Why is hemoglobin needed in the blood and what does iron have to do with it?
Hemoglobin is a special complex protein that is formed in red blood cells when iron atoms enter there. It is hemoglobin that colors blood red. It is entrusted with the most important mission: it transports oxygen from the lungs to organs and tissues. And vice versa: it transports carbon dioxide back to the lungs to be removed from the body. This important protein is also involved in DNA synthesis, maintaining acid-base balance, and organizing proper metabolism.
This is why low hemoglobin is so dangerous: it reduces the efficiency of all internal organs and systems, the vitality and emotional state of a person. And therefore it must be increased to normal.
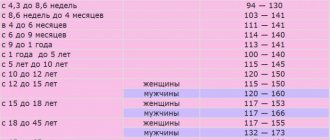
Normal hemoglobin levels in men, women and children
The level of hemoglobin in a person’s blood depends on gender, age and various physiological characteristics of the body. In men, hemoglobin is normal at values of 135–160 g/l. For women, 120–140 g/l are allowed. In pregnant women, the level of hemoglobin decreases noticeably - up to 110 g/l.
Hemoglobin standards for children vary significantly depending on age. The maximum protein level in newborns in the first month of life is from 140 to 200 g/l. Then it declines quite quickly. In the first six months, the norm is considered to be from 90.5 to 140 g/l. In children under 18 years of age, hemoglobin should be in the range of 110–150 g/l, and then equal to the norms of adults.
How to decipher the units of measurement of hemoglobin in the blood?
Hemoglobin is measured in grams per liter (g/L) or grams per deciliter, i.e. 10 liters (g/dL). To convert g/dl to g/l, simply multiply the first figure by 10.
The level of hemoglobin in the blood is influenced by both the innate characteristics of the body and the person’s lifestyle: level of physical activity, environment, type of diet, and the presence of bad habits.
Why is hemoglobin needed?
Almost all types of vertebrate animals require a special delivery system to transport oxygen to tissues, since molecular oxygen is poorly soluble in water: only 3.2 ml of O2 dissolves in 1 liter of blood plasma. The hemoglobin protein (Hb, Fig. 1) contained in vertebrate erythrocytes is capable of binding 70 times more - 220 ml O2/l. The Hb content in human blood varies between 120–180 g/l, which is twice as high as the concentration of plasma proteins (50–80 g/l). Therefore, hemoglobin makes the greatest contribution to maintaining the pH-buffering capacity of the blood. In its structure, adult human hemoglobin (HbA) is a tetramer consisting of two α- and two β-subunits with molecular masses of about 16 kDa. The α and β chains differ in amino acid sequence but have similar conformations.
Figure 1. Hemoglobin molecule. Hemoglobin is one of the most well studied proteins. It was discovered by the German physiologist Otto Funke in 1851, and the structure of this protein was described by the Austrian molecular biologist Max Perutz in 1959, for which he received the Nobel Prize in Chemistry three years later [1].
Visual Science
Figure 2. Oxygen saturation of hemoglobin and myoglobin
[2]
Each hemoglobin subunit carries a heme group with a ferrous iron ion at the center. When O2 binds to the iron atom in heme (Hb oxygenation) and O2 is removed (deoxygenation), the oxidation state of the iron atom does not change. The oxidation of Fe2+ to Fe3+ in heme is random. The oxidized form of hemoglobin, methemoglobin, is unable to transport O2. The proportion of methemoglobin is maintained by enzymes at a low level and amounts to 1–2% [2]. O2 binding centers on each of the four subunits act cooperatively: when an O2 molecule binds to one of them, the others increase their affinity for oxygen (this phenomenon is called positive cooperativity) [3]. As a result, the hemoglobin oxygen saturation curve has a pronounced sigmoidal character (Fig. 2, curve 2).
Another muscle protein, myoglobin, which is the evolutionary predecessor of hemoglobin, is a monomer and contains a single O2 binding site, which is why its oxygen saturation curve is non-sigmoidal (Fig. 2, curve 1). The affinity for oxygen of myoglobin is approximately 13 times higher than that of hemoglobin (50% saturation of myoglobin with O2 is achieved already at a partial pressure of oxygen of 1–2 mm Hg, while for hemoglobin this figure is 26 mm Hg. Art.) [4]. Because of this, hemoglobin is able to efficiently transfer oxygen to tissues and is a more efficient carrier than myoglobin. But it does not follow from this that myoglobin is an ineffective and poorly structured protein, since it performs a fundamentally different biological function - storing oxygen and providing it to mitochondria. These adaptive differences between myoglobin and hemoglobin arose as a result of millions of years of evolution...
Why does hemoglobin fall?
Hemoglobin cannot decrease, much less drop sharply, without reason. They can be serious illnesses or situations that cause blood loss: operations, injuries, wounds, internal and external bleeding. In women, a short-term decrease in protein is possible during menstruation, which lasts 5 days or more. The most common causes are lack of iron, folic acid and vitamin B12. However, low hemoglobin can also be a consequence of serious pathologies.
Causes of low hemoglobin:
- failure of the endocrine system;
- gastrointestinal diseases, intestinal pathologies;
- kidney disease;
- problems with the circulatory system;
- pneumonia, tuberculosis, hepatitis and other serious diseases;
- gastritis and neoplasms in the digestive organs;
- oncological diseases;
- exhausting long-term diets, unhealthy diet;
- vitamin deficiency and lack of vitamins and minerals;
- severe stress or prolonged depression;
- multiple pregnancy.
As you can see, the causes of low hemoglobin can be extremely serious and dangerous to health, and therefore this indicator must be monitored regularly and, if necessary, quickly increased.
Causes of low iron levels
Low iron levels may result from the following diseases and conditions:
- Insufficient intake of microelements from food. This is the most common cause of serum and heme iron deficiency. Passion for diets, as well as refusal to consume animal proteins (vegetarianism, veganism) only aggravate this problem.
- Increased iron consumption. This is most often observed in children during periods of active growth and development, as well as during pregnancy and breastfeeding.
- Infectious diseases. Acute or chronic infections often lead to a decrease in serum iron. This mechanism is evolutionary, since with a low iron content in tissues, cell division (including bacteria) slows down.
- Vitamin deficiency. B vitamins, vitamin C and folic acid are necessary for normal absorption of iron in the intestines. A deficiency of these vitamins leads to poor absorption of iron.
- Anorexia and starvation. A pathological desire to lose weight can lead to anorexia. A person refuses to eat, which quickly leads to exhaustion of the body.
- Dysgesia and parosmia. Distortion of smell (parosmia) and taste (dysgesia) is one of the possible reasons for refusing foods containing iron. For example, a person may become disgusted with meat and meat products. This problem is especially relevant during the coronavirus pandemic. One of the complications of infection is impaired sense of smell and taste.
- Diseases of the digestive tract. Such pathologies impair the absorption of iron in the small intestine.
- Worms. Parasites feed on the host's nutrients and minerals. And some types of worms (for example, roundworms) also drink blood, which also leads to loss of hemoglobin and serum iron.
- Pregnancy and breastfeeding. Particular attention should be paid to the third trimester of pregnancy, when the additional consumption of iron is maximum. It should also be taken into account that the child receives iron through mother’s milk. Therefore, during lactation you also need to take care of getting an adequate amount of iron from food and/or medications.
- Substances that slow down the absorption of iron. These include calcium, vitamin E, zinc and oxalates. Iron absorption is also impaired by coffee and tea.
- Intoxication. Donating blood for iron is also not recommended immediately after infectious and inflammatory diseases. This is due to the fact that during intoxication, iron consumption increases. To neutralize toxins, the liver intensively produces enzymes, an integral part of which is iron.
- Bleeding. This may include bleeding from open wounds, internal bleeding, or heavy menstruation.
Low hemoglobin with normal serum iron levels
We wrote above that normal hemoglobin does not at all indicate a normal level of iron in the blood.
However, the opposite situation is also possible when, with normal or elevated iron levels, the patient has low hemoglobin. For the synthesis of hemoglobin, you need not only iron, but also folic acid and vitamin B123. A lack of these vitamins (even with normal or elevated levels of iron in the blood) leads to a decrease in hemoglobin levels. This occurs when the absorption of vitamins is impaired, their consumption is increased (for example, during pregnancy, childbirth, dysbacteriosis, helminthic infestations, taking certain medications) or insufficient intake from food.
What symptoms indicate low iron levels in the blood?
There are latent and pronounced signs of iron deficiency in the body. The latent stage of iron deficiency is observed with a slight decrease in the concentration of the microelement. This may be accompanied by the following symptoms:
- increased fatigue;
- malaise;
- weakness;
- decreased concentration;
- cardiopalmus;
- brittle nails;
- emotional disorders (depressive states);
- headache and dizziness;
- irritability; pale skin;
- difficulty swallowing;
- hair loss;
- sleep disorder;
- deterioration of memory and cognitive functions.
If iron deficiency is not corrected, symptoms worsen. At the stage of pronounced manifestations it is:
- Decreased immunity. The patient often suffers from acute respiratory diseases.
- Cold extremities. Blood microcirculation deteriorates, causing a person’s feet and hands to freeze. Body temperature may also drop below 36.6 degrees.
- Digestive disorders. There are problems with stool (constipation or diarrhea), flatulence, heartburn, abdominal pain and other symptoms of disorders of the gastrointestinal tract.
- Neurological disorders. A person's mood changes. Irritability and short temper appear. Headaches are common.
- Dyspnea. With a lack of iron, oxygen transport deteriorates. Oxygen starvation occurs, which causes shortness of breath and tachycardia.
How to find out without tests whether you have low hemoglobin: symptoms of deficiency
Many people are accustomed to ignoring a decrease in hemoglobin. Often, even from doctors, you can hear the phrase: “I have lived with low hemoglobin all my life, and nothing.” However, this does not mean that there is no need to look for the cause of the decrease in hemoglobin and eliminate it.
A low level of hemoglobin in the blood gives very specific symptoms, so even a layman can notice them. Here are some of the most common signs of its decline.
Signs of low hemoglobin:
- constant feeling of fatigue, drowsiness, fatigue;
- shortness of breath during physical exertion and normal climbing of stairs;
- regular headaches;
- low blood pressure;
- dry and brittle nails;
- dryness and active hair loss;
- disruption of the gastrointestinal tract;
- pale dry skin, possible peeling;
- tinnitus and dizziness;
- decreased appetite or perverted taste preferences: desire to eat chalk, raw dough or meat, smell paint or gasoline;
- muscle pain, freezing hands and feet;
- regular menstrual irregularities in women;
- decreased potency in men;
- frequent colds and viral diseases.
These symptoms, especially if there are several of them and they are observed for a long time, indicate that the hemoglobin in the blood is already quite reduced. In severe cases, the person may even lose consciousness. This means that you need to look for a solution and take action quickly.
What does low and high hemoglobin levels mean?
When the amount of hemoglobin decreases, a person develops anemia. The main reason for this is considered to be iron deficiency.
Photo: istockphoto.com
Anemia can also be associated with a deficiency of vitamin B12 or folic acid.
In addition, a decrease in hemoglobin levels can be caused by premature death of red blood cells and an increase in the rate of their destruction. This condition is observed in some immune disorders, long-term infectious diseases, as a result of exposure to drugs and chemicals of oxidative action, poisons, burns and frostbite, infectious factors, etc.
Finger on the pulse: what should be the heart rate at different ages
An increase in hemoglobin above normal may indicate dehydration or a high number of red blood cells. Increased hemoglobin is observed in congenital and acquired heart defects, lung diseases, and some cancers. Also, the level may be higher than normal after physical exercise and in general among residents of high mountains, which is associated with a compensation reaction: high mountain air is poor in oxygen, and in this way the body increases its content in the blood.
When to donate blood for hemoglobin
The reason to consult a physician or hematologist and take a blood test for hemoglobin level may be the detection of the above symptoms - one or more, a serious deterioration in health after an illness, significant blood loss due to injury or during surgery, adherence to a strict diet, an identified disease blood from close relatives, pregnancy.
A slight decrease may not be noticeable to humans. To prevent changes in hemoglobin levels from becoming a surprise, it is better to keep the situation under control: get your blood tested 1-2 times a year, and if necessary, consult a hematologist.
What is anemia and how to diagnose it
Anemia (or anemia) is a decrease in hemoglobin and a decrease in the number of red blood cells in the blood. This condition leads to the fact that organs and tissues do not receive the required amount of oxygen, metabolic processes and the general well-being of a person worsen. The first symptoms may be fatigue, shortness of breath, loss of appetite, dry skin, brittle hair and nails and other signs that are not always immediately linked into a single picture.
This is why it is extremely difficult to diagnose anemia on your own, and it is impossible to do this based only on laboratory test results. To make a diagnosis, doctors not only look at the level of hemoglobin and iron, but also check the level of cholesterol, glucose, creatinine, uric acid and electrolytes, assess the general condition of the patient and his internal organs, and conduct a comprehensive diagnosis.
Severity of anemia:
- Mild anemia:
the level of hemoglobin in the blood is less than normal, but more than 100 g/l. The symptoms are subtle, so a person rarely turns to specialists at this stage of the disease. - Moderate anemia:
hemoglobin level in the blood is from 66 to 100 g/l. Frequent dizziness, nausea, drowsiness appear, dryness and cracks in the skin become noticeable. - Severe anemia:
hemoglobin level in the blood is less than 66 g/l. Critical condition, clouding and loss of consciousness, cold hands, fainting. Emergency hospitalization is required as there is a serious threat to life.
However, it is worth consulting at least with a therapist when the indicator drops below 120 g/l in women and below 135 g/l in men, without waiting for the condition to worsen.
How dangerous is anemia for humans?
This disease can be considered both dangerous and relatively harmless at the same time. On the one hand, mild anemia occurs quite often and can be treated without problems. On the other hand, long-term iron deficiency and low hemoglobin levels place a serious burden on the body. Severe anemia can have serious consequences:
- malfunctions of the kidneys, liver and other internal organs;
- diseases of the cardiovascular system;
- cognitive impairment;
- increased risk of falls and, as a result, injuries and fractures;
- oxygen starvation (hypoxia), risk of myocardial infarction and stroke;
- exacerbation of chronic diseases;
- deterioration of the reproductive system;
- anemic coma or death.
However, there is no need to panic. Pathologies and complications tend to develop if hemoglobin is greatly reduced for several years. Regular monitoring and testing of tests 1-2 times a year will be sufficient prevention and will help to quickly identify the problem and begin treatment.
It is important for pregnant women and young children to monitor the level of hemoglobin in the blood and prevent it from decreasing. Otherwise, there is a risk of pregnancy complications, premature birth and impaired fetal development - a malfunction of the brain, nervous and respiratory systems. In young children, a lack of hemoglobin can cause delayed intellectual development.
Causes of high iron
An increased level of iron is said to be when its concentration is more than 28-30 µmol/l (reference values may differ slightly in different laboratories).
The following diseases and conditions can be the causes of elevated iron levels in the blood:
- Hemochromatosis. This is a hereditary disease in which the rate of iron accumulation exceeds the rate of its removal from the body2. Due to such disorders, iron accumulates in tissues, which leads to a number of other diseases. For example, against the background of hemochromatosis, joints may become inflamed (arthritis), sugar levels may rise, and even cirrhosis of the liver may develop.
- Some types of anemia. If with iron deficiency anemia there is a lack of iron, then with hemolytic or sideroblastic anemia there is an excess. In hemolytic anemia, red blood cells are intensively destroyed. This results in the release of heme iron into the blood. With sideroblastic anemia, iron metabolism in the bone marrow is disrupted, which causes hemoglobin synthesis to slow down.
- Iron poisoning. Most often, such poisoning occurs due to an overdose of iron supplements. To prevent this problem, you should take such medications only as prescribed by your doctor. Keep them away from children. For them, the toxic dose is much lower than for adults.
- Thalassemia. This is a hereditary disease in which the process of hemoglobin synthesis is disrupted. With thalassemia, less iron is used for the formation of hemoglobin, which leads to its excess in the blood.
- Blood transfusion. Several days after a blood transfusion, a person usually has an increased iron content.
- Premenstrual period. In women, serum iron levels increase slightly before menstruation. This is a normal physiological phenomenon that can mislead the doctor if you donate blood for analysis during this period. For this reason, women are recommended to donate blood after menstruation.
- Some diseases of internal organs. The level of iron in the blood is greatly influenced by the condition of the liver, spleen and pancreas. With diseases of these organs, there may also be a disturbance in iron metabolism, leading to its excessive accumulation in tissues.
- Excessive iron intake. This is most often observed when taking iron supplements. An excess of iron in the blood from food is unlikely.
What symptoms indicate high iron levels?
Elevated levels of iron in the blood can be manifested by the following symptoms:
- nausea and vomiting;
- bowel disorder (diarrhea or constipation);
- renal dysfunction;
- unexplained weight loss;
- loss of appetite;
- pain and swelling in the joints;
- joint inflammation (arthritis);
- elevated blood sugar levels;
- atherosclerosis;
- hair loss;
- muscle pain;
- decreased immunity (resulting in frequent infectious diseases);
- decreased sex drive;
- delayed physical and mental development in children.
If iron levels are elevated, blood donation is recommended. Photo: kasto / Depositphotos
How to increase hemoglobin
It is quite difficult to quickly increase hemoglobin levels. This process usually takes about a month. You should not assume that self-prescribed vitamins or increased nutrition with meat will work miracles.
The most important thing in the process of normalizing hemoglobin is not to throw iron into the body, but to look for the causes of the malaise. It is important to promptly and correctly diagnose the disease that causes a decrease in hemoglobin, and work with it first. In case of severe blood loss or blood diseases, the patient is given a transfusion of blood or its individual components. This helps replenish its volume.
And already in combination with professional treatment, taking iron-containing medications and adjusting the diet will give a good effect, help avoid complications and improve the patient’s condition.
Important:
Before starting treatment, it is necessary to undergo a medical examination, do a blood test and obtain consultations from all specialized doctors, depending on the diagnosis. Self-medication is unacceptable. All procedures and prescriptions must be agreed with a doctor and regularly monitored by him.
And to prevent iron deficiency and decrease in hemoglobin, it is recommended to adjust your diet and include iron-containing foods. Approximate norms for iron consumption per day are 10–12 mg for men and 20–30 mg for women. More precise figures depend on the person's condition.
Preparing for analysis
Laboratory blood tests often require some preparation to obtain correct results. An analysis of iron levels in the blood (Fe, Iron) is no exception. As a rule, these are the following requirements (which doctors and diagnostic laboratory staff will definitely inform the person about):
- Blood must be donated on an empty stomach.
- 12 hours before the expected test, you should avoid eating fatty foods, smoking and drinking alcohol. Strenuous physical activity is also not recommended.
- If you have to conduct instrumental studies, then you need to donate blood before performing an X-ray or computed tomography.
- A week before donating blood, you should stop taking iron-containing medications. It is also recommended to discontinue other medications (if possible). If the medication cannot be delayed, the patient should tell the doctor, who will take this into account when interpreting the test results.
- If a person has had a blood transfusion, an iron test can only be done a few days after the blood transfusion.
There may also be other recommendations and restrictions for each patient. The doctor will definitely indicate them. It is important to strictly follow the prescribed rules, since the results of the analysis (and therefore the treatment regimen) depend on this.
During pregnancy, women often experience iron deficiency in the body. Photo: freeograph / freepik.com
Which foods contain a lot of iron to increase hemoglobin?
- Dried mushrooms.
A product that can significantly increase iron levels in the body. Just 50 g of dried mushrooms per day will help replenish the iron content in the blood. Not everyone can eat them every day, but periodically including mushrooms in your diet is very useful.
- Red meat.
The dark color of the product indicates a high iron content. For example, a steamed beef cutlet weighing 100 g contains approximately 2.7 mg of iron - almost 15% of the daily requirement. For comparison: in the same turkey cutlet the amount of iron is about 0.7 mg.
- Pumpkin seeds.
An excellent source of iron: 200 g of the product easily covers the daily requirement. But you shouldn’t get carried away with pumpkin seeds: they are very high in calories and can cause disruptions in the gastrointestinal tract. But a small handful of seeds in a salad or hot dish will be very useful.
- Offal.
In terms of the content of iron and other useful microelements, offal easily surpasses meat. 100 g of cooked beef liver contains 36% of the daily iron requirement.
- Buckwheat and rolled oats.
A couple more important foods that can boost your iron levels. A 100 g serving of buckwheat or rolled oats will provide the body with approximately 25% of the beneficial element.
- Legumes.
An essential part of the diet for vegetarians and vegans, legumes are not only rich in iron, but also very filling. A cup of boiled lentils, for example, will cover approximately 35% of the daily requirement for iron, and a glass of boiled beans will cover 20%.
- Dark chocolate.
Perhaps the favorite product of those who seek to increase their hemoglobin levels. The main thing is to choose chocolate with a cocoa content of at least 70% and eat at least ¼ bar (25 g) per day. This will help compensate for about 17% of the daily iron requirement and give you a good mood due to the “happiness hormone”.
For iron deficiency and low hemoglobin, the following foods are also recommended: eggs (especially the yolk), quinoa, almonds, walnuts, peeled apples, pomegranate, grapes, raspberries, rose hips, beets, freshly squeezed fruit and vegetable juices, seafood - caviar, fish, oysters It is important that the diet is balanced and that foods contain a variety of nutrients and vitamins.
Indications
The level of iron in the blood is determined for the following purposes:
- for diagnosis, differential diagnosis and control of treatment of various types of anemia;
- for diagnosing hemochromatosis, a hereditary disease in which iron metabolism is disrupted (there is too much of it);
- to determine transferrin saturation with iron (find out exactly how much iron the blood carries);
- to monitor the effectiveness of treatment with iron preparations.
The study is carried out if the following diseases and conditions are suspected:
- if there are deviations in the results of the general analysis (hemoglobin level, red blood cells, hematocrit);
- in case of poisoning with salts or drugs (overdose) of iron;
- if iron deficiency is suspected;
- for diseases of the gastrointestinal tract leading to impaired absorption of iron in the small intestine;
- with malnutrition (when the diet lacks iron, and this leads to adverse consequences);
- if you suspect hereditary pathologies accompanied by impaired iron metabolism;
- for various types of bleeding that can lead to the loss of a significant amount of iron (for example, heavy bleeding during menstruation, stomach ulcers and other conditions and diseases).
How to make iron better absorbed
To increase hemoglobin, it is not enough to simply include iron-containing foods in your diet. It is important that the nutrients are absorbed as much as possible and are beneficial. To do this, you should know which products can and cannot be combined with each other.
Iron is best absorbed in the presence of vitamins C and A. That's why seafood with lemon is not only tasty, but also incredibly healthy. A few drops of lemon can be added to salads and other dishes. Almost all fresh vegetables and fruits, such as bell peppers, are rich in vitamin C. Vitamin A is found in fish, oil, vegetables and orange fruits.
It is important to ensure that the body receives folic acid, which takes part in the synthesis of red blood cells. Therefore, you should regularly eat beef, green salad, avocados, legumes, rice, peanuts and other foods high in folic acid.
But calcium and casein (milk protein) reduce the absorption of iron, so you should not consume dairy and fermented milk products and cheeses along with vegetable and meat dishes. Wheat and other grains have a negative effect on the absorption of iron. So it’s better to eat meat without bread, and use vegetables rather than pasta as a side dish. Among the foods that can provoke hemoglobin deficiency: tea, coffee and persimmons (contain tannins), bread, soy, canned food, soda, processed cheese. Therefore, you should not abuse them.
Can there be too much iron in the body?
Maybe. An excess of iron is just as harmful to the body as its deficiency. It causes fibrosis of organs and tissues. The pancreas, liver and heart are most often affected. However, it is impossible to achieve an excess of iron through diet alone. The pathology is often due to genetic predisposition and improper or uncontrolled use of iron-containing drugs.
What is an increase in hemoglobin called?
An increase in the number of red blood cells and an increase in hemoglobin is called erythrocytosis. Its characteristic symptoms: nosebleeds, headaches and dizziness, fatigue. Erythrocytosis, in turn, can be a sign of various diseases, which only a doctor can determine.
What does it mean if hemoglobin is elevated?
High hemoglobin levels can be caused by dehydration, smoking, lung cancer, heart disease and other pathologies. Elevated hemoglobin sometimes indicates the presence of a rare disease - polycythemia. When this happens, the body produces too many red blood cells, which can lead to blood clots, heart attacks and strokes. This is a very serious disease that is important to identify and control early throughout your life.
How to maintain normal hemoglobin levels
For a healthy person without congenital pathologies, it is important to monitor the daily routine, drink enough water, eat a balanced diet, include foods rich in iron and vitamins in the diet, lead an active lifestyle and periodically undergo general and biochemical blood tests.
These tips may seem obvious and even banal to you, but they will help prevent a decrease in hemoglobin, the development of anemia and other diseases, and improve your well-being and quality of life.
This material summarizes the best research on evidence-based medicine over the years. However, it is for informational purposes only, is not intended to prescribe treatment, and cannot be used as a direct guide to action.