Red blood cells are one of the very important elements of blood. Filling organs with oxygen (O2) and removing carbon dioxide (CO2) from them is the main function of the formed elements of blood fluid.
Other properties of blood cells are also significant. Knowing what red blood cells are, how long they live, where they are destroyed and other data allows a person to monitor their health and correct it in time.
General definition of red blood cells
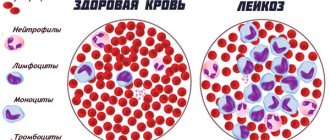
If you examine blood under a scanning electron microscope, you can see what shape and size the red blood cells have.
Human blood under a microscope
Healthy (undamaged) cells are small disks (7-8 microns), concave on both sides. They are also called red blood cells.
The number of red blood cells in the blood fluid exceeds the level of leukocytes and platelets. There are about 100 million of these cells in one drop of human blood.
A mature red blood cell is covered with a membrane. It has no nucleus and no organelles other than a cytoskeleton. The inside of the cell is filled with concentrated fluid (cytoplasm). It is saturated with the pigment hemoglobin.
The chemical composition of the cell, in addition to hemoglobin, includes:
- Water,
- Lipids,
- Squirrels,
- Carbohydrates,
- Salts,
- Enzymes.
Hemoglobin is a protein consisting of heme and globin . Heme contains iron atoms. Iron in hemoglobin, binding oxygen in the lungs, colors the blood light red. It turns dark when oxygen is released into the tissues.
Blood cells have a large surface area due to their shape. Increased cell flatness improves gas exchange.
The red blood cell is elastic. The very small size of the red blood cell and its flexibility allow it to easily pass through the smallest vessels - capillaries (2-3 microns).
How long do red blood cells live?
The lifespan of red blood cells is 120 days. During this time they perform all their functions. Then they are destroyed. The place of death is the liver, spleen.
Red blood cells degrade faster if their shape changes. When bulges appear in them, echinocytes are formed, and depressions - stomatocytes . Poikilocytosis (change in shape) leads to cell death. Pathology of the disc shape arises from damage to the cytoskeleton.
Video of blood functions. Red blood cells
Red blood cells
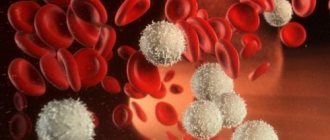
Red blood cells are anucleate blood cells that do not have organelles . It is an integral part of the blood along with leukocytes, platelets and plasma. The cells contain a protein called hemoglobin, which carries oxygen from the lungs to all parts of the body. Hemoglobin is the substance that makes our blood red.
In humans, like all mammals, mature red blood cells lack a nucleus. This gives the cell more space to store oxygen-binding hemoglobin, allowing red blood cells to transport more oxygen. Cells have a biconcave shape, which increases their surface area for oxygen diffusion. If a person has low hemoglobin levels, a condition called anemia, they may appear pale because hemoglobin colors the blood red.
Important! Every second, 2-3 million red blood cells are formed in the bone marrow and enter the bloodstream. Each cubic millimeter of blood contains 4-6 million blood cells.
The structure of red blood cells
These are small cells measuring 7-8 micrometers (µm). As a rule, they are shaped like a donut, without a hole in the middle. This is an important adaptation that allows the cell to efficiently transport oxygen molecules. It has also been shown that red blood cells are able to return to a biconcave disc shape after being exposed to external forces that cause them to deform.
Unlike other cells in the body, red blood cells are made up of known pigments and hemoglobin. It consists of four protein strands, each attached to one heme, which contains an iron atom and is capable of holding one oxygen molecule. Four hemes are attached to one protein to form a polypeptide chain. It is this special structure that allows the cell to carry oxygen and transport it to organs and muscles. Red blood cells do not have a nucleus and therefore do not reproduce by division.
Functions of red blood cells
Red blood cells perform the following functions:
- gas transportation. Transfer of oxygen from the alveoli of the lungs to tissues and carbon dioxide;
- participate in pH homeostasis (maintain normal acid-base balance);
- are regulators of vascular tone;
- protect the body from toxic substances and remove them from the body;
- participate in the implementation of humoral regulation of adaptation processes;
- support hemostasis function;
- participate in the movement of NH3 (ammonia, hydrogen nitride), purines and cholesterol from the liver to other organs and immune complexes.
Important! Although red blood cells are involved in the transport of oxygen, they do not use it during transportation for respiration. The absence of a nucleus reduces the overall weight of the cell, allowing them to move faster when they carry oxygen.
Where and how are they formed
Red blood cells begin their life journey in the red bone marrow of all human bones (up to the age of five).
In an adult, after 20 years of age, red blood cells are produced in:
- Spine,
- sternum,
- Ribs,
- Ilium.
Where are red blood cells formed?
Their formation takes place under the influence of erythropoietin, a kidney hormone.
With age, erythropoiesis, that is, the process of formation of red blood cells, decreases.
The formation of a blood cell begins with the proerythroblast. As a result of repeated division, mature cells are created.
From the unit forming the colony, the red blood cell goes through the following stages:
- Erythroblast.
- Pronormocyte.
- Normoblasts of different types.
- Reticulocyte.
- Normocyte.
The original cell has a nucleus, which first becomes smaller and then leaves the cell altogether. Its cytoplasm is gradually filled with hemoglobin.
If there are reticulocytes in the blood along with mature red blood cells, this is normal. Earlier types of red blood cells in the blood indicate pathology.
Place of formation of red blood cells
In the human embryo, the first place of blood formation is the yolk sac. Later, the liver becomes the most important organ in which red blood cells are formed. As the fetus develops, bone marrow develops, which is the only source of red blood cells in adult life.
Erythropoiesis is the process by which new blood cells are produced and takes about seven days. In a healthy adult, red blood cells are produced continuously in the red bone marrow of large bones at a rate of about 2 million cells per second. The main sites for the formation of red blood cells are the bone marrow spaces of the vertebrae, ribs, sternum and pelvis.
Erythropoiesis can be stimulated by the hormone erythropoietin, which is synthesized by the kidneys in response to hypoxia (systemic oxygen deficiency). During the final stages of development, immature red blood cells absorb iron, vitamin B12, and folic acid—nutrients that are essential for proper hemoglobin (iron) synthesis and normal red blood cell development (B12 and folic acid). Immediately before and after leaving the bone marrow, the developing cells are known as reticulocytes. These are immature red blood cells that have lost their nuclei after initial differentiation. After 24 hours in the bloodstream, the reticulocytes mature into functional blood cells.
Functions of red blood cells
Red blood cells fulfill their main purpose in the body - they are carriers of respiratory gases - oxygen and carbon dioxide.
This process is carried out in a certain order:
- Nucleated discs, as part of the blood moving through the vessels, enter the lungs.
- In the lungs, the hemoglobin of red blood cells, in particular its iron atoms, absorbs oxygen, turning into oxyhemoglobin.
- Oxygenated blood, under the influence of the heart and arteries, penetrates through capillaries into all organs.
- Oxygen carried by iron is detached from oxyhemoglobin and enters cells experiencing oxygen starvation.
- Empty hemoglobin (deoxyhemoglobin) is filled with carbon dioxide and converted into carbohemoglobin.
- Hemoglobin combined with carbon dioxide carries CO2 to the lungs. In the vessels of the lungs, carbon dioxide is broken off and then removed to the outside.
In addition to gas exchange, formed elements also perform other functions:
- Absorb and transport antibodies, amino acids, enzymes,
- Human red blood cells
- Transport harmful substances (toxins), some medicines,
- A number of erythrocyte factors take part in stimulating and preventing blood clotting (hemocoagulation),
- They are primarily responsible for blood viscosity - it increases when the number of red blood cells increases and decreases when it decreases,
- Participate in maintaining the acid-base balance through the hemoglobin buffer system.
What is the norm of red blood cells in the urine and why are they elevated?
A healthy adult should have approximately one to three red blood cells per field of view (the sample under the microscope at the time of analysis) in their urine.
Increased levels of red blood cells in urine can be caused by stress, intense physical activity, alcohol abuse, overwork, and certain diseases. Diseases in which the content of red blood cells in the urine increases include:
- Thrombocytopenia. The number of platelets in the blood decreases, which causes the blood in the vessels to clot worse and, as a result, ends up in the urine.
- Hemophilia. Blood clotting decreases, causing it to leak into the urine.
- Intoxication of the body. The entry of poisons or toxins into the body during viral and bacterial infections can cause an increase in the permeability of the glomerular membrane for red blood cells, due to which they enter the urine.
- Acute and chronic glomerulonephritis. The filtering function of the kidneys is impaired, as a result of which red blood cells enter the urine.
- Kidney cancer. The tumor affects the walls of blood vessels and provokes minor bleeding, as a result of which blood enters the urine.
- Urolithiasis disease. The integrity of the mucous membrane of the bladder is compromised, resulting in bleeding and some of the blood entering the urine.
- Pyelonephritis. The inflammatory process increases the permeability of the blood vessels of the kidney, and red blood cells leak into the organ.
- Hydronephrosis. There are difficulties in the outflow of urine, which leads to distension of the bladder and microdamage to blood vessels.
Red blood cells and blood groups
Normally, every red blood cell in the bloodstream is a cell that is free to move. With an increase in blood acidity pH and other negative factors, red blood cells stick together. Their bonding is called agglutination.
This reaction is possible and very dangerous when blood is transfused from one person to another. In order to prevent red blood cells from sticking together in this case, you need to know the blood group of the patient and his donor.
The agglutination reaction served as the basis for dividing human blood into four groups. They differ from each other in the combination of agglutinogens and agglutinins.
The following table will introduce the characteristics of each blood group:
| Blood type | Availability |
| agglutinogens | agglutinins in plasma | |
| I | 0 | αβ |
| II | A | β |
| III | B | α |
| IV | AB | 0 |
What should be the level of red blood cells in the blood of men, women and children?
For adult men, the norm is considered to be from 3.9•1012 to 5.5•1012 cells in 1 liter of blood, for women - from 3.9•1012 to 4.7•1012 cells in 1 liter of blood. In older people, the number of red blood cells gradually decreases, so their healthy indicator is slightly lower - approximately 4.0 x 1012 cells per liter.
For children, the norm of red blood cells in the blood varies depending on age:
- in umbilical cord blood - from 3.9•1012 to 5.5•1012 cells per 1 liter;
- on the first to third days of life - from 4.0•1012 to 6.6•1012 cells per liter;
- by the seventh day of life - from 3.9•1012 to 6.3•1012 cells per liter;
- at the age of two weeks - from 3.6•1012 to 6.2•1012 cells in 1 liter;
- at the age of one month - from 3.0•1012 to 5.4•1012 cells in 1 liter;
- at the age of two months - from 2.7•1012 to 4.9•1012 cells per liter;
- at six months - from 3.1•1012 to 4.5•1012 cells per liter;
- up to 12 years, regardless of gender - from 3.5•1012 to 5.0•1012 cells in 1 liter.
As they grow older, red blood cell standards begin to differ for girls and boys. Thus, for girls aged 13 to 19 years, a healthy indicator is considered to be from 3.5•1012 to 5.0•1012 cells per liter. While for boys aged 13-16 years the norm is from 4.1•1012 to 5.5•1012 cells per liter, and at the age of 16-19 years - from 3.9•1012 to 5.6•1012 cells in 1 liter.
Vital interest. Six naive questions about tests Read more
Transfusion
When determining your blood group, you should never make a mistake. Knowing the blood group is especially important when transfusing it. Not every one is suitable for a certain person.
Extremely important! Before blood transfusion, it is necessary to determine its compatibility. You cannot give incompatible blood to a person. This is life-threatening.
When incompatible blood is administered, red blood cell agglutination occurs . This occurs with this combination of agglutinogens and agglutinins: Aα, Bβ. In this case, the patient develops signs of transfusion shock.
They can be like this:
- Headache,
- Anxiety,
- Flushed face
- Low blood pressure,
- Rapid pulse,
- Tightness in the chest.
Agglutination ends with hemolysis, that is, red blood cells are destroyed in the body.
A small amount of blood or red blood cells can be transfused as follows:
- Group I – into the blood II, III, IV,
- Group II - to IV,
- Group III – to IV.
Important! If there is a need for transfusion of a large amount of fluid, only blood of the same group is infused.
What does increased and decreased levels of red blood cells in the blood mean?
An increased amount of red blood cells is called erythrocytosis. Excess red blood cells make the blood thicker and impair its properties. The level of red blood cells in the blood may be elevated due to dehydration, or less commonly due to a tumor of the kidneys or endocrine glands.
Possible symptoms of high levels of red blood cells in the blood include frequent headaches, dizziness, nosebleeds, and sometimes redness on the face or body. Erythrocytosis can be a sign of serious illness. Among them are erythremia (a disease of the hematopoietic system), diseases of the cardiovascular or pulmonary system, which can lead to respiratory and heart failure, renal artery stenosis and others.
A low level of red blood cells in the blood is erythropenia. The reason for the low red blood cell count may be:
- acute blood loss (for example, due to injury);
- chronic blood loss (for example, heavy menstruation in women or hidden bleeding due to gastrointestinal diseases);
- insufficient amount of iron in the body (necessary for hemoglobin synthesis);
- poor absorption of vitamin B12 and folic acid from food or their deficiency in the body;
- excessive fluid intake or intravenous administration of large amounts of saline;
- rapid destruction of red blood cells due to transfusion errors, hereditary diseases (such as sickle cell disease), poisoning from heavy metals or other poisons, and in people with an artificial heart valve.
Erythropenia usually manifests itself in a feeling of weakness, fatigue, tinnitus, and pale skin.
What are eosinophils in the blood and why are they needed? More details