Systematic abuse of alcoholic beverages can lead to the appearance of symptoms of such a dangerous disease as alcoholic cardiomyopathy. This is an extremely common pathology caused by the negative effects of ethanol alcohol on the myocardial tissue of the heart. In the EU, every third diagnosis of cardiomyopathy is due to the alcoholic variety. In 35% of cases, extremely negative consequences of this disease are recorded. This outcome can be avoided if you take charge of your own health in a timely manner, visit a qualified cardiologist, undergo diagnostics using modern equipment and begin treatment.
What is alcoholic cardiomyopathy?
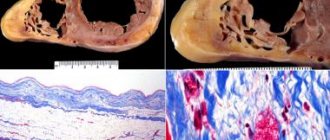
It is alcohol and its toxic effects that cause pathological changes in myocardial tissue. In turn, because of this, the functions of the heart muscle, blood circulation, and the supply of oxygen and nutrients to the body are disrupted. The mortality rate for alcoholic cardiomyopathy in various European countries ranges from 20 to 35%. In other words, every fifth patient with this diagnosis does not live to old age.
There are 3 known clinical forms of the disease:
- classic , the main symptom of which is heart failure with traditional symptoms;
- pseudo-ischemic is characterized by severe and prolonged chest pain after drinking alcohol, changes in the ECG, as in the diagnosis of coronary artery disease;
- arrhythmic is accompanied, accordingly, by various types of arrhythmia and symptoms: a feeling of lack of air, weakness, excessive sweating.
How is the diagnosis made?
When making a diagnosis, complaints, clinical manifestations, medical and life history, results of laboratory tests and instrumental research methods (ECG, WG, echocardiogram) are taken into account.
When a patient hides the fact of alcohol abuse, this process takes some time, since many symptoms are not specific. For such cases, doctors use daily monitoring of the cardiogram and a stress test. If necessary, the doctor prescribes sounding.
Diagnostic criteria are atrial fibrillation and enlarged heart muscle.
Causes of alcoholic cardiomyopathy
It is known that in general, cardiomyopathy is a heart disease with unclear causes. It is classified as primary (with changes at the genetic level) and secondary (provoked by other factors, diseases). Secondary cardiomyopathy often manifests itself in the alcoholic form. In some cases, it is accompanied by initial signs of liver cirrhosis. Alcohol impairs intestinal absorption, and metabolism is disrupted: the heart does not have enough vitamin B, calcium, etc. to function normally.
The cause of the pathology in this case is the same - excessive consumption of ethanol (more than 8 liters per year), which forms the basis of alcoholic beverages, for 4-5 years. Uncontrolled addiction to it in large doses can have a rapid negative effect. Abstinence causes improvement, which is leveled out when taking the next dose of alcohol.
Information about the disease
As mentioned earlier, cardiomyopathy is a fairly common disease and can be caused for various reasons, including due to congenital pathologies. But approximately 30% of diseases occur in people who abuse alcohol. This category of patients is most vulnerable to cardiovascular pathologies. Moreover, most often they are found in men.
In addition to alcohol dependence, regular stress, as well as smoking, can aggravate cardiomyopathy. Therefore, people with such characteristics are at risk and require systematic medical examination and timely preventive measures.
Alcoholic cardiomyopathy: symptoms
Often, patients who abuse alcohol refuse to recognize the symptoms of heart failure that appear the day after drinking too much as dangerous. Moreover, all symptoms are attributed to a hangover.
In addition, there are a number of symptoms of alcoholic cardiomyopathy that are not paid attention to at all, for example, sleep disturbance, frequent headaches, swelling of the extremities. Meanwhile, this is evidence of unsatisfactory functioning of the heart, liver and kidneys.
Over time, alcoholic cardiomyopathy manifests itself with more obvious symptoms:
- hand trembling;
- causeless agitation;
- weight gain or weight loss;
- vessels on the nose become noticeable;
- facial skin takes on a reddish tint;
- the sclera turns yellow.
The patient first shows concern when there are obvious signs of arrhythmia, shortness of breath during exercise, or prolonged pain in the heart. He may complain of a feeling of coldness in the extremities or, conversely, a feeling of heat. At night, persistent headaches and suffocation may occur.
The age of patients at which symptoms of alcoholic cardiomyopathy may appear is quite diverse, however, the first signs may appear as early as 30 years of age, when a person pays little attention to the ailment. Women in general do not have this disease (although they develop it in a shorter period of time), and the main statistics are filled out by men from 30 to 55 years old.
Pathology can be detected at an early stage using modern hardware diagnostic methods. In particular, echocardiography (ultrasound of the heart) provides detailed information about changes in the myocardium and the need to start treatment and change lifestyle.
A little history
The first description of alcoholic poisoning of the heart muscle belongs to the scientist G. Steel (1893). Later, J. Mackenzie (1902) focused on the symptoms of the disease and their relationship with alcohol-containing drinks. He expressed the opinion that hidden decompensatory processes can be diagnosed by paroxysmal tachycardia. It is the cause of a rapid increase in heart size, swelling of the lips and neck veins, and gray-bluish complexion of the face.
N. Vaquez in 1921 continued to study this pathology and published the conclusion that subacute myocarditis of alcoholic etiology may not be immediately diagnosed, since it occurs in a delayed form.
As knowledge about the disease accumulates, cardiologists have formed the opinion that the diagnosis of “alcoholic cardiomyopathy” is not entirely correct. Its primary origin was argued to be unknown, non-coronary factors. Today, the critical importance of the toxic effects of alcohol allows us to correct the terminology. The correct term is myocardial dystrophy.
It is difficult to carry out an accurate analysis of the prevalence of alcohol-related cardiomyopathies, since the patient’s history does not always indicate the fact of alcohol abuse. However, it can be clearly said that in Europe, a third of dilated cardiomyopathies are of an alcoholic nature.
12-22% of diseases are accompanied by death. 35% of coronary deaths at autopsy reveal alcoholic degenerative processes in the heart muscle.
Among men, the most affected age group is 30-55 years. A feature of female alcoholic cardiomyopathies is the short period of their development.
Stages of alcoholic cardiomyopathy and their symptoms
In medicine, there are 3 main stages in the development of alcoholic cardiomyopathy. The first of them can last for a decade, during which you may periodically notice individual symptoms: irritability, headaches, shortness of breath. But, as we have already noted, many patients prefer not to attach importance to them. Meanwhile, at this stage, metabolic disorders develop in the body, and negative changes occur in the structure of myocardial tissue.
The second stage can be brought closer by systematic consumption of alcohol in large doses. In this case, stronger symptoms of alcoholic cardiomyopathy will appear within 4-5 years. At this stage, you will begin to notice symptoms such as swelling, blue fingertips, and the appearance of an unreasonable cough. Hypertrophic phenomena and arterial hypertension are already actively developing in the myocardium. During the examination, the doctor will find dull tones in the heart. This stage is also characterized by damage to the kidneys, liver, and other gastrointestinal organs (gastritis, ulcers). Ascites may develop with extremely negative consequences.
If you do not start changing your life at the second stage, then irreversible processes may begin in the myocardium - some of its tissues will gradually die off, being replaced by connective tissue. This is how cardiosclerosis develops, accompanied by obvious disturbances in heart rhythm, symptoms of heart failure (prolonged severe chest pain, shortness of breath, sweating, weakness, fatigue, etc.).
With advanced cardiomyopathy, patients appear emaciated and their skin takes on a yellow tint. The examination reveals an increase in the size of the heart and pathological changes in its structure. Without treatment, the prognosis in this case is extremely negative.
Physical examination of other organs and systems
When examining the respiratory organs, no significant changes are detected. However, it should be taken into account that many people who abuse alcohol are also “hard” smokers and they exhibit symptoms of chronic obstructive bronchitis (prolonged exhalation, scattered dry whistling and buzzing rales during auscultation of the lungs).
When palpating the abdomen, many patients experience pain in the right hypochondrium. Epigastric tenderness can be caused by erosive gastritis, as well as gastric or duodenal ulcers, which often affect people who abuse alcohol. Pain in the right hypochondrium is usually associated with liver enlargement due to alcohol damage (chronic hepatitis, cirrhosis of the liver) or heart failure (“congestive” liver). Percussion reveals an increase in the borders of the liver, its surface is usually smooth, the edge is rounded (with cirrhosis, the edge is sharp). In case of decompensated portal hypertension in patients with concomitant alcoholic cirrhosis of the liver or severe heart failure, examination of the abdomen reveals a shortening of the percussion sound in sloping areas due to ascites.
Severe heart failure and cardiomegaly are accompanied by the appearance of a gallop rhythm (protodiastolic with the appearance of a pathological III tone or presystolic with the appearance of an IV tone), as well as an accentuation of the II tone over the pulmonary artery. Physical examination of patients with alcoholic cardiomyopathy reveals symptoms that are extremely similar to dilated cardiomyopathy, which forces a careful differential diagnosis of these two diseases (see further section “Differential diagnosis”). In patients with alcoholic cardiomyopathy, an increase in diastolic and systolic blood pressure is often found, and in many patients it is predominantly diastolic with an increase in pulse pressure. Usually, a moderate degree of arterial hypertension is observed, however, after an alcoholic excess, a sharp increase in blood pressure is possible up to the development of a hypertensive crisis. After stopping alcohol abuse, the severity of arterial hypertension may decrease, but spontaneous normalization of blood pressure does not occur in chronic alcoholics.
Kidney damage may occur in chronic alcoholism and therefore in some patients with alcoholic cardiomyopathy. It is caused primarily by the direct nephrotoxic effect of alcohol and acetaldehyde, as well as immunological and hemodynamic mechanisms. There are acute and chronic alcoholic kidney damage. The most common acute kidney lesions are myoglobinurin nephrosis (caused by severe alcoholic myopathy), necrosis of the renal papillae, urinary acid blockade of the kidneys (alcohol excess can cause a sharp increase in the level of uric acid in the blood and its intensive deposition in the kidney tissue) and hepatorenal syndrome in decompensated alcoholic cirrhosis liver. The main clinical sign of acute alcoholic kidney damage is acute renal failure with pain in the lumbar region, the development of anuria and the appearance of azotemia. Acute kidney damage develops, as a rule, after severe alcoholic excess. Chronic kidney damage in alcoholism is most often represented by alcoholic pyelonephritis and chronic glomerulonephritis. In some patients, chronic pyelonephritis may be complicated by apostematous nephritis due to the spread of infection in the kidney and infected emboli through its vessels.
Diagnosis of alcoholic cardiomyopathy
In terms of its symptoms, alcoholic cardiomyopathy resembles angina pectoris, so a doctor with insufficient qualifications may make a mistake in diagnosis and prescribe ineffective treatment.
At the same time, a qualified specialist, based on the results of cardiac ultrasound and ECG, will make an accurate diagnosis and develop a competent treatment method for alcoholic cardiomyopathy. Modern ultrasound equipment determines the expansion of the cavities of the heart and thickening of the walls of the ventricles. And when performing an electrocardiogram, rhythm disturbances and atrial flutter are noticeable.
Alcoholic cardiomyopathy: treatment
Let us immediately note that the treatment will not have any effect if you do not give up alcohol. Even small doses will negate the treatment. If your own strength is not enough for this, you need to seek the help of a professional narcologist who will reduce the craving for alcohol.
To treat alcoholic cardiomyopathy, you will have to be patient - this is a fairly long process, lasting from several months to several years. At this time, the functions of the myocardium will gradually be restored, and regeneration will begin in its tissues, i.e. recovery.
Of great importance is the drug treatment of alcoholic cardiomyopathy. You need to take modern medications:
- adrenergic blockers that stop the growth of myocardial walls;
- glycosides that relieve symptoms of heart failure;
- antiarrhythmic drugs that stabilize the heart rhythm;
- diuretics to relieve swelling.
Separately, the doctor prescribes vitamins, potassium, and drugs to restore metabolism.
The specialist will develop a special protein and vitamin diet for you. At the same time, treatment of the liver, kidneys and other organs affected by the disease will be carried out. It is important to restore their overall functionality in order to prevent an extremely negative outcome.
Modern treatment of alcoholic cardiomyopathy at CBCP
If you notice unpleasant symptoms of alcoholic cardiomyopathy, you are welcome at the CBCP Center for Circulatory Pathology. Here, highly qualified cardiologists and the latest expert-class diagnostic equipment are at your service. We will develop individual treatment programs for alcoholic cardiomyopathy for you. And in case of surgery, we will offer an effective recovery method based on innovative technologies used in similar clinics in the USA, Europe and Israel. The sooner you contact us, the more chances doctors have to restore your health!