© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
The right aortic arch in the fetus is a congenital heart defect, which can occur alone or be combined with other, sometimes severe, defects. In any case, during the formation of the right arch, disturbances in the normal development of the fetal heart occur.
The aorta is the largest vessel in the human body, the function of which is to move blood from the heart to other arterial trunks, up to the arteries and capillaries of the whole body.
Phylogenetically, the development of the aorta undergoes complex changes during evolution. Thus, the formation of the aorta as an integral vessel occurs only in vertebrates, in particular in fish (two-chamber heart), amphibians (two-chamber heart with an incomplete septum), reptiles (three-chamber heart), birds and mammals (four-chamber heart). However, all vertebrates have an aorta, into which arterial blood mixed with venous, or entirely arterial, flows.
During the process of individual development of the embryo (ontogenesis), the formation of the aorta undergoes changes as complex as the heart itself. Starting from the first two weeks of embryo development, there is an increased convergence of the arterial trunk and the venous sinus, located in the cervical part of the embryo, which subsequently migrated more medially, towards the future thoracic cavity. The arterial trunk gives rise not only to two ventricles subsequently, but also to six branchial (arterial) arches (six on each side), which, as they develop, within 3-4 weeks, are formed as follows:
- the first and second aortic arches are reduced,
- the third arch gives rise to the internal carotid arteries that supply the brain,
- the fourth arch gives rise to the aortic arch and the so-called “right” part,
- the fifth arc is reduced,
- the sixth arch gives rise to the pulmonary trunk and the arterial (Botallov) duct.
The heart becomes completely four-chambered, with a clear division of the cardiac vessels into the aorta and pulmonary trunk, by the sixth week of development. A 6-week embryo has a fully formed, beating heart with large vessels.
After the formation of the aorta and other internal organs, the topography of the vessel looks like this. Normally, the left aortic arch begins from the aortic bulb in its ascending part, which, in turn, originates from the left ventricle. That is, the ascending part of the aorta passes into the arch approximately at the level of the second rib on the left, and the arch bends around the left main bronchus, heading posteriorly and to the left. The uppermost part of the aortic arch projects onto the jugular notch just above the upper part of the sternum. The aortic arch goes down to the fourth rib, located to the left of the spine, and then passes into the descending part of the aorta.
In the case when the aortic arch “turns” not to the left, but to the right, due to a failure in the formation of human vessels from the branchial arches of the embryo, they speak of a right-sided aortic arch. In this case, the aortic arch extends through the right main bronchus, and not through the left, as it should normally be.
What you need to know about the right aortic arch
- In men and women, these anomalies occur equally often.
- Anomalies in the development of the aortic arch are detected in approximately 1% of the population
- Disruption of the process of obliteration of symmetrical branchial arterial arches and dorsal aorta. There are several possible types of aortic anomaly:
Right aortic arch
- with aberrant origin of the left subclavian artery as the last branch of the aortic arch, arising after the left carotid artery, right carotid and right subclavian arteries
- This is the most common option
- Usually not combined with other congenital heart defects (10% of cases)
- It is not clinically manifested.
Right aortic arch
- with a mirror origin of the branches of the arch (left subclavian artery, left carotid artery, right carotid and right subclavian arteries)
- Often combined with congenital heart defects (90% of cases).
Duplication of the aortic arch:
- the carotid and subclavian arteries depart from the arches of their side
- Both arches merge behind the esophagus to form the descending aorta, located in the midline
- More often (in 75% of cases) there is a dominant right aortic arch and a left-sided descending aorta.
Why does vice occur?
Any malformation is formed in the fetus if a woman is influenced by negative environmental factors during pregnancy - smoking, alcoholism, drug addiction, ecology and unfavorable background radiation. However, genetic (hereditary) factors play an important role in the development of the child’s heart, as well as existing chronic diseases in the mother or past infectious diseases, especially in the early stages of pregnancy (influenza, herpes infection, chickenpox, rubella, measles, toxoplasmosis and many others) .
But, in any case, when any of these factors influence a woman in the early stages of pregnancy, the normal processes of ontogenesis (individual development) of the heart and aorta, formed during evolution, are disrupted.
So, in particular, the period of pregnancy of approximately 2-6 weeks is especially vulnerable to the fetal heart, since it is at this time that the formation of the aorta occurs.
Which method of diagnosing the right aortic arch to choose: MRI, CT, ECHO-CG, angiography
Selection Methods
- KTA,
- MRA.
What will a chest x-ray show in the right aortic arch?
Right aortic arch:
- There is no aortic arch on the left side
- The aortic arch is located on the right in the paratracheal position, forming a depression on the trachea and pushing it to the left.
Duplication of the aortic arch:
- two arches of the aorta are located on either side of the trachea and esophagus
- The trachea is located in the midline and is compressed by the dominant arch (the right aortic arch is usually larger than the left and located higher)
- The descending aorta is located in the midline
- The trachea and esophagus at the level of the aortic arch are pushed anteriorly.
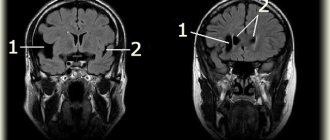
What will MRI and MSCT images of the heart show in the right aortic arch?
- Using these research methods, it is possible to obtain a clear picture of the aortic anomaly and identify concomitant congenital malformations
- In aortic arch duplication, axial images show how both arches arise from the ascending aorta, envelop the trachea and esophagus, and each arch gives rise to one carotid and one subclavian artery.
Plain chest x-ray of a 25-year-old man with a right aortic arch. There is no aortic arch on the left side. But it is present on the right in the paratracheal position, and is located unusually high, slightly pushing the trachea to the left. The descending aorta is located on the right.
Diagnosis of pathology
Vascular pathologies are one of the most common causes of disability in young people. Making a clinical diagnosis of aortic lesions requires additional research methods presented in the table:
| Name of the survey | The essence of the method | What allows you to determine |
| Duplex scanning (ultrasound) of the aortic arch |
|
|
| Aortography |
|
|
| Multislice computed tomography (MSCT) |
|
|
| Magnetic resonance imaging (MRI) |
|
|
The choice of method is determined by the patient’s complaints and age:
- Ultrasound is recommended for children;
- for adults, an MRI examination is considered the “gold standard”.
Before using contrast agents, the doctor must test for allergic reactions to dyes. Ignoring the order leads to life- and health-threatening consequences.
Contraindications to the use of contrast methods:
- allergy to dyes (the most common preparations contain iodine);
- renal failure;
- breastfeeding (allowed 48 hours after the procedure);
- blood clotting pathologies (hemophilia, thrombocytopathy and others);
- severe conditions of the patient (post-resuscitation illness, shock, agony);
- thyrotoxicosis;
- diabetes mellitus type II;
- high level of creatinine in the blood (a marker of impaired renal excretory function).
Clinical manifestations
Typical symptoms of aortic abnormality:
- A right aortic arch with an aberrant origin of the left subclavian artery is usually not clinically apparent
- Clinical symptoms in the form of stridor, recurrent respiratory tract infection and dysphagia associated with compression of the trachea and esophagus appear with a duplication of the aortic arch, a right-sided descending aorta with a left ductus arteriosus and an anomalous right subclavian artery (a. lusoria)
- These symptoms usually appear in early childhood.
Causes of aortic enlargement
Congenital systemic connective tissue diseases: Marfan syndrome, Ehlers-Danlos syndrome, caused by genetic changes in which the aortic wall has an abnormal structure, can cause the development of an aneurysm.
Acquired diseases that cause aneurysmal changes in the aortic wall: most often this is atherosclerosis. About 80% of all complicated aortic aneurysms are aneurysms caused by an atherosclerotic process, which leads to weakening of the vessel wall and the inability to withstand normal blood pressure, and as a result, to its expansion.
Less commonly, an aortic aneurysm develops in inflammatory diseases caused by external agents (syphilis, fungal infection, tuberculosis) or in autoimmune diseases (nonspecific aortoarteritis).
Symptoms of aortic aneurysm
Unfortunately, the diagnosis of aortic aneurysm cannot always be established during the “cold period” (before complications develop), since this disease is usually asymptomatic. Most often, it is discovered accidentally during fluorography, ultrasound or tomography studies performed in connection with other diseases. Treatment of an aneurysm of the ascending aorta before complications develop is much safer for the patient, therefore, in the early diagnosis of an aortic aneurysm, routine medical examination is important.
It is worth noting that every hundredth patient who died suddenly dies from aortic dissection.
Complaints usually appear when the aneurysm begins to stratify or, enlarging, compresses surrounding organs and tissues. Pain or dysfunction of those organs located in the area of the aneurysm appears. At first, this is not of a bright nature and, therefore, does not alarm either the patient or the doctor.
However, the pain intensifies as these deadly complications of an aortic aneurysm develop—it is some of the most severe pain a person can experience. It is localized in the chest if the aneurysm is located in the ascending, descending sections or in its arch, or in the abdomen if it formed in the abdominal section. Characterized by severe weakness, pallor, and often the person loses consciousness.
Impaired blood supply to organs located in the area of aneurysm rupture or aortic dissection (brain or spinal cord, kidneys, intestines, upper or lower extremities) leads to loss of function of these organs, and a large volume of blood loss during aortic rupture represents the most serious danger. To save a life, minutes count. If early surgical treatment is not available, the first-day mortality rate for aortic dissection is 1% per hour (one person in a hundred dies every hour). Within the first 24 hours, 33% of patients die from aortic dissection, 50% of patients within 48 hours and 75% within two weeks. Only early surgical intervention makes it possible to save a significant proportion of patients.
Treatment methods for aortic aneurysm
The main method of treating an aneurysm of any part of the aorta is surgical. The point of the method is to replace the dilated section of the aorta in order to prevent its further stretching and rupture. To replace the aorta, two methods are used - the endovascular (intravascular) method using a special intravascular prosthesis (stent graft), and open surgery - aortic replacement.
Each method has its own indications, and each of them has its own advantages and disadvantages.
The advantages of the surgical method lie in its versatility, that is, the ability to correct all disorders associated with an aortic aneurysm, regardless of the department and nature of the lesion. For example, in case of an aneurysm of the ascending aorta and damage to the aortic valve, aortic and aortic valve replacement is performed in combination with coronary bypass surgery.
To perform surgery on the ascending aorta and its arch, it is necessary to use artificial circulation, systemic hypothermia, and often complete circulatory arrest.
Indications for surgical treatment
- transverse size of the aneurysm,
- aneurysm growth rate;
- the formation of complications of this disease.
For each section of the aorta, there is a cutoff limit for the transverse size of the aorta, after which the risk of aortic rupture statistically significantly increases. Thus, for the ascending and abdominal aorta, the transverse diameter of the aneurysm is 5 cm dangerous in terms of rupture, for the thoracic aorta - 6 cm. If the diameter of the aneurysm increases by more than 6 mm in 6 months, then this is also an indication for surgery. Also threatening in terms of rupture and dissection of the aorta are the saccular form of the aneurysm and expansion of the aorta, which is smaller than the diameter that is the indication for surgery, but accompanied by pain at the site of expansion and dysfunction of the presenting organs. Dissections and completed ruptures of aneurysms are absolute indications for emergency surgery.
Endovascular interventions
They allow you to dramatically reduce the amount of surgical trauma, shorten hospitalization periods and reduce the inevitable suffering of the patient associated with surgical approaches. One of the main disadvantages of the method is the need for repeated interventions.
Types of endovascular operations for aortic aneurysm:
- implantation of a stent graft into the abdominal aorta,
- implantation of a stent graft into the ascending (thoracic) aorta.
The most modern method of treating aortic aneurysm is a hybrid method, which allows achieving optimal treatment results with the least surgical trauma.
Hybrid surgeries combine the advantages of open and endovascular interventions.
To prevent the development of aortic aneurysms, the most important thing is the need to control risk factors, namely arterial hypertension. In addition to arterial hypertension, the most significant risk factors are age (over 55 years), male gender, smoking, the presence of aneurysms in direct relatives, and high cholesterol levels.