Pseudocyst of the brain in newborns and adults
Cystic pseudocysts are cavity formations with liquid contents and a thin wall that limits the size of the structure.
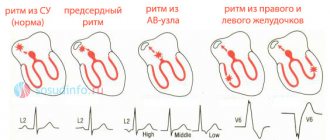
The false cavity differs from the true analogue by its formation from the germinal matrix, which is clearly visible on MRI of the brain. Nosology refers to developmental anomalies. The most common location of a cystic cavity formation is between the head of the caudate nucleus, the optic thalamus, and the lateral angles of the lateral ventricles. In adults, the main cause of cystic cavities is brain infections (Toxoplasma, Cryptococcus).
What is a subepindymal cyst?
In newborns, hemorrhages from the damaged vessel wall, localized under the ependyma, are not multiple. Usually one or two cavities containing blood are found. Gradually, the blood clots dissolve, and the vacated space is filled with cerebrospinal fluid (CSF). Formations are recorded by neurosonogram until the fontanelles close after the birth of the child.
Minor hemorrhages do not affect the functionality of the brain. There is no infection of the formations. Multiple subependymal pseudocysts do not cause neurological disorders.
Some doctors consider early closure of the fontanelles of the skull in an infant to be the reason for the long-term persistence of pseudocysts. For this reason, the child is contraindicated in taking vitamin D3, which accelerates the calcification of cartilage tissue. Physiologically, the closure of the large fontanel occurs by twelve months.
Most experts do not consider the relationship between fontanelles and brain cysts to be real. There are no objective studies confirming the presence of a relationship between nosologies.
Subepindymal pseudocysts are small (up to 4 millimeters), medium and large (about 10 mm) in size. Small cavities in children disappear on their own by the age of one year. Medium and large formations can provoke irritation of the nearby parenchyma, and therefore persist for a long time (up to 6 years). If electroencephalography reveals increased excitability of the cerebral cortex, medications are prescribed.
The localization of the subependymal cyst determines the clinical picture:
- A space-occupying formation in the back of the head is characterized by damage to the visual centers;
- Cerebellar cavity – dysfunction of the motor sphere;
- Cyst of the temporal region - hearing damage;
- Pituitary pseudocyst – endocrine imbalance.
The side of the lesion determines the location of the lesion - right or left.
What is the difference between a pseudocyst and a cyst?
A cavity formation containing cerebrospinal fluid in the central part, which occurs after the birth of a child, in adults causes clinical symptoms and is capable of progression.
Pseudocysts form in utero or directly during childbirth. The soft bones of the baby's skull, when moving along the birth canal, can cause excess pressure on the brain tissue. Lack of oxygen supply (hypoxia) leads to the formation of cystic cavities as a result of rupture of blood vessels. Gradually, such cavities resolve.
False cystic cavities are formed under the influence of the following etiological factors:
- No genetic predisposition;
- Multichamber cavities of the lateral ventricles arise due to abundant vascular ruptures;
- Pseudoformations are localized between the caudate nucleus and the optic thalamus.
The absence of damage to the tissue of the lateral ventricles and periventricular space is not accompanied by clinical symptoms.
Concept
All cysts have a similar structure - they are cavities in which fluid is located - and can form in different parts of the body.
A subependymal cyst forms in the brain under the influence of one or more unfavorable factors.
Small cystic formations do not cause significant negative consequences and resolve on their own over time , but large cysts that are poorly located require increased medical supervision.
What are the consequences of cephalohematoma in newborns? Find out about this from our article.
Types of true brain cysts
There are several types of cerebral cystic cavities:
- Pathological manifestations of cystic cavities of the retrocerebellar space arise due to damage to the thickness of the brain tissue. Damage to the cerebral parenchyma occurs due to circulatory disorders, inflammatory processes (encephalitis, meningitis), after surgical interventions. Retrocerebellar cavities increase with repeated infections and bleeding;
- Arachnoid cysts are localized between the membranes. In children, education may have a congenital etiology. In adults, it forms after injury or inflammation. The danger of the arachnoid cavity lies in compression of the brain parenchyma, which is accompanied by an increase in intracranial pressure;
- The pineal cystic cavity is localized between the hemispheres. Damage to the area of the pineal gland is accompanied by disturbances in hormonal metabolism. The cause of the nosology is duct blockage, echinococcal damage;
- Subarachnoid intracerebral cyst has a congenital etiology. The clinical picture of the formation is characterized by intracranial pulsation, a feeling of instability, and muscle cramps. Diagnosis of formation is carried out using magnetic resonance imaging;
- An epiphyseal cyst of the brain is accompanied by drowsiness, disorientation in space, and double vision of objects. The symptoms are varied, but signs of damage to the pineal gland predominate. An abnormal structure is detected using magnetic resonance imaging. If the cavity is large, surgery is required to decompress the brain structures;
- Choroid plexus cyst is a type of pseudocyst. Detected by neurosonography of a pregnant woman;
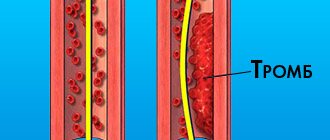
- The lacunar cyst is located in the pons and subcortical structures. The main cause in older people is atherosclerosis of the arteries of the brain;
- Pineal cystic cavity is an etiological factor in the disorder of metabolic processes and motor activity. Pathology causes encephalitis and hydrocephalus;
- A limited cerebrospinal fluid cavity is located between the meninges. Etiological factors of nosology are injuries, inflammatory processes, strokes. The formation causes leg paralysis, muscle cramps, psychosis, and a gag reflex;
- Porencephalic cystic cavity is the result of past infections. The nosology is dangerous due to the development of hydrocephalus and increased intracranial hypertension. Some scientists argue about the hereditary etiology of education, as it is found in children after birth.
The described types differ from pseudo-formations on tomograms by establishing a specific location of the cavities.
Qualitative approach to therapy
Treatment of a cerebral cyst is aimed at preventing its growth. To do this, you need to find and eliminate the main cause that provokes oxygen starvation. During certain life stages of a child's growth, medical care will vary.
First aid
After birth, a neonatologist performs resuscitation care.
Removes fluid from the respiratory tract, stimulates artificial respiration; in severe cases, an oxygen mask is used to supply pure oxygen.
The first three days after birth...
A neurologist conducts a daily examination and prescribes a restorative course of medication and rehabilitation therapy. Massage, physical therapy and sedatives are prescribed.
In childhood, the doctor observes the dynamics of the child’s development rate.
Medicines are used to stimulate speech functions and normalize the psycho-emotional state. At this stage, you may need the help of specialists such as a speech therapist and a psychologist.
...and beyond
When a child reaches adolescence, vitamin medications are prescribed to stimulate brain function and normalize metabolism. It is also necessary to take hormone replacement medications.
All physiotherapeutic and medicinal methods are prescribed only after the results of the examination and identification of deviations in the child’s development.
Causes of cerebral pseudocysts
Scientists were unable to establish the etiological factors of cystic intracerebral cavities. Verification of provoking mechanisms of development in children has been established by practice. Pathology is most often formed due to problems passing through the birth canal. Prenatal ultrasound does not indicate pseudocysts.
True cysts can be detected up to 28 weeks. Then they regress on their own.
Problems arise in children due to cerebral hemorrhage, hypoxic conditions, and cerebral circulatory pathology.
Subepindymal pseudocysts in newborns and infants are associated with the birth process, but are not congenital. Complications arise due to concomitant hemorrhages.
Pseudocyst of the choroid plexus of the right lateral ventricle
The development of cystic cavities of the choroid plexus is observed at 13-18 weeks. By this time, a mesh structure is formed inside the choroid. After filling the formation with liquid, cavities with the presence of cerebrospinal fluid are visible on ultrasound. By the twenty-eighth week of pregnancy, the cysts disappear on their own. Pseudoformations of the right ventricular plexus after birth are found during complicated pregnancy:
- Hypoxia of fetal brain tissue;
- Infections (herpes, chlamydia, cryptococcal).
The choroid plexuses in the fetus form in the sixth week. In the absence of nerve cells, fluid formation abnormalities may occur. Drops of cerebrospinal fluid after contact with the structures of the choroid plexuses lead to the formation of additional cystic cavities.
Pseudoformations of the left and right sides are equally likely to develop. Most of it resolves by 28 weeks. The pathology is formed at the beginning of intensive fetal development, when there are temporary disturbances in embryogenesis. By birth, brain function is normalized. If the formations persist after birth, the nosology usually disappears within a year.
The danger comes from the combination of pseudocysts with other brain changes:
- Diaphragmatic hernia;
- Trisomy 18 chromosomes;
- Diaphragmatic hematoma;
- Micrognathia;
- Omphalocele;
- Hydrocephalus;
- Cystic hygroma;
- Neural tube defects;
- Hammer feet.
In the presence of combined disorders, amniocentesis is performed - this is the removal of amniotic fluid for subsequent study of chromosomes. Pseudocysts with additional stigmas of disembryogenesis develop in a number of hereditary diseases (Down, Edward).
Amniocentesis is considered safe for the child, but the procedure is invasive, so it is performed according to indications.
A comprehensive examination involves the use of additional neuroimaging methods:
- Neurosonography;
- Magnetic resonance imaging (MRI);
- Computed tomography (CT).
Ultrasound examination is possible in full-term infants, when the fontanelles are covered with thin bone tissue. In newborns, the lumens are open to ultrasound rays. MR and CT angiography methods are used to examine cerebral vessels after intravenous administration of a contrast agent.
Pathology
WHO classification:
1. Nonanaplastic (low grade of malignancy)
2. Papillary: “classic lesion” of the GM and SM. Metastasis is possible up to 30%.
3. Myxopapillary ependymoma: a separate form, found only in the area of the filum terminale. Papillary ependymoma with microcystic vacuoles and mucous contents.
4. Subependymoma
5. Anaplastic: pleomorphism, multinucleation, giant cells, mitoses, vascular changes, areas of necrosis (sometimes when anaplastic changes are more pronounced, the term ependymoblastoma is used, but this term should be reserved for a separate type of tumor, rare primitive neuroectodermal tumors in children). Whether the degree of anaplasia influences outcomes is unclear.
Features of symptoms of pseudocysts in adults and newborns
In an adult, multiple cystic cavities rarely form. Single cavities do not pose a health hazard if they are not infected, and there is no increase during follow-up. True cysts in adults are diagnosed more often, which is caused by skull injuries, infectious diseases, and inflammatory processes.
Features of pseudocysts in a newborn baby
Diagnosis of pseudocystic formations is carried out in one child out of a hundred. After birth, an ultrasound examination (ultrasound) is prescribed for all premature babies, in case of complicated childbirth, or difficulties passing through the birth canal.
Oxygen starvation of the brain in utero develops after a woman experiences stress during pregnancy, infections, or the use of medications while bearing a child.
Pseudocysts of the choroid plexus are detected at 14 weeks of intrauterine development. To preliminarily identify and carry out dynamic monitoring of formations, ultrasound is performed in the first trimester of pregnancy.
Why are choroid plexus cysts dangerous in a child?
The first signs of the formation of the hemispheres during embryogenesis are the formation of choroid plexuses. The process of formation of restricted cerebrospinal fluid within the structures has not been studied. Pseudocysts do not pose a health hazard and therefore do not require urgent treatment. Dynamic observation and maintenance therapy accelerate the process of spontaneous resorption of cavities.
In most cases, pseudocysts are not dangerous. The absence of an increase in size during dynamic observation leads to positive prognosis. Growing formations that arise after heavy bleeding are dangerous. Such structures belong to the type of true cysts.
Prognosis after surgery
Life after treatment for ependymoma largely depends on the stage of the disease. If the disease is diagnosed in time and treated appropriately, the survival rate for more than 5 years is 70%. A less favorable prognosis is present with an anaplastic tumor, which can grow rapidly and metastasize. In this case, the chances of life are not great, and the treatment provided will prolong life by 1 - 2 years. If surgery is not possible, supportive care may increase life expectancy by just a few months.
If the operation fails to completely remove the tumor, there is always a risk of its recurrence. In such cases, the prognosis worsens, and the risk of its metastases to other organs and systems increases significantly. Unfortunately, there are no preventive measures that can protect against brain cancer. However, if you follow some rules, you can reduce tumor formation:
- proper and healthy nutrition;
- rejection of bad habits;
- eliminate the effects of radiation on the body;
- undergo regular medical examinations;
- monitor the state of the immune system.
By following basic rules, you can significantly reduce the risk of any cancer. Ependymoma is a type of brain cancer that requires timely diagnosis and quality treatment. By treating this pathology in the early stages of the disease, the chance of a positive prognosis is quite good, and the patient himself has the opportunity to return to a full life.
Diagnosis of cysts and pseudocysts of the brain
Ultrasound scanning of the brain parenchyma is a safe and informative diagnostic method. Indications for examination:
- Hypoxic conditions;
- Traumatic brain injury;
- Complication of childbirth;
- Restless behavior of the baby;
- Suspicion of pathology of intracerebral circulation.
Detection of pseudocystic cavities in newborns is not difficult. If the fontanelles become overgrown, tissue examination is carried out using computed tomography and magnetic resonance imaging (CT and MRI).
Headaches, dizziness, muscle cramps with the combined presence of cystic cavities require combined diagnostics using neuroimaging methods:
- Positron emission tomography (PET);
- Neurosonography;
- Doppler encephalography;
- Cerebral scintigraphy;
- Computed tomography and MRI of the head.
A comprehensive study reveals concomitant pathology that occurs during complicated pregnancy or childbirth. Using intravenous administration of a contrast agent, the condition of the cerebral arteries is monitored, areas of hemorrhage and hematomas are identified.
If chromosomal abnormalities are suspected (Edward's disease, Down's disease), amniocentesis is performed - taking material from the amniotic fluid for genetic examination.
Treatment
Surgical resection
The purpose of the operation: maximum removal of the intracranial part of the tumor without neurological deficit. If there is significant tumor invasion into the bottom of the fourth ventricle, then it is completely impossible to remove it. After surgery, radiation therapy and myelography are performed to exclude possible metastasis. 10 ml of cerebrospinal fluid is sent for cytological examination to determine the number of malignant cells (if any) and can also be used as a way to monitor the effectiveness of treatment.
Radiation therapy
Ependymomas are second in radiosensitivity after medulloblastomas. Radiation therapy is prescribed after surgical removal of the tumor (survival improves after radiation therapy in the postoperative period: survival of 50% of patients was 2 years longer with radiation therapy than without it, while the number of patients who had a 5-year survival period increases from 20 -40% to 40-80%)