Glycated hemoglobin is one of the indicators of a biochemical blood test. Allows you to determine the average blood sugar level over the past three months. In tests it may be referred to as HbA1C or A1C.
Knowing its significance is important in order to promptly identify diabetes mellitus, monitor the course of the disease and the effectiveness of the therapy used.
Who needs to donate blood for glycated hemoglobin and how often?
A blood test for glycated hemoglobin provides basic information about the condition and is much more convenient than other tests; it allows you to identify non-compliance with the diet and poor sugar control on the part of the patient.
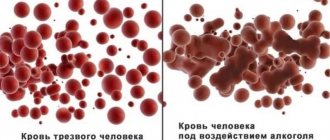
The result is expressed as a percentage. For example, the level could be 6.5%. The number shows the proportion of hemoglobin that has combined with glucose, that is, glycated. Toxins produced as a result of the reaction in excess cause complications in the kidneys, organs of vision and lower extremities. The remaining 93.5% of the substance remains free and continues to deliver oxygen to the tissues.
It is not suitable for detecting gestational diabetes in pregnant women, as it shows an increase in sugar late. The analysis is indicated for women planning to have a child.
For all healthy people, upon reaching 45 years of age, it is enough to measure glycated hemoglobin once every three years. This will help identify type II diabetes at an early stage.
Up to 45 years of age, regular testing is required if you are in a risk group:
- For obesity or being registered as overweight.
- With a sedentary lifestyle.
- If you have close relatives who suffer from diabetes.
- If glucose tolerance or a glycated hemoglobin level of more than 5.7% is detected.
- If you have a diagnosis of arterial hypertension.
- If you had gestational diabetes during pregnancy.
- There is a decrease in insulin sensitivity.
If you are at high risk of developing diabetes, get tested to determine your glycated hemoglobin level at least once a year.
In a well-controlled course, when the indicator can be kept at a level of no more than 7%, the analysis is taken once every 6 months.
At the initial stages of therapy and when changing the treatment regimen, HbA1C is monitored quarterly.
Persons over 60 years of age need to be tested annually, and if their vision and general health deteriorate, or diabetes is suspected, they should be tested immediately.
What is glycohemoglobin (glycolysed or glycated hemoglobin or hemoglobin A1c)?
This is where an analysis for glycohemoglobin (glycated or glycolyzed hemoglobin or, in short, A1c hemoglobin) comes to the rescue. This is a measurement of glucose already bound to hemoglobin, rather than free blood sugar, which can be measured with home glucose meters. Glucose binds to hemoglobin through the Maillard reaction. Normally, the products of this reaction are removed from the body, but if glucose has been increased, then glycated hemoglobin (the reaction product) does not have time to be removed and accumulates in the blood.
What level of HbA1C is considered normal?
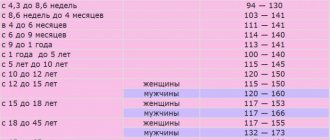
The official norms of the indicator are the same for both men and women. It does not depend on age, with minor exceptions.
A glycated hemoglobin level of up to 5.7% is considered normal. The best indicator is 5.5%.
Finding the result in the range of 5.7% -6.4% indicates the risk of developing type II diabetes mellitus. In this case, it is important to take measures to reduce the likelihood of getting sick and consult a doctor. At levels up to 6%, a switch to a low-carbohydrate diet is required.
An indicator of 5.6-5.9% is considered slightly elevated; there are no symptoms of carbohydrate metabolism disorders, but excess weight may be present.
When the HbA1C level is between 6.1-6.4%, some specialists already diagnose pre-diabetes and prescribe treatment. If the development of the disease is left to chance, then within 6-10 years problems with the kidneys, vision and legs will appear. The risk of death from cardiovascular disease in this case increases by 25%. The prediabetic state requires a transition to a healthy lifestyle.
According to the analysis result showing HbA1C more than 6.5%, diabetes mellitus is possible, but additional studies are required to confirm the diagnosis. As a rule, it is confirmed. The figure of 6.5-7.5% indicates a pathology of moderate severity.
For people with diabetes, it is recommended to maintain the rate at a level of up to 7%. However, keeping the figure within 5.5-5.7% will prolong life and help avoid disability.
An indicator of 8% indicates poor control and rapid development of complications, including loss of consciousness and coma.
Establishing and maintaining normal HbA1C is important to reduce the development of dangerous complications:
- Heart attack and stroke.
- Diabetic retinopathy or neuropathy, kidney damage.
In children with diabetes, it is advisable to maintain a glycated hemoglobin level of 5.4% until adolescence. The figure of 4-5.9% indicates that there is no disease. 6-7% - the course of the disease is well controlled. With an indicator of 7.1%, a serious condition is recorded.
Pregnancy with diabetes
According to modern epidemiological data, more than 2 million patients with diabetes mellitus are registered in Russia, but their real number may reach 8 million people. At the same time, approximately half are women of reproductive age1. Sooner or later, every obstetrician-gynecologist has to face all the difficulties of the reproductive period in this group of patients.
The reform of domestic health care rightly strives to provide highly specialized care in large inpatient departments of multidisciplinary hospitals. Here, next to the obstetrician-gynecologist, there are professional endocrinologists, cardiologists, vascular surgeons, and rheumatologists. Pregnant women with complex extragenital pathology require comprehensive monitoring. When it comes to diabetes, this is the golden rule.
Risks to mother and fetus
Pregnancy with diabetes can only be planned. If we are really interested in the end result. It is important that both the expectant mother and the attending physician understand: pregnancy in a patient with diabetes carries risks for both the woman and the fetus.
glycated hemoglobin is normal during pregnancy
Maybe this story will be useful to someone... It would have been useful to me at one time. The main thing to remember is that nothing critical happened and you shouldn’t be afraid at all!
It all started with the first blood test (biochemistry) when registering with the LCD at about 10 weeks: fasting glucose 6.0. The gynecologist ordered me to retake my glucose level, again on an empty stomach - 5.9. Then I found out that for pregnant women the sugar standards are lower than for an adult, and are up to 5.1 on an empty stomach, up to 7.0 an hour after meals, and seem to be established by the WHO as safe based on the results of many years of research on this topic.
So, the gynecologist referred me for a consultation with an endocrinologist, noting that my sugar was high and there was a risk of GDM. I haven’t complained about sugar before, but it’s a family history; both parents have type 2 diabetes.
To get to the district clinic to see an endocrinologist, you first had to get an appointment with a therapist. EMIAS helps a working person, but making an appointment with him at a convenient time 2 weeks in advance...
The therapist “opened the corridor”, but an appointment with an endocrinologist also took 2 weeks...
That. After about a month I managed to see a specialist doctor. At the appointment, it turned out that the endocrinologists at the district clinic themselves do not have the authority to make a diagnosis of GDM, they are only questionable, and to clarify the diagnosis they are referred to the only (!) medical institution of this profile in the MSK - LC at City Clinical Hospital No. 1 named after Pirogov, at 25 RD .
It took almost another month to get an appointment there, a week and a half to call and make an appointment, and a couple of weeks to wait in line...
As a result, at about 16-18 weeks I received confirmation of the diagnosis of GDM (this was all based on two tests that were taken at the very beginning, I had not retaken anything else by that time, I was not given a glucose tolerance test). A low-carbohydrate diet, a food diary, control of fasting blood glucose and before and after meals, tests (glycated hemoglobin) and a second appearance after 2 weeks are recommended... Looking ahead, I note that from that moment and throughout the pregnancy I was observed by an endocrinologist in the gastrointestinal tract at 25 RD , appearances every 10-15 days.
The epic itself was quite exhausting, hence there was some distrust of the diagnosis. Moreover, nothing bothered me! And I ate whatever I wanted, at first I was especially drawn to sweet soda...
We purchased a glucometer. The first independent measurements of sugar showed that it was really high. I accepted that the diagnosis was correct, but there was a state of confusion, fear for myself and the baby, and a lot of questions: what’s next, why is it dangerous, why did I never complain, etc., etc... I re-read a lot of information about diabetes, I found out that you can live with it, and it’s not even bad, you just have to change your eating habits. And the baby I was expecting became a powerful incentive for this, because her health was at stake!
Then there was almost a month of persistent struggle with sugars by following a strict diet, we managed to achieve good daily sugar levels and after meals no higher than 7.0, but morning (fasting) sugar stood firmly at 5.5-6.0. At the same time, a couple of hours after sleep it fell, and even before breakfast it was already 4.8-5.3... Of course, there were times when I really wanted something tasty, then I could break the diet... But I never broke it critically. And then, occasionally you also need to pamper yourself, I think that the mother’s endorphins are more beneficial for the baby than constant stress due to dietary restrictions. By the way, everyone has a different reaction to the same carbohydrates... My sugar was increased by whole grain bread (if I ate more than 1 piece per meal), and porridge with water (all cereals and oatmeal), and milk, and almost all fruits (if ate as dessert). Fruits were the most offensive thing for me... You could only eat 1 apple or 1 pear in a separate meal, like a second breakfast or afternoon snack... And of course, no “quick” ones, i.e. easily digestible carbohydrates: sugar, sweet dishes, baked goods, juices, desserts, etc. What was surprising was that cottage cheese with medium and high fat content increased sugar less than low-fat cottage cheese, although everything is logical, it is easier to digest...
In general, the diet began to consist of vegetables and protein, I ate carbohydrates in minimal quantities, because you can’t live without them at all, ketones may appear in the urine... The main rule that saved me when eating: start with vegetables. Then the sugar rises less than if you eat the same vegetables in the middle or end of the meal. For example, if I started lunch with grated carrots and not with soup, then the sugar was almost 0.5 lower than if I started with soup, and this was always the case with any raw vegetables. Cucumbers, tomatoes and lettuce have become permanent residents of our refrigerator.
It was not possible to reduce morning sugar with diet; it remained at the level of 5.6-6.0, and at approximately 22-23 weeks the endocrinologist prescribed insulin Levemir. This is a “long” insulin, with a long period of absorption by orgasm, which needs to be injected. It does not pass through the placenta and is not dangerous for the baby; pregnant women should not take any diabetic pills. To say that I was afraid to start injecting him is an understatement, it was a shock... But I had to somehow reduce (compensate) the level of my morning sugar!
Here I want to make a digression and explain why this GSD is generally dangerous, as I understand for myself.
It is not for nothing that it is gestational, i.e. arising (or first identified) during pregnancy (gestation) - apparently the placenta and the hormonal background changing during pregnancy are to blame. In the first half of pregnancy, the danger is that due to the mother’s elevated sugar levels, a favorable environment is created for the baby to gain excess weight. Large babies are more difficult to give birth to and there are more risks to their health. And in the second half of pregnancy, when the baby’s organs begin to function, an increased load is added to the baby’s pancreas; it begins to intensively produce insulin, which the mother’s pancreas cannot cope with. “Getting used to” working for two, there is a risk of hypoglycemic coma immediately after the birth of a child, because his gland, coping with sugars from the mother, produces insulin in an increased volume, quickly processes all its own sugar and a sharp drop in blood sugar levels can occur, leading to coma. It is dangerous for the baby in the future due to all sorts of bad things, in particular, disturbances in the functioning of the pancreas and diabetes. Taking all this into account, there was no question of whether to inject or not to inject for me, but it was scary...
So, the prescribed Levemir was given free of charge at the place of residence in the district clinic, after visiting the district endocrinologist.
The dosage was also not selected immediately, it took about a week and a half, starting with 8 units once a day in the evening, and gradually reaching 12 units. Sugar became 4.9-5.1 in the morning.
The form of release of the medicine (syringe pen) is very convenient, you twist a disposable thin needle, measure out the required dosage and inject it subcutaneously into the skin fold (pinching the skin with two fingers). It just sounds scary, but in reality it didn’t hurt at all and there was no blood. Usually injections are given in the thigh (lateral surface) or stomach. Apparently, I have more fat on my thighs, so sometimes the medicine got into the fatty tissue, from there it took longer to dissolve and the morning sugar could be higher, so I liked the injection in the stomach more. At the same time, the diet was followed as before.
This continued until about 30-32 weeks, I got used to it and relaxed a little, I began to pamper myself with treats more often, already knowing that the main thing is not to overindulge. And then the figures for morning sugar and after eating slowly crept up.. True, after eating the increase was not critical, up to 7.5 maximum, once up to 8.5 if the diet was violated. I note that regarding the placenta, i.e. to the child, the sugar level goes above 7.6, in my opinion, or even higher.
Because From the very beginning, I kept a glycemic diary (by this time, with the permission of the endocrinologist, I was no longer writing down what I was eating, but simply noting the sugar on an empty stomach and after meals), based on these indicators, the endocrinologist in the LCD at 25 RD prescribed me an increase in the dose of levemir, first to 15 units , then until 17, and also prescribed Novorapid (this is “fast” insulin, injected with food immediately before meals). At the same time, from the explanations, I understood that the increase in sugar levels is associated with the growth of the placenta and further changes in hormonal levels...
I received novorapid at the clinic, but began to try not to break my diet, and my sugar level no longer increased after eating. But NovoRapid came in handy: when it became unbearable and you wanted something sweet, you could afford it, having first given an injection, 5-7 units, and the sugar did not rise above 7. Looking ahead, I will say that NovoRapid was also useful in the maternity hospital, because hospital food I was completely without fresh vegetables and contained a lot of “fast” carbohydrates, and I was in the maternity hospital for a long time and needed to eat something))).
Morning sugar also remained at the level of 4.8-5.1 until hospitalization in the RD, which is scheduled for pregnant women with GDM at 39 weeks, i.e. in advance, to conduct examinations and choose the right delivery tactics.
In MSC there are only 2 maternity hospitals where diabetics give birth, these are 29 and 25. I chose 25, partly because I was observed in the residential complex with him, partly because, according to reviews, it has one of the best children's intensive care units, while I have The words about the risk of a hypoglycemic coma in a baby after childbirth were so ingrained in my memory that, despite my compensated sugar levels, I didn’t want to risk it.
As a result, at the direction of the endocrinologist from the LC at 25 RD, I went to the RD for a planned hospitalization at week 39, taking with me all the insulins and a glucometer, continuing to measure my sugar and give injections. The story of staying in the maternity hospital is a separate story about childbirth, I’ll just say that I was not disappointed in choosing the maternity hospital, my sugar levels even dropped a little (I think because of the regime, because at home I ate irregularly, had dinner often late, and in the RD dinner was at 6:00 p.m. or earlier, by 10 p.m. I was already starting to get ready for bed, and at 11 p.m. I was usually lying down, because there wasn’t much to do there in the evenings, I was studying the Internet and preparing for childbirth).
As a result, I gave birth on my own (with stimulation), a girl, height 56, weight 3660, not at all large as I was told by ultrasound. My sugar levels were normal during the birth process, after giving birth both my baby’s sugar levels were also normal and now everything is fine.
After giving birth, you immediately stop injecting insulin, and right in the maternity hospital I began to gradually eat fast carbohydrates, I really missed them (at first tea with sugar, porridge with milk, a piece of bread and butter, then my husband brought marshmallows, biscuits, etc.) . My sugar didn't go up! It was so strange, because before that, any piece of white bread had to be injected with insulin... I didn’t think that immediately after giving birth (as the placenta would be gone), my sugar levels would immediately return to normal, and the numbers became almost better than they were before. insulin: on an empty stomach up to 5, after meals up to 6.5. By the way, for postpartum women the sugar norms are already different: on an empty stomach up to 6.0, after eating 2 hours later up to 7.8. It's called, feel the difference)))
Well, as a bonus: during pregnancy I gained only 7 kg, and after giving birth I lost 10 kg relative to my pre-pregnancy weight. I'm a big girl, and it turned out to be quite good)))
What I want to say in conclusion: now I know that there is no need to be afraid, you need to gather your will into a fist, follow a diet, listen to what the doctors say, listen to your own feelings, and most importantly, remember every minute why and for whom you are doing all this. For me, the baby’s health was such a powerful incentive that I did not experience any severe discomfort from GDM and the restrictions associated with it. Of course, there are a lot of examinations, ultrasounds, diet, tests, injections, etc., but you take it for granted. It’s good that I had a compulsory medical insurance policy, otherwise it’s difficult to imagine the total cost of all the tests and consultations...
Yes, you also have to believe that everything will be fine, because thought is material!)
Indications for insulin therapy, recommendations of the Russian national consensus
Sulfonylurea drugs (glibenclamide, glimepiride) penetrate the placental barrier and can have a teratogenic effect, therefore they are not used for GDM.
- Failure to achieve target plasma glucose levels
- Signs of diabetic fetopathy by ultrasound (indirect evidence of chronic hyperglycemia [13])
- Ultrasound signs of diabetic fetopathy:
- large fetus (abdominal diameter greater than or equal to the 75th percentile);
- hepatosplenomegaly;
- cardiomegaly and/or cardiopathy;
- dual-circuit head;
- swelling and thickening of the subcutaneous fat layer;
- thickening of the neck fold;
- newly identified or increasing polyhydramnios with an established diagnosis of GDM (if other causes are excluded).
When prescribing insulin therapy, a pregnant woman is treated jointly by an endocrinologist (therapist) and an obstetrician-gynecologist.
Treatment during pregnancy
Treatment of GDM is a complex and complex task. The drugs are selected so as not to harm the fetus. And treatment, if necessary, can continue after childbirth.
Diet
Following a special diet is the first step towards getting rid of gestational diabetes. Drug treatment for GDM will not be effective without diet. What you need to pay attention to:
- It is necessary to exclude fast carbohydrates (sweets, pastries, white bread, cakes, fruits), and also limit fats,
- There should be several meals, you should eat every 2-3 hours,
- You should consume enough protein and reduce your intake of foods high in starch (rice, bread, pasta, potatoes, corn),
- It will be useful to increase the consumption of vegetables and herbs, vegetable oils and other foods rich in unsaturated fats,
- It is important to maintain a balance of proteins, carbohydrates and fats, as well as monitor the caloric content of your diet.
Important! You can’t prescribe your own diet! It should be compiled by a specialist taking into account the needs of the expectant mother and baby.
In addition to dietary changes, incorporate moderate, regular physical activity into your daily routine. Exercise at least 150 minutes a week; swimming is very beneficial.
Blood Sugar Tracking
The second step in the fight against GDM is daily monitoring of blood sugar. It is needed to understand whether the diet helps.
To determine your glucose, you do not need to go to the doctor; for this there is a special device - a glucometer (Fig. 3).
Figure 3. A set of a glucometer, a skin-piercing pen, a set of test strips and needles for a cartridge pen. Source: WikiMedia
With its help, patients with GDM check their glucose levels on an empty stomach and 1-2 hours after meals every day for a week, recording the data in a journal. Based on the results obtained, the endocrinologist decides whether drug treatment is required, or whether GDM has already been controlled through dietary restrictions. Medicines are prescribed if one third or more of the results indicate glucose levels:
- on an empty stomach - more than 5.3 mmol/l,
- an hour after eating - more than 7.2-7.8 mmol/l,
- 2 hours after eating - more than 6.5 mmol/l.
Sometimes your doctor will also ask you to keep a diary of your blood pressure, body weight, and nutrition. You can also monitor sugar in your urine using test strips.
Important! Devices without a needle have already appeared - it is replaced by a sensor in the form of a patch that is glued to the skin. The glucometer reads its readings continuously. You can configure the device so that the data is sent to your mobile phone or immediately sent to the doctor.
Drug treatment: insulin
To control glycemic levels, hypoglycemic drugs are prescribed:
- In case of uncontrolled glycemia and the presence of fetopathy, insulin is used first. It is safe for the fetus; the dose and mode of administration are determined by the endocrinologist on an individual basis.
- In some cases, an insulin pump is installed for better glycemic control.
- Tablets of hypoglycemic drugs are used strictly according to indications.
During treatment, blood sugar control is not interrupted; all data on drug doses and blood glucose levels are recorded so that the doctor can adjust the dosage regimen.
Important! Insulin is considered the best treatment for GDM. To date, there is not enough data to judge the delayed effects of other glucose-lowering drugs.
Benefits of HbA1C testing
Currently, the HbA1C test is also used to diagnose diabetes, although previously the test was prescribed only for monitoring already diagnosed patients. Endocrinologists believe that the HbA1C test is in many ways better than the traditional fasting glucose test or oral glucose tolerance test for diagnosing diabetes.
Its advantages::
- simplicity;
- ability to perform at any time of the day;
- does not require preparation and abstinence from food;
- only one blood sample is needed;
- reliability in both diagnosing and predicting the risk of some chronic complications of diabetes.
The blood for the test can be taken either from a vein (venipuncture) or from a finger, depending on whether the test is done in a laboratory or in a doctor's office (or at home).
Who's at risk
Risk factors for gestational diabetes
| Risk factor | Consequences |
| Mother's age is over 40 years old | Large fruit |
| Maternal obesity, or excess body weight | Polyhydramnios |
| History of gestational diabetes | Excessive weight gain during current pregnancy |
| History of early or late gestosis | Congenital malformations of the fetus |
| Diabetes mellitus in close relatives | Excretion of glucose in urine |
| History of miscarriage or stillbirth | |
| Diseases and conditions that can provoke the development of diabetes (metabolic syndrome, polycystic ovary syndrome, high blood pressure, high cholesterol) | |
| Multiple pregnancy |
Management of patients with GDM
Within 1–2 weeks after diagnosis, the patient is advised to be monitored by obstetricians-gynecologists, therapists, and general practitioners.
Rules for conducting an oral glucose tolerance test (OGTT)
- The test is carried out against the background of normal nutrition. At least 150 g of carbohydrates should be consumed per day for at least three days before the study.
- The last meal before the test should contain at least 30–50 g of carbohydrates.
- The test is performed on an empty stomach (8–14 hours after eating).
- Drinking water before the test is not prohibited.
- You are not allowed to smoke during the study.
- The patient must sit during the test.
- If possible, on the eve of and during the study, it is necessary to avoid taking medications that can change blood glucose levels. These include multivitamins and iron supplements, which contain carbohydrates, as well as corticosteroids, beta blockers, beta adrenergic agonists.
- OGTT should not be performed:
- with early toxicosis of pregnant women;
- if necessary, on strict bed rest;
- against the background of an acute inflammatory disease;
- with exacerbation of chronic pancreatitis or resected stomach syndrome.
Recommendations for a pregnant woman with diagnosed GDM according to the Russian national consensus:
- Individual correction of the diet depending on the woman’s body weight and height. It is recommended to completely eliminate easily digestible carbohydrates and limit the amount of fat. Food should be distributed evenly over 4-6 meals. Non-nutritive sweeteners can be used in moderation.
For women with a BMI >30 kg/m2, average daily caloric intake should be reduced by 30–33% (approximately 25 kcal/kg per day). It has been proven that this measure can reduce hyperglycemia and plasma triglyceride levels [12].
- Aerobic physical activity: walking at least 150 minutes per week, swimming.
- Self-monitoring of key indicators:
- glucose level in capillary blood on an empty stomach, before meals and 1 hour after meals;
the level of ketone bodies in urine in the morning on an empty stomach (before bedtime or at night, it is recommended to additionally take carbohydrates in an amount of about 15 g for ketonuria or ketonemia);
- arterial pressure;
- fetal movements;
- body mass.
In addition, the patient is recommended to keep a self-monitoring diary and a food diary.