Varicose veins of the esophagus are lesions of the veins of this organ, in which the vessels become tortuous and dilated. This pathology is provoked by increased pressure in the portal or vena cava, which leads to stagnation of blood in the venous system of the esophagus and causes vasodilation. In the initial stages, this condition may not manifest itself in any way, and the first sign of its development is often bleeding from the affected vessels.
According to the observations of experts, usually varicose veins of the esophagus are detected in people over 50 years of age. More often this pathology is found in men. Much less often, a hereditary form of varicose veins of the esophagus is detected.
In recent years, the frequency of detection of the pathology discussed in this article has increased significantly, and experts attribute this fact to the widespread prevalence of viral hepatitis, alcoholism and other liver pathologies that lead to the development of portal hypertension. Doctors' wariness towards varicose veins is associated with high mortality rates for this pathology: the first bleeding kills about half of the patients, and with repeated vascular accidents the mortality rate reaches 80%. Esophageal varicose veins are an incurable disease, but its early detection and timely treatment can prolong the life of patients.
In this article you can get answers to many questions about esophageal varices. Why does this pathology occur? How does it manifest itself? What are the methods for diagnosing and treating it?
Causes
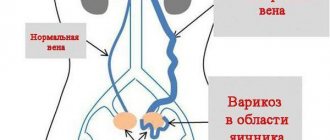
The main cause of esophageal varices is high pressure in the portal vein system (portal hypertension).
In most cases, varicose veins of the esophagus are caused by portal hypertension and much less often provoked by systemic hypertension and congenital pathologies.
Increased portal vein pressure is usually caused by the following diseases and conditions:
- cirrhosis of the liver;
- chronic hepatitis;
- liver tuberculosis;
- liver amyloidosis;
- neoplasms of the liver and pancreas;
- compression of the portal vein by stones, cysts and other neoplasms;
- thrombosis of the portal vein (develops in certain diseases of the heart and blood vessels);
- Randu-Osler syndrome;
- Budd-Chiari disease.
In some cases, portal hypertension develops against the background of chronic cardiovascular failure.
In cases where the dilation of the esophageal veins is provoked by liver diseases, varicose veins are usually observed in the lower parts of the esophagus or the central parts of the stomach. If the disease is caused by pathologies of the cardiovascular system, then the venous vessels expand along the entire length of the esophagus. In addition, vascular nodes arising as a result of pathology in liver diseases are 2-3 times larger than in cardiovascular failure.
The reasons for the development of congenital varicose veins of the esophagus are still unknown.
Classification
Depending on the severity of structural changes in the venous vessels, four degrees of varicose veins of the esophagus are distinguished:
- I – the diameter of the veins increases to 0.5 cm, the vessels become elongated and are located in the lower part of the organ;
- II – the diameter of the veins increases to 1 cm, they become tortuous, nodules up to 3 mm are present on them, bleeding has not yet occurred;
- III – the diameter of the veins exceeds 1 cm, the vessels become tense and constantly dilated, clear nodes are present on them, the mucous membrane of the organ becomes thinner and foci of redness appear on it, bleeding is caused by provoking factors;
- IV – multiple nodes on the veins protrude into the lumen of the esophagus, the mucous membrane of the organ becomes covered with erosions, bleeding occurs spontaneously.
Symptoms
Varicose veins of the esophagus are asymptomatic for a long time, and often the first manifestation of the disease is bleeding, provoked by rupture of the affected vessels. Sometimes, a few days before bleeding, the patient experiences a feeling of pressure and heaviness behind the sternum. In some patients, varicose veins lead to the development of esophagitis, which is provoked by damage to the loose mucous membrane of the esophagus by solid food. In such cases, bleeding may be preceded by manifestations of inflammation of the mucous membrane of the esophagus: burning sensations and heartburn, sour belching, difficulty swallowing solid pieces of food.
When the pressure in the veins of the esophagus increases to 25 mm Hg. Art. or more bleeding occurs. Its intensity may vary, but in approximately 60% of patients it is massive, causes a significant deterioration in the general condition and can lead to death.
In the initial stages of the disease, bleeding is provoked by physical activity, heavy lifting, fever, digestive disorders or overeating, which lead to pressure fluctuations. However, as the pathology progresses, ruptures of varicose vessels can occur even during sleep (that is, they develop spontaneously). Before bleeding occurs, the patient may experience a salty taste in the mouth and a slight tickling sensation.
Over time, frequent and minor blood loss leads to the development of anemia. They are accompanied by the following symptoms:
- weakness;
- nausea;
- vomiting with blood;
- black stool (melena);
- exhaustion.
With massive bleeding, the patient experiences the following manifestations:
- profuse vomiting of blood;
- decreased blood pressure with tachycardia;
- severe weakness;
- increased sweating.
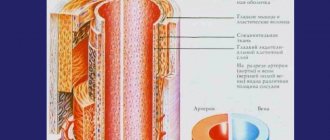
PORTAL GASTROPATHY
Portal hypertensive gastropathy is inherited from portal hypertension with capillary dilatation and rupture of internal mucosal arterial shunts. This indicates the importance of maintaining the liver, which may occur in patients with hepatic portal block. With morphological examination, dilatation of vessels of both the mucous and submucosal balls is indicated. Hemorrhage in the mucous membrane is associated with thrombocytopenia, which develops with liver cirrhosis. With portal gastropathy, the sensitivity of the mucous membrane to various ear-causing agents increases: aspirin, alcohol, etc. Regression of portal gastropathy after transhepatic portosystemic shunting and reduction - after sclerotherapy or ligation of varicose veins is indicated.
The New Italian Endoscopic Club (1997) recommends that the diagnosis of portal gastropathy be based on four signs: mosaic appearance of the mucous membrane, appearance of red spots (mild stage), cherry-red spots, black-brown spots (important). step). The body of the slut is struck in front of us.
It is important to note that portal gastropathy can occur in patients with arterial hypertension without PG, and also in patients without other illnesses, its manifestations can progress, and also disappear. Bleeding, referred to as portal gastropathy, is rarely massive and more often leads to chronic bleeding.
Diagnostics
The doctor can suspect the development of varicose veins of the esophagus based on the patient’s medical history (the presence of background diseases), the patient’s complaints and signs of anemia in the results of a general blood test, which indicate the presence of bleeding. After this, a liver examination is usually carried out (biochemical blood test, ultrasound, MRI), which allows us to identify the root cause of the disease. If necessary, the patient is prescribed studies of the heart and blood vessels (ECG, Echo-CG, etc.).
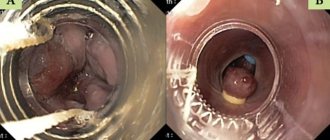
To assess the condition of the esophageal veins, the following diagnostic procedures are performed:
- X-ray of the esophagus with contrast - detects narrowing of the esophagus and deformation of its walls;
- esophagogastroduodenoscopy is the most informative method that allows you to detect bluish protrusions of venous vessels in the lumen of the organ and determine the degree of damage to the veins.
It should be noted that esophagogastroduodenoscopy against the background of bleeding does not always make it possible to determine its source. In such cases, studies are required to identify extraesophageal sources of blood loss. To do this, differential diagnosis of pathology with the following diseases is performed:
- peptic ulcer;
- Mallory-Weiss syndrome;
- thrombocytopenia;
- hemophilia;
- von Willebrand disease;
- thrombocytopenic purpura, etc.
Treatment
To prevent the development of bleeding, the patient must take drugs that reduce pressure in the portal vein.
The goals of treatment for esophageal varices are aimed at treating the underlying disease causing portal hypertension and preventing bleeding.
To prevent bleeding, the patient is recommended to take drugs that reduce pressure in the portal vein. Beta blockers or nitroglycerin can be used for this. In addition, the drug therapy plan includes vitamins, antacids and astringents. In case of bleeding, hemostatic agents are prescribed and transfusions of plasma, blood and red blood cells are performed.
With varicose veins of the esophagus, the patient is recommended to follow a diet that is indicated for the underlying disease. The food you eat should not be hot or cold. It is recommended to eat small meals 5-6 times a day. The patient must give up bad habits and observe moderate physical activity.
To stop bleeding, emergency esophagoscopy is performed, during which endoscopic clipping of the source of bleeding is performed. During this manipulation, a ligating attachment is attached to the endoscope. After inserting the device into the lumen of the organ, it is brought as close as possible to the bleeding vessel and, when the aspirator is turned on, draws a section of the vein into the nozzle. Thus, a ligature or several latex rings are thrown onto the affected vessel, which tighten the vein. As a result, the bleeding stops, and after some time the venous vessel becomes empty and becomes sclerotic.
In addition to clipping, other techniques can be used to stop bleeding during esophagoscopy:
- electrocoagulation of the vessel;
- applying thrombin or an adhesive film to the affected vein.
After stopping the bleeding and stabilizing the patient's condition, slerosis of varicose veins of the esophagus is performed. During this minimally invasive surgical intervention, a special drug is injected into the lumen of the altered vessels, ensuring their “sealing”. After a certain time, the procedure is repeated. Usually, to achieve the desired result, sclerotherapy is performed 4-5 times a year.
If the above measures are ineffective, the patient is advised to perform a bypass, which provides communication between the portal vein and the systemic bloodstream. The purpose of these operations is to eliminate portal hypertension and reduce the risk of bleeding. To achieve this, the following types of bypass can be performed:
- Endovascular transjugular intrahepatic bypass (TIPS). During this operation, a shunt is placed between the portal and hepatic veins. Access to these vessels is through the jugular vein. The catheter is inserted into the right hepatic vein and a needle is inserted through it, with the help of which a puncture of the right branch or trunk of the portal vein is performed. The created channel is expanded with a balloon inflated on the catheter and strengthened with a self-expanding metal stent, which ensures the discharge of blood from the portal vein into the systemic circulation.
- Portocaval shunting (PCS). With this technique, an anastomosis is performed between the portal and inferior vena cava.
- Selective splenorenal shunting. During this operation, a distal anastomosis is performed between the splenic and left renal veins.
If bypass surgery is not possible, the veins of the esophagus are removed or sutured. In some cases, splenectomy is performed.
What are esophageal varicose veins of the first degree?
What obvious signs will allow a gastroenterologist to make a diagnosis? Grade 1 varicose veins (abbreviated as varicose veins) of the esophagus is a rather insidious pathology.
The disease occurs when normal blood flow to the liver is blocked by a clot or scar tissue.
As a result, blood flow is redirected to the smaller blood vessels of the esophagus, which are not designed to carry large volumes of blood.
A gastroenterologist will determine the first degree of varicose veins of the esophagus if, during an endoscopic examination, he sees:
- expansion of the lumens of individual vessels (their diameter should not exceed 5 mm );
- areas of veins raised above the mucous membrane;
- pathologies only in the distal part of the esophageal tube ;
- characteristic mosaic appearance of the mucosa .
But if radiography is performed using contrast, then at the first stage of varicose veins, the esophagus will look absolutely normal. Also, the doctor can easily distinguish the first degree of the disease from the second by performing two simple tests.
First, the diagnostician can press the endoscope on the swollen area of the esophagus. If the size of the veins decreases, then the first stage is diagnosed, but if it does not change at all, the second stage is diagnosed. The gastroenterologist can also inject air into the esophageal tube.
In stage 1 of the disease, the walls with swollen vessels will temporarily take on a normal, healthy appearance.
What symptoms characterize the first stage of esophageal varices?
The first degree of varicose veins of the esophagus is not accompanied by any obvious symptoms. But experts have identified several secondary signs that may indicate the development of an early stage of the disease.
The first sign that the veins in the esophagus have begun to swell is portal hypertension (a pathology in which the pressure in the portal vein increases). A person may also feel:
- unexplained weakness , constant fatigue;
- periodic nausea (without vomiting);
- periodic pain in the liver area , which passes very quickly;
- low blood pressure.
It is important to closely monitor your health, because if you notice not one, but several signs from the above list, you need to sign up for an endoscopy to confirm your concerns.
Varicose veins of the esophagus: classification
To understand how exactly different degrees of esophageal varicose veins differ, it is necessary to understand what classifications there are. At the moment, all gastroenterologists use a three-stage classification.
Stage 1 : the width of the lumen of the veins is no more than 5 mm ; localization of pathological vessels - the distal part of the esophageal tube.
Stage 2 : clearance no more than 10 mm ; the vessels are tortuous and localized in the middle part of the esophagus.
Stage 3 : the diameter of the vessels increases by more than 10 mm ; during endoscopic examination, red spots on the swollen veins are clearly visible. There is also a significant narrowing of the esophageal tube.
But until 1997, experts around the world used the Peckett classification , which divided the disease into four stages.
| Stage | Signs |
| I | lumen diameter (d) 5-10 mm ; Almost complete obstruction of the esophagus is observed, bleeding develops. |
All other types of classifications of esophageal varices, including NIEC (developed by specialists of the Northern Italian Endoscopic Club), OMED (World Organization of Endoscopy), JRSPH (Japanese Association) have minor differences and are based on the same obvious signs. Additionally, the location, shape of varicose vessels, area of lesions, and even the saturation of red markers can be assessed.
Note: I85.9 is the disease code according to ICD-10, II is stage.
Forecast
Varicose veins of the esophagus are an incurable condition and in almost 50% of cases, even the first bleeding occurs, causes the death of the patient. Timely treatment can prolong the life of such patients.
After the first bleeding, more than half of the survivors experience another vascular catastrophe within 1-2 years, which in the vast majority of cases becomes fatal. In addition, the patient’s condition is significantly aggravated by the underlying severe disease.
Symptoms of the disease
Grade 1 varicose veins appear and develop with virtually no obvious symptoms, although in some cases they are still present. This is most often due to the presence of some associated factors. Symptoms are often similar to other diseases of the digestive system; in any case, you should see a doctor if you have:
Varicose veins of the 1st degree appear and develop with virtually no obvious symptoms
- heartburn;
- unpleasant sensation in the upper abdomen and chest;
- frequent belching;
- difficulty swallowing food;
- increased heart rate;
- blood in stool.
General signs of illness may also occur, such as chronic fatigue or vague painful sensations. The importance of timely detection also lies in the fact that esophageal varicose veins of this form can develop rapidly, and the transition from the first to the advanced stage will be very rapid. Although, its development may be very slow.
Which doctor should I contact?
If varicose veins of the esophagus are detected during examinations for the underlying disease or bleeding occurs, the patient should contact a vascular surgeon. After an examination (general and biochemical blood tests, esophagogastroduodenoscopy), the patient undergoes conservative and surgical treatment of the identified pathology and underlying disease.
Varicose veins of the esophagus are a dangerous pathology, which is accompanied by changes in the structure of the venous vessels of this organ and a high risk of bleeding. For a long time, this condition can be asymptomatic, but even the first bleeding can cause the death of the patient. That is why treatment of this pathology should begin as early as possible.
Gastroenterologist I. Alyshov talks about varicose veins of the esophagus:
External factors
In addition to pathological causes, there are a number of extraneous causes that can affect the appearance and development of the disease, these include:
In addition to pathological causes, there are a number of extraneous causes
- alcohol abuse;
- medications that negatively affect the condition of the liver;
- some diseases transmitted by inheritance;
- viral diseases affecting the liver (hepatitis).
Important! Pregnant women should pay increased attention to their health, since any viral infections suffered during this period can be transmitted to the fetus, increasing its risk of developing esophageal varices.