothelioma and angiosarcoma) are also rare. Of all these vascular tumors, capillary and cavernous hemangiomas are the most common [4].
Based on our observations, the first place in frequency belongs to capillary hemangioma. It can be localized in the ear, nasal cavity, pharynx and larynx. The favorite place for the development of capillary hemangioma is the nasal cavity. We observed 25 patients with nasal hemangioma. The neoplasm was most often detected in the cartilaginous part of the nasal septum, in the area of the Kisselbach zone. In this place there are many superficially located vessels, the walls of which, apparently, are the substrate for the development of the neoplasm. Capillary hemangiomas of this localization grow exophytically and are a spherical, wide-based formation of bright red color, soft consistency with a fine-grained surface, without an epithelial membrane. Histologically, the tumor consists of a dense network of small pathological blood vessels (capillaries, precapillaries), devoid of elastic and muscular elements. Quite rarely, the tumor is localized on the lower wall of the vestibule of the nasal cavity or on the anterior end of the inferior turbinate.
This type of hemangioma is much less common in the ear. It is localized mainly on the lower wall of the cartilaginous part of the external auditory canal. Its appearance resembles capillary hemangioma of the nasal cavity. Capillary hemangioma of the tympanic cavity can be classified as a casuistry. We have only one observation of a tumor in this location. It was localized on the lower wall of the tympanic cavity.
The neoplasm spread along this wall, repeating its relief (creeping, fungoid growth of the tumor).
In the pharynx, capillary hemangioma was localized in 10 of our patients. In 6 cases, the neoplasm was located on the edge of the soft palate, near the uvula, in 3 cases - on the anterior palatine arch and in one case - in the hypopharynx, on the aryepiglottic fold. In one observation, this tumor resembled a contact granuloma in clinical appearance, appearance, and location. The tumor was localized in the posterior third of the right vocal fold.
It should be emphasized that in none of our observations did we see a widespread tumor occupying more than one fragment of a particular anatomical region, i.e. it was a tumor process of I-II degree of prevalence according to our clinical classification.
We emphasize once again that this tumor is characterized by exophytic growth. In only one case with capillary hemangioma of the tympanic cavity, creeping (fungoid) growth was noted.
The age of the patients ranged from 18 to 45 years. The average age was 28 years. Most of our patients were between 18 and 35 years of age. We noted the patient's age upon admission to the hospital. Many patients did not see a doctor for a long time or did not agree to treatment in a hospital. If we determine the age at the time of the onset of the first symptoms of the disease, then the average age will shift towards an even younger age. Among the patients, females predominated.
The symptoms of the disease depend to a certain extent on the location of the tumor. One of the first symptoms of capillary hemangioma of the nose was nosebleeds. At first, bleeding recurred rarely (2-3 times a year), and then over the course of 3-4 years it gradually became more frequent and more intense. Patients began to notice difficulty breathing through one half of the nose. This difficulty was, as a rule, insignificant. They consulted a doctor mainly because of increased bleeding and increased intensity.
Patients with pharyngeal hemangioma noted an admixture of blood in saliva or sputum, complained of a sensation of a foreign body in the throat, and some complained of slight pain when swallowing. A patient with a hemangioma in the area of the vocal process of the right arytenoid cartilage complained of weakness and fatigue of the voice and blood in the sputum. Upon examination in the clinic (indirect laryngoscopy, microlaryngoscopy), a diagnosis was made: laryngeal granuloma. During direct laryngoscopy under anesthesia with injection ventilation, the granuloma was removed. After removal, moderate bleeding was observed, which was stopped by coagulation of the wound using surgitron. Histological examination data: capillary hemangioma.
A tumor of the external auditory canal was discovered accidentally. The patient came to the clinic with a complaint of ear congestion. Otoscopy revealed a sulfur plug. After washing the ear, a red tumor was found, round in shape, with a smooth spherical surface, on a wide base with a diameter of 0.5 cm, rising 2-3 mm above the surface of the skin of the lower wall of the cartilaginous part of the external auditory canal. The patient was sent to the clinic. From the anamnesis it became known that the hearing in this ear decreased 10-12 days ago after swimming. The tumor did not obstruct the ear canal and could not cause hearing loss, but it caused the formation of cerumen plug. The tumor was removed using surgitron. Histological examination data: capillary hemangioma.
All patients, with the exception of the patient with capillary hemangioma of the external auditory canal, complained of bleeding or spotting (blood in the sputum, in saliva). This symptom is characteristic of vascular formations. But when carrying out differential diagnosis, it should be borne in mind that bloody discharge from the nose, an admixture of blood in saliva or sputum are possible with malignant neoplasms of the ENT organs.
Capillary hemangioma is painless with light touching and probing, but the slightest trauma causes bleeding. The tumor has almost no effect on the basic functions of the nose and other ENT organs for a long time. A routine examination (rhinoscopy, otoscopy, laryngoscopy and pharyngoscopy using optics) shows that the surface of the formation is granular, moist, not shiny, slightly lumpy. The vascular pattern is visible only around the tumor focus on the healthy mucosa. It has no signs of atypia, sometimes slightly enhanced. The vessels around the tumor respond well to vasoconstrictors, and the tumor itself does not decrease in size or fade. Based on these signs, we presumably make a diagnosis: capillary hemangioma. Diagnostic biopsy should be avoided. It is desirable that the biopsy be a radical intervention.
In most patients, our clinical diagnosis coincided with the results of histological examination. Only in two cases was capillary hemangioma (external auditory canal and vocal process of the arytenoid cartilage) mistaken for granuloma.
The main treatment method for patients with vascular tumors in general and capillary hemangioma in particular remains surgical to this day. Recently, relatively new methods of therapeutic treatment have been introduced into clinical practice - laser and radio wave destruction of tissue. It must be emphasized that these methods did not make the surgeon’s work much easier when removing vascular tumors. The main difficulty remains the fight against intra- and postoperative bleeding.
In recent years, we have again drawn attention to the possibility of using sclerosing, or rather, vascular-obliterating therapy for hemangiomas. To reduce bleeding, and therefore blood loss during surgery, we use TachoComb. More than 5 years ago we stopped removing capillary hemangiomas of the nasal septum. Previously, they were excised together with the underlying mucosa and perichondrium, using radio wave tissue disintegration (surgitron).
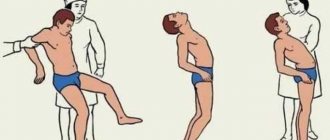
For the treatment of capillary hemangiomas of the nasal cavity and other localizations, we use injections of 1% Fibro-Vain solution. Under local application anesthesia by irrigating the mucous membrane of the nasal cavity or pharynx with a 10% solution of lidocaine with a thin injection needle and a 1-mm syringe through the healthy mucous membrane, 3-4 mm from the edge of the tumor, we inject 0.2-0.00 into the base of the tumor. 3 ml of Fibro-Vayne solution. Before administering the medicine, we pack the nasal cavity around the hemangioma, especially below the tumor, with gauze turunda. In this way, we to some extent reduce the blood flow to the tumor site and the possibility of the injected solution getting beyond the hemangioma. After administration of the drug, the tumor slightly increases in volume.
The introduction of Fibro-Vain solution directly into the tumor tissue is accompanied by severe bleeding. The pathological vessels of the neoplasm are not able to contract. The drug flows out of the tumor tissue along with the blood. Introducing it through a healthy mucous membrane significantly reduces the possibility of bleeding after an injection, and therefore the elimination of the drug in the blood.
Usually the color of the tumor changes the very next day. It darkens and after 2-3 days decreases in volume. On the 4th-5th day, the capillary hemangioma is separated from the healthy tissue. Histological examination in only one observation revealed remains resembling capillary hemangioma; in other cases it was necrotic tissue.
Most of our patients are followed up for 1 to 5 years or more.
Contact with 5 patients was lost. Relapses of hemangioma occurred in 2 cases, 12 and 18 months after treatment.
Relapses occurred after surgery (mechanical removal of the tumor without the use of surgitron). In 18 people observed for a period of 1 to 3 years, there were no relapses of the disease. They were also absent after tumor destruction using Fibro-Wein solution (21 people; follow-up period 1-3 years).
Capillary mesh on the face: tolerate or remove?
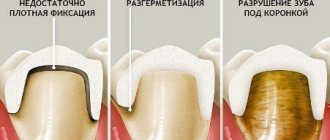
You probably know and have seen where such a mesh pattern on the face is most pronounced. Most often, patients come to us who have thin red lines of blood vessels appearing on their face. The cheeks, nose, and sometimes the chin or forehead are especially affected. This not only complicates the health situation and makes you think about the state of the cardiovascular system, but is also an aesthetic problem.
When thinking about removing capillary mesh on your face, you must understand that procedures and doctor’s advice alone will not be enough. It is important to minimize the impact of internal and external irritants to help your skin recover, strengthen and glow.
Modern clinics offer various ways to remove venous mesh on the face:
- photocoagulation (laser exposure);
- electrocoagulation (exposure to electric shock);
- phototherapy (there are different techniques);
- ozone therapy (exposure to ozone gas)
- sclerotherapy (introduction of special compounds directly into the vessels);
- radio wave surgery.
All methods and techniques have their own specifics. If you decide to remove the vascular network on your face, you should choose them together with a qualified specialist, preferably one who has a medical education and experience in working with similar cases. Don't be afraid to ask questions, because we are talking about your health and appearance.
In our clinic, all cosmetologists are educated in the medical field and know how to select the right treatment for spider veins. We practice laser removal. The method of using a laser to solve the problem of vascular pattern is called effective, powerful and safe.
Prices
Treatment of pigmentation. Service code: A20.01.005
| Description of service | Cost of service, rub. |
| Face | 5 000 |
| Cleavage/hands | 4 000 |
| 1 flash | 250 |
Treatment of blood vessels, post-acne spots, acne. Service code: A20.01.005
| Description of service | Cost of service, rub. |
| Face | 5 000 |
| Cleavage/hands | 4 000 |
| Wings of the nose | 2 000 |
| Cheeks | 3 000 |
Epilation. Service code: A14.01.013
| Description of service | Cost of service, rub. |
| Areas above the upper lip/chin/sideburns | 2 000 |
| Neck | 2 500 |
| Armpits/linea alba | 3 000 |
| Nipple area | 1 500 |
| Back top | 6 000 |
| Back lumbar/chest/abdomen | 4 000 |
| Full hands | 7 000 |
| Forearms | 5 000 |
| Hands | 2 000 |
| Full legs | 13 000 |
| Shin | 7 500 |
| Hips | 8 000 |
| Buttocks | 5 000 |
| Bikini line | 3 500 |
| Bikini pubis | 4 500 |
| Bikini deep | 6 000 |
| Total bikini | 7 000 |
How to remove capillary mesh on the face with maximum effect
Firstly , any doctor will tell you that one procedure will not be enough. And the point is not at all that the “stars” will not disappear the first time. You will see positive results after the first session. Depending on the intensity of rosacea, skin sensitivity, and individual characteristics of the body, you may be prescribed not one manipulation, but several. Even when you seem to have already gotten rid of the line of blood vessels appearing on your face, you will be advised to repeat the sessions after some time to consolidate the effect. The duration of the procedure is only a few minutes; you can first do a gentle peeling to remove excess epidermal cells and the fatty layer. A repeat session will be scheduled for you no earlier than in 3-4 months.
Your nose will delight you with the absence of red veins...
The most modern premium Italian equipment and the vast experience of specialists leave no chance for red veins from burst vessels. You will be surprised how simply and easily a cosmetic defect can be removed.
If you wish, you can also undergo a full examination and identify the cause of poor elasticity of the capillary walls. The doctor will offer you options to eliminate this cause - to avoid the appearance of new red veins in the future.
With DECA, taking care of your appearance and health is a pleasure! Waiting for you!