Varicose veins of the pelvis - symptoms and treatment
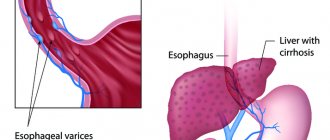
Pelvic varicose veins (PVD) is a disease characterized by dilation of the ovarian veins and intrapelvic venous plexuses [3].
The ovarian vein is a paired vessel that carries venous blood from the ovaries. The right ovarian vein drains into the inferior vena cava, which directly opens into the right atrium. Blood from the left ovarian vein is sent first to the left renal vein and then to the inferior vena cava.
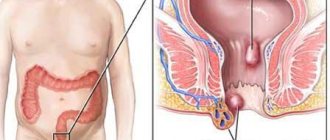
The intrapelvic venous plexuses include a set of veins of various calibers that envelop certain organs and are repeatedly connected to each other. These are the pampiniform plexus of the ovary, uterovaginal, vesical, presacral and rectal plexuses, which also interconnect and drain venous blood from the corresponding organs. Blood from the pampiniform plexus flows mainly into the ovarian veins, from other plexuses - into the internal iliac veins, from where through the common iliac veins it enters the inferior vena cava.
The diversity of views on the development of varicose veins of the pelvis also determines the presence of significant “scatter” in the terminology of this disease. In the domestic literature, the following names are used to denote the disease: pelvic varicose veins, pelvic varicose veins, pelvic varicose veins, pelvic venous congestion syndrome, varicose ovarian veins, left ovarian vein syndrome, pelvic organs overflow syndrome. In the English-language literature, the following terms are used: pelvic congestion syndrome (pelvic venous congestion syndrome), pelvic varicies (pelvic varicose veins), pelvic venous incompetence (pelvic venous insufficiency), pelvic venous disorders (pelvic venous pathology), Iliac vein insufficiency syndrome (iliac vein insufficiency syndrome). veins), pelvic varicocele (pelvic varicocele), pelvic venous stasis (pelvic venous stasis) [1][2].
The disease occurs in all biological periods of women’s lives and does not tend to decrease [4]. VBT is observed in 6-15% of women of reproductive age [5].
This pathology is traditionally associated with the female gender, and therefore it is often called pelvic varicose veins in women. However, recently this concept has begun to extend to males. In this case, the gonadal vein is also damaged, which in men is represented by the testicular vein [6].
Pelvic varicose veins, better known in English literature as pelvic congestion syndrome, is relatively “young”, since it has only recently been identified. Nevertheless, this is a very relevant and independent form of the disease, and its manifestations are witnessed not only by vascular surgeons, phlebologists and gynecologists, but also by a fairly wide range of doctors of other specialties. That is, patients with VBT are treated by various specialists who find something familiar from the arsenal of complaints of this category of patients.
Due to the lack of knowledge of the disease, the diversity and non-specificity of clinical manifestations hidden behind the masks of various diseases, patients with VBT are often subject to long-term and not always adequate observation by urologists, proctologists, vertebroneurologists, nephrologists, gastroenterologists, surgeons, orthopedists, endocrinologists and infectious disease specialists [7] . At the same time, long-term and unsuccessful treatment of symptoms, when efforts are aimed not at the cause of the disease, but at combating its destructive consequences, leads patients into a vicious circle, leaving them alone with their disease. The inability to lead a normal lifestyle, constant pain leading to a decrease in physical and social capabilities, conflicts in the family associated with an inferior sex life, suspicions of faking and exaggerating their symptoms worsen the psychosomatic state of sick women, increasing anxiety and irritability. Ultimately, all this becomes the reason for their referral to a psychiatrist or sex therapist, which, unfortunately, only aggravates the disease [8].
Causes of the disease
Pelvic varicose veins are associated with chronic stagnation of venous blood in the pelvis. The conditions for the occurrence of this process arise against the background of various provoking factors that occur over the course of a woman’s life. The main ones are multiple pregnancies and childbirths . The incidence of the disease is directly proportional to the number of pregnancies. Other risk factors:
- age (most often found in active reproductive age - from 21 to 31 years) [48];
- unfavorable working conditions (forced long periods of sitting or standing, heavy physical labor);
- hereditary predisposition: collagenosis (diseases characterized by damage to connective tissue, especially fibers containing collagen) and angiodysplasia (various structural anomalies of arterial, venous, lymphatic vessels);
- conditions and diseases that increase intra-abdominal pressure (chronic respiratory diseases, constipation, strength sports, etc.);
- sexual dysfunction;
- excess body weight;
- hormonal contraception.
In addition, various gynecological pathologies (inflammatory diseases, endometriosis, ovarian tumors, genital prolapse, bending of the broad ligament of the uterus due to uterine retroflexion), menstrual disorders and hormonal imbalances pose a risk for the development of VBT [9][10].
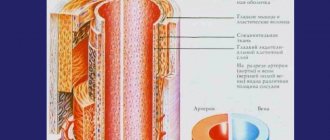
One of the main causes of the disease is a genetic predisposition caused by impaired development of connective tissue, which is the basis of the structure of the venous wall. In this case, the strength of the connective tissue decreases due to a decrease in various types of collagen in its composition or a violation of the ratio between them [11][12].
No less important predisposing factors for the development of VVT are various anomalies in the development of the venous system (venous dysplasia), previous thrombotic lesions of the inferior vena cava system , as well as the so-called venous compression syndromes . These compression syndromes include May-Turner syndrome (compression of the left common iliac vein by the right common iliac artery) and aorto-mesenteric compression syndrome of the left renal vein - Nutcracker syndrome (compression of the left renal vein in the space between the aorta and superior mesenteric artery), in which external compression of venous vessels, preventing the normal outflow of venous blood from the pelvis [13][14][15].
Treatment of May-Turner syndrome
The syndrome requires surgical intervention because it is caused by a mechanical cause (i.e., compression). The goal of the operation is to eliminate it through stenting. To do this, a self-expanding stent is delivered to the area affected by the syndrome, with the help of which the narrowed area is opened.
The stent itself will serve as a framework for the affected area and will be able to provide the required level of vein patency. In order to achieve the desired result, special reinforced stents are used, since conventional ones are not able to cope with high pressure. If, in addition to the syndrome, the patient suffers from severe varicose veins, he undergoes microphlebectomy - an operation aimed at removing damaged areas of blood vessels.
You can make an appointment with specialists from the phlebology department of CELT for the treatment of May-Turner syndrome online or by contacting our operators: +7 (495) 788-33-88
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Causes of pathology
Pathology can develop due to:
- Compression of the vein of an extravasal nature;
- Spread of cancer cells to neighboring organs;
- Formation of blood clots in a vein;
- Lung oncology (up to 90% of diseases);
- Lymphogranulomatosis;
- Lymphoma;
- Metastasis of the tumor from other organs, for example, from the breast;
- Sarcomas and in a number of other cases.
Benign neoplasms, such as cysts, can also become a source of pathology.
In addition, some diseases, for example, tuberculosis, become the “culprit” for the occurrence of pathology.
Pathology can develop slowly or rapidly, it all depends on the cause that caused it. The symptoms are directly affected by the location of the vein blockage and its degree. Sooner or later, a situation arises in which emergency medical care is needed.
Diagnosis of pathology
Activities for diagnosing pathology include:
- X-ray examination;
- Venocavagraphy;
- CT;
- MRI;
- Endoscopy with biopsy.
The doctor needs to determine what caused the pathology. This is important for the selection of treatment methods. So chemotherapy is prescribed only if cancer is confirmed.
Lung cancer: symptoms
Complications
Bleeding is a common complication of the pathology. They can be nasal, pulmonary, esophageal. This is the result of hypertension of the vein and rupture of the affected vascular walls.
In addition, as a result of the development of pathology, the outflow of blood from the vein located in the cranial cavity is disrupted, which can lead to:
- Head pain;
- The occurrence of noise;
- Feeling of constant sleepiness;
- The occurrence of convulsive syndrome;
- Fainting.
With the development of pathology, the functioning of the nerves responsible for vision and hearing is disrupted, which leads to:
- Diplopia;
- Shift of the eyeballs forward;
- Decreased quality of vision;
- Hearing impairment;
- Auditory hallucinations;
- Tinnitus and other unpleasant consequences.
How is magnetic resonance imaging of the inferior vena cava performed?
In medical centers in St. Petersburg, open and tunnel type equipment is used for MR scanning. In the first case, the tomograph consists of a magnetic frame and a table where the patient is located. The device allows you to examine overweight people and people suffering from claustrophobia.
In closed tomographs, the scanning part is represented by a wide tunnel in which an electromagnetic pulse generator is located. The power of the device is 1.5-3 Tesla. The high intensity of the force field allows you to obtain detailed images.
MRI procedure of the abdominal cavity on a closed tomograph
Before scanning, you should remove jewelry, accessories, and piercings. The doctor gives instructions and helps the patient position himself on the tomograph table.
MR angiography of the inferior vena cava takes 45-60 minutes. During this time, the patient must maintain a motionless body position. Random movements cause artifacts to appear in photographs.
The table with the patient is rolled into the apparatus tunnel, and several non-contrast photographs are taken. To administer the “coloring” solution, an automatic system consisting of an intravenous catheter and an injector is used.
Scanning continues after filling the vascular bed with contrast.
MRI allows examination of the inferior vena cava system without bolus enhancement. When scanning natively, a special mode is used, adapted to the constant movement of blood in the vessels.
As a result of MR venography, layer-by-layer images are obtained in three mutually perpendicular projections. To clarify the location of the affected area, you can reconstruct a 3D model of the inferior vena cava system.
During the procedure, medical personnel are located in the adjacent room. Communication with the subject is carried out using a microphone.