A certain set of symptoms that develops in women during menopause is called in medical practice dishormonal menopausal cardiomyopathy.
Myocardial fibers experience the negative influence of hormonal “storms” that occur in the female body after 45 years. In most cases, pathology is detected 3-4 years after menopause.
A woman may be bothered by very unpleasant sensations in the sternum area for quite a long time, but she, due to her busyness or for other reasons, does not pay attention to them. Meanwhile, negative changes in the heart muscle can lead to very serious complications.
Who develops the disease
ICMP develops in approximately 5-8% of people with coronary heart disease (CHD).
It affects people aged 45-55 years. It is noteworthy that 90% of all patients are men. Previously, it was believed that ischemic cardiomyopathy occurs only in those who have suffered a myocardial infarction. Numerous scientific studies and studies of the state of the myocardium using modern diagnostic methods have made it possible to refute this fact. It turned out that ICMP is also present in people suffering from coronary heart disease in the form of angina (pressing/squeezing/burning pain behind the sternum during physical activity), but who have never had a heart attack. Moreover, the vast majority of such patients turned out to be.
The third stage is “Outpatient rehabilitation II”. Profile "Cardiology and cardiac surgery (adults)"
Lost validity - Archive
RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2014
ICD-10: Hypertensive disease with predominant damage to the heart and kidneys (I13), Hypertensive disease with predominant damage to the kidneys (I12), Hypertensive heart disease (I11), Ventricular septal defect (Q21.0), Atrial septal defect (Q21.1) , Dilated cardiomyopathy (I42.0), Other hypertrophic cardiomyopathy (I42.2), Other restrictive cardiomyopathy (I42.5), Other congenital anomalies of large arteries (Q25.8), Other multiple valve diseases (I08.8), Other forms angina pectoris (I20.8), Cardiomyopathy due to exposure to drugs and other external factors (I42.7), Myocarditis in diseases classified elsewhere (I41*), Multiple valvular lesions, unspecified (I08.9), Presence of cardiac and vascular implants and transplants (Z95), Unstable angina (I20.0), Obstructive hypertrophic cardiomyopathy (I42.1), Acute myocardial infarction (I21), Patent ductus arteriosus (Q25.0), Primary pulmonary hypertension (I27.0), Pericarditis for diseases classified in other headings (I32*), Repeated myocardial infarction (I22), Rheumatic diseases of the aortic valve (I06), Rheumatic diseases of the mitral valve (I05), Rheumatic diseases of the tricuspid valve (I07), Combined damage to the mitral and aortic valves ( I08.0), Combined lesions of the aortic and tricuspid valves (I08.2), Combined lesions of the mitral and tricuspid valves (I08.1), Angina pectoris with documented spasm (I20.1), Endocardial fibroelastosis (I42.4), Endomyocardial ( eosinophilic) disease (I42.3), Essential hypertension (I10)
Section of medicine: Medical rehabilitation
Changes in the heart muscle
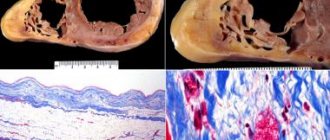
What happens in the heart during ischemic cardiopathy? The organ gradually increases in size due to the expansion of the left ventricle (LV), its walls become thinner, and the ability to pump blood decreases. Myocardial cells are damaged, and in place of dead cardiomyocytes (in the case of a heart attack), scar connective tissue appears, which creates conditions for the occurrence of arrhythmias. The result is chronic heart failure (CHF).
The pathophysiological mechanism for the development of ICMP is based on a process called hibernation - switching the work of the heart muscle to an energy-saving mode. Due to atherosclerotic narrowing of the coronary arteries, the myocardium receives insufficient oxygen. Under conditions of ischemia, the organ deliberately reduces the force of contractions to reduce the need for nutrition. This is a kind of protective mechanism - this is how the heart protects itself from a heart attack.
Causes
Sometimes dishormonal cardiomyopathy develops as a result of prolonged use of hormonal drugs.
The main cause of myocardial damage in dishormonal cardiomyopathy is a significant and prolonged disruption of hormonal levels. More often, such fluctuations in sex hormones occur during menopause or adolescence. However, in some cases, hormonal imbalance is provoked by other factors and diseases:
- long-term use of hormonal drugs for the treatment of hormone-dependent diseases of the kidneys and other organs, connective tissue diseases - in such cases, hormones are taken for years or for life, and their intake negatively affects the production of one’s own sex hormones;
- diseases of the ovaries and testicles - damage to these organs leads to a decrease in the level of sex hormones;
- diseases with excessive function of the thyroid gland and pathologies of the adrenal glands - disturbances in the production of these hormones lead to hormonal imbalance;
- obesity in men - with excessive accumulation of fat in the body, the level of estrogen increases, disrupting the functioning of the heart;
- prostate tumors – these tumors disrupt testosterone production and lead to hormonal imbalance.
When hormonal imbalances occur, the metabolism of fats, proteins and carbohydrates changes. As a result, the myocardium does not receive enough substances necessary for its normal functioning (fatty acids, glucose, microelements), becomes depleted and ceases to function properly.
Important symptoms
With the development of ICMP, patients with severe heart pain begin to notice a weakening of its intensity. Meanwhile, new signs appear:
- shortness of breath that gets worse over time;
- weakness after the usual amount of work;
- swelling of the ankles and lower legs;
- a feeling of heaviness or nagging pain in the right hypochondrium due to liver enlargement due to stagnation.
Often, people with ICMP experience heart rhythm disturbances, which are manifested by a feeling of rapid heartbeat, a feeling of “fading” of the heart. They can be constant or paroxysmal. During attacks, blood pressure may decrease, causing dizziness, darkening of the eyes, and sometimes short-term loss of consciousness. These symptoms are caused by decreased blood supply to the brain.
The most common cause of death in ischemic cardiomyopathy is progressive chronic heart failure. Less commonly, stroke and heart rhythm disturbances lead to death.
Propositions
In the context of the system:
- This is the case with the syllables.
- Alternately.
- Gyogov, avtomov, yazko âîé çîá.
- Geology and information sources.
- In other words, this is the case.
- Aliyah's version.
Basic information (90% synonymous) in the Russian Federation è è ñîïóòñòóþùèé åé àòårîñêårîç. More information about the world as a whole This is the same as the traditional one and the traditional one this is how it works. As for the world, this is what we are talking about ulsova. About the Russian Federation - the Russian Federation, the Russian Federation èððîöåñññ fôèáðîçà. Key words in the world and in the other world óäî÷ka.
How to confirm the diagnosis
- biochemical blood test is a mandatory test. Almost all people with ICMP have high levels of cholesterol in their blood. It is also necessary to determine glucose concentration to detect diabetes mellitus;
- electrocardiography (ECG) – a specific sign is a decrease in the ST segment below the isoline, indicating the presence of myocardial ischemia. However, I often fail to capture this change on a regular ECG, so I record a film of the person during physical activity (riding an exercise bike, walking or running on a treadmill). This increases the myocardium’s need for oxygen, which is reflected in the cardiogram. Also, during registration of a stress cardiogram, arrhythmias may appear (tachycardia, atrial fibrillation, atrioventricular or intraventricular block, etc.);
- echocardiography - ultrasound of the heart clearly shows the degree of expansion of the LV cavity, “non-functioning” areas of the myocardium (a sign of a previous heart attack). Particular attention is paid to the contractile function of the heart, i.e. ability to pump blood. For this purpose, an indicator such as the LV ejection fraction is assessed. In patients with ICMP it is below 55%. Another specific sign is the absence of thickening of the LV wall at systole;
- Coronary angiography allows you to assess the patency of the vessels supplying the myocardium (coronary arteries). It is thanks to this test that it is possible to accurately confirm that the development of ICMP is caused by cardiac ischemia. The main criterion is a narrowing of the lumen of one of the arteries by more than 50%.
Diagnosis of ischemic cardiomyopathy
Dilated cardiomyopathy in children
Primary diagnosis begins at an appointment with a cardiologist. The doctor collects a family history and analyzes the patient's symptoms. After this, he listens to the heart, performs tapping and a physical examination, which helps differentiate ICMP from other pathologies. To confirm the diagnosis you must undergo:
- General blood and urine tests to assess the condition of the body.
- Biochemical analysis of blood to assess the content of cholesterol, triglycerides and other compounds, the volume of which is increased in pathology.
- ECG. This study often reveals changes in the myocardium of a cicatricial nature, which happens after heart attacks, as well as a horizontal displacement downward from the ST line (a sign of ischemia). A characteristic indicator is myocardial hypertrophy, arrhythmia and conduction disturbances.
- Daily ECG monitoring. Helps identify low-symptomatic myocardial ischemia.
- Echocardiography detects myocardial hypertrophy, dilatation of the cardiac muscle cavity, hypokinesia of the left ventricular wall of a diffuse nature, as well as other signs of pathology.
- Chest X-ray. Allows you to determine the size of the heart, the chambers of which are enlarged due to ICMP, as well as to detect concomitant pathologies.
- Radioisotope scintigraphy, which is rarely performed. The study shows the localization of disturbances in the accumulation of thallium-201, and this is an indicator of ischemia and fibrosis.
- Coronary angiography, which reveals atherosclerotic lesions of the coronary arteries. It is noteworthy that the artery can narrow up to 50%.
In rare cases, the patient may be prescribed other tests. If there is an MRI machine in his locality, then ICMP can be diagnosed using it, since the study visualizes the heart muscle. If previous studies have not yielded results, the patient may undergo a biopsy, that is, part of the muscle will be taken for laboratory analysis.
A specialist will talk about an echocardiogram as an effective method for diagnosing ischemic cardiomyopathy in the following video:
Differences between ICMP and DCM
The clinical picture of ischemic cardiomyopathy is very similar to dilated cardiomyopathy. To provide a clearer picture of the differences between these diseases, I will provide information below.
Table: distinguishing features of ICMP from DCM
| Sign | ICMP | DCM |
| Patient age | On average 45-55 years | 30-40 years, can also develop in children |
| The main reason | Cardiac ischemia | Genetic mutations; Previous viral myocarditis; Alcoholism |
| Risk factors | Elderly age; Smoking; Diabetes; Obesity | Presence of DCM in close relatives |
| Development mechanism | Adaptation of the myocardium to ischemic conditions | Pathological expansion of the chambers of the heart |
| Dilation of the heart chambers | Only the LV undergoes significant expansion | Very pronounced dilation of all chambers of the heart |
| Severity of the clinical picture | Slow development of CHF symptoms | Rapid development of CHF symptoms |
| Arrhythmia frequency | 30% | Almost 100% |
| Thrombosis rate | 20-40% | 60-70% |
| Reversibility of changes | Partially reversible | Irreversible |
Drug treatment
For the treatment of ischemic cardiomyopathy I use:
- beta blockers - Atenolol, Bisoprolol;
- ACE inhibitors – Perindopril, Ramipril;
- sartans - Candesartan, Telmisartan (for intolerance to ACE inhibitors);
- aldosterone antagonists – Spironolactone;
- diuretics – Indapamide, Torasemide (for severe congestion);
- nitrates - Isosorbide Dinitrate (only in the presence of attacks of pain).
Doctor's advice: what medications should you take regularly and why?
In addition to the above medications, the patient in any case constantly needs to take the following medications:
- antiplatelet agents (acetylsalicylic acid) – prevent thrombosis, thereby reducing the risk of myocardial infarction;
- statins (Atorvastatin, Rosuvastatin) – drugs that lower blood cholesterol levels;
- anticoagulants (Warfarin, Dabigatran) - blood thinning drugs, they are necessary for the prevention of stroke in patients who have developed atrial fibrillation;
- hypoglycemic agents (Metformin, Glibenclamide) - if a biochemical blood test reveals a high level of glucose in the blood, I refer the patient to an endocrinologist to confirm diabetes mellitus, prescribe medications and a special diet;
Preventive measures
It is better to prevent a disease than to treat it. Therefore, once a year, if one of the above causes of the disease is present, it is necessary to undergo examination by a cardiologist. This will make it possible to identify a genetic predisposition to heart disease and begin treatment in a timely manner. In the early stages, treatment is more effective and has a favorable outcome for the person. An important role in the prevention of cardiomyopathy is played by a healthy lifestyle, systematic treatment of chronic diseases, and getting rid of excess weight, if any.
- Severe ischemic cardiomyopathy: there is not much chance of survival without help
Do they do surgery?
Revascularization surgeries, i.e. restoration of blood supply to the myocardium is the most effective way to treat ICMP. Thanks to them, it is possible not only to prevent the progression of the disease, but also to improve the contractile function of the left ventricle.
There are 2 main methods of surgical intervention for ICMP:
- stenting - installation of a metal cylinder (stent) at the site of stenosis, which expands the lumen of the artery;
- aorto-coronary bypass surgery - the creation of an artificial connection (ostium) between the aorta and the coronary artery, due to which blood flows bypassing the narrowed areas of the vessels.
Prognosis for cardiomyopathies
With regard to cardiomyopathy, the prognosis is unfavorable: the steady progression of heart failure causes a high probability of arrhythmic, thromboembolic complications, as well as sudden death of the patient. According to statistics, with dilated cardiomyopathy, the 5-year survival rate is 30%. Systematic treatment can stabilize the patient’s condition indefinitely. There are also cases of exceeding 10-year survival after heart transplantation. Surgical treatment, for example, for hypertrophic cardiomyopathy, gives a positive result, but is associated with a high risk of death of the patient during or after surgery. Women who have been diagnosed with cardiomyopathy are not recommended to become pregnant, since pregnancy and childbirth are associated with a high probability of maternal death.