Central venous pressure (abbreviated as CVP) is an integral level that characterizes indicators in the right atrium and, partially, in the pulmonary circulation at the moment of greatest relaxation of the muscular organ. That is, diastole. It is measured in mm, but not in the column of mercury, but in the water column.
An assessment of this level is not always necessary. There are several indications. All of them, one way or another, relate to urgent, critical conditions. For example, acute heart failure, cardiogenic shock and others.
In this case, the task of diagnosis is not only to determine the severity of the disorder, but also to evaluate the effectiveness of the infusion of drugs (infusion therapy).
CVP is a kind of marker, an indicator of myocardial contractility, pumping function, and hemodynamic quality. Any deviations indicate dangerous violations. In such a situation, the condition that caused the jumps in numbers is corrected.
Norms for adult patients
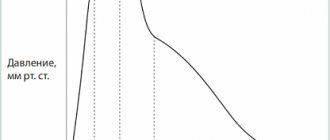
As for adequate indicators, they vary widely. According to studies, the normal central venous pressure in adults is from 30 to 90-100 mm water column.
Changes in value in one direction or another indicate critical disorders in the functioning of the cardiovascular system.
Measurements are carried out using invasive methods, by catheterization of large veins, therefore they do not resort to diagnosis without sufficient grounds.
The study has undeniable advantages: clarity of the indicator, monitoring of dynamic changes in real time, the ability to assess the quality of the treatment. But highly qualified personnel are required.
What does central venous pressure depend on?
Central venous pressure is determined by several factors:
- The volume of blood that is currently circulating in the body. If there is a lack of liquid connective tissue, after, for example, an injury, an open injury, a sharp drop in the level occurs, which indicates a decrease in the quality of the heart. The condition can result in the death of the patient if a transfusion is not performed.
Even after this, the level of central venous pressure rises and stabilizes gradually, not abruptly.
With an increase in the volume of circulating blood, against the background of pronounced edema, the pressure accordingly increases, which also does not bode well for the patient.
Such processes are also observed in a healthy person, but due to the body’s ability to self-regulate, no one notices this.
- Intensity of heart contractions. If the systole is full, the pumping function is normal, the liquid connective tissue is pumped sufficiently, the central venous pressure indicators are within adequate limits.
In critically ill patients, continuous measurement of the central venous pressure level allows one to notice the onset of a decline in myocardial contractility. That is, worsening heart failure.
Other methods do not provide such accurate results in real time.
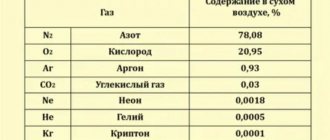
- Central venous pressure depends on respiration, but in this situation the values vary within normal limits. We are not talking about a static number, but about a range that is accepted in medical practice.
Some lung diseases, especially those accompanied by respiratory failure, are accompanied by abrupt changes in central venous pressure, including outside critical conditions.
These include, for example. COPD, bronchial asthma, emphysema, bronchiectasis and others. The influence of pathologies of the respiratory system on the measurement results must be taken into account.
- Situational short-term changes are possible when using diuretics. Especially loop or osmotic diuretics, vasodilating medications.
There are also physiological changes in the level of central venous pressure. In the morning, the numbers are minimal, close to the lower limit of an adequate indicator; in the evening they are much higher.
The reason is muscle movements, tension (for example, straining when coughing, physical activity).
In bedridden patients, the changes are not so noticeable, but they also exist, because vascular tone and pressure in the right atrium deviate for natural reasons.
Indications for monitoring
There are not many reasons for measuring central venous pressure. These are always life-threatening conditions. Among them.
- Formation of acute heart failure. Without adequate therapy, the deviation in almost 95% of cases ends in the death of the patient within a matter of hours or days. The response to the therapy is needed immediately; the high speed of data acquisition is precisely what ensures control of the central venous pressure. Another indication for assessing the level is also partially touched upon here.
- Study of the safety and effectiveness of intravenous drugs for heart failure. Dysfunction of cardiac structures requires careful infusion of pharmaceuticals, because there is a change in hemodynamics and fluid volume. It is not known how the muscular organ will react even to such a minor intervention. In case of severe insufficiency, measurement of central venous pressure is indicated as part of the therapy and to determine its safety and effectiveness.
- Assessment of the state of the cardiovascular system, pumping ability of the myocardium after surgical interventions. It is not always required, usually if there is a tendency to cardiac dysfunction, a diagnosis of heart failure has already been made, or after surgical treatment of blood vessels and abdominal structures. The task is to prevent collapse and death of the patient from spontaneous changes.
- Massive blood loss. In such a situation, even the transfusion itself carries enormous danger. Sharp jumps in central venous pressure can lead to the opposite effect: a decrease in myocardial contractility, critical heart failure, or even stoppage of organ function (asystole). Pressure control is used as a monitoring method.
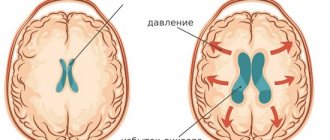
- Pericardial tamponade or suspicion of this condition. The essence is the accumulation of fluid or blood in a special membrane that encloses the heart itself. If the pressure in this bag exceeds the levels in the cardiac structures, the patient will stop and die. Careful monitoring can prevent such an outcome.
- Finally, it makes sense to carry out measurements during the acute phase of blood poisoning, sepsis. To avoid the development of a shock state or timely recognition of it.
Based on objective data, specialists adjust therapy and infusion volumes.
For what pathologies is monitoring prescribed?
Indications for CVP monitoring are serious disturbances of hemodynamic processes provoked by the following pathologies:
- acute circulatory failure;
- massive blood transfusion syndrome due to severe blood loss;
- chronic heart failure requiring invasive monitoring of the response during infusion therapy;
- the threat of developing shock conditions due to severe sepsis;
- suspicion of the development of cardiac tamponade;
- monitoring the condition during and after surgery in the abdominal area.
The CVP indicator helps to correctly assess the BCC (circulating blood volume) and the ability of the myocardium to contract.
And also control of its level allows you to avoid the occurrence of water intoxication due to the introduction of too large a volume of liquid during infusion activities.
Algorithm for measuring venous pressure
The study is carried out using an invasive method.
The list of actions is as follows:
- The doctor performs a puncture (puncture) of the jugular or superior vena cava using a special catheter with a tube leading to the system. This is a phlebotonometer or the so-called Waldmann apparatus. The device is relatively old, mechanical, but has great accuracy if installed correctly and all technological diagnostic features are observed.
- The catheter is passed to the right atrium and fixed in this state. Any movements are excluded to avoid dangerous consequences.
- A system for administering solutions and infusion therapy (dropper) is connected to the device. Then begin infusions of saline solution to fill the scale. The phlebotonometer itself is positioned so that the zero line, the beginning of the reference point, is at the level of the patient’s atrium. This will eliminate false indicators and errors.
- After filling the flotonometer scale with saline solution, you can disconnect the tube leading to the infusion therapy system. After a few minutes, the device begins to show measurement results.
Although the measurement technique is old, it is still widely used in medical practice. The mechanical phlebotonometer is being replaced by electronic analogues.
They are able to build graphs and display visual indicators on the screen. In addition, they do not require such qualifications from personnel and are easier to install.
Otherwise, the algorithm for measuring CVP is the same: insertion of the catheter, fixing it, checking the technique of performing the procedure, obtaining and processing the results.
Possible complications during measurement
Overhydration (infusion of an excessive amount of solution) of the body can provoke not only an increase in the level of central venous pressure, but also lead to organ damage, even death.
The following complications are most often observed with invasive methods for determining central venous pressure:
- pneumothorax;
- artery damage;
- infection.
And there are also cases with more rare, but quite serious consequences of the following plan:
- hydrothorax;
- air (or catheter) embolism;
- thrombosis;
- damage to nerve receptors;
- puncture by the end of the catheter of the superior vena cava or the right atrium with the subsequent appearance of hydromediastinum or hydropericarditis;
- perforation of the endotracheal tube cuff.
It is worth noting that if all the rules of technique for performing the method are observed, the possibility of complications occurring is minimized.
Reasons for the increase
Among the possible factors that provoke an increase in central venous pressure:
- Heart attack. Acute nutritional disorder of the heart muscle and myocardium. It is accompanied by a critical increase not only in central venous pressure, but also in blood pressure and general dysfunction of cardiac structures. Monitoring the indicator is not always necessary; the feasibility is determined by the doctor based on the current condition of the patient.
- Cardiogenic shock. Urgent, critical disorder. Mortality even with therapy is more than 90%. As is typical for pathology, it is extremely demanding on the quality of treatment and the professionalism of doctors; the slightest mistakes cost the patient his life. Measurement of central venous pressure in cardiogenic shock is always indicated.
- Pericarditis. An accumulation of fluid (hydropericardium) or blood (hemopericardium) in a special membrane, a sac, enclosing the heart. Develops as a result of trauma, medical diagnostic or therapeutic interventions. Spontaneous formation is also possible.
In any case, control of pressure in the right atrium and pulmonary circulation is a vital measure.
- Injuries of cardiac structures. Any, especially those accompanied by a violation of the anatomical integrity of certain tissues.
- Acute heart failure. For this disease, a dangerous sharp drop in myocardial contractility and the pumping function of the muscular organ is pathognomonic (typical).
As a result, insufficient trophism of all systems and tissues is formed. There is little nutrition, as well as oxygen, ischemic processes begin, including in the heart itself, which receives useful substances along with blood through the coronary arteries.
The venous indicator increases as a result of a reflex reaction, which the body is unable to correct.
Control of central pressure is also required in case of decompensation of chronic heart failure, when the disease becomes actualized and enters the acute phase.
- Inflammatory lesions of the heart. In particular myocarditis. It is usually of infectious origin. An autoimmune variant is possible; the body attacks the cells of the muscular layer of the heart itself, as a result of an erroneous reaction or failure.
The condition is unstable and reacts unpredictably to the administration of intravenous drugs, therefore constant monitoring of objective indicators of central venous pressure is necessary.
These are the key reasons. However, the list is incomplete; there are other factors for changes in venous pressure. For example, severe arrhythmia with instability of the contraction frequency, brain injuries that affect the regulation of the functioning of cardiac structures.
Provocation of the disorder is possible after the development of pulmonary embolism, pneumothorax, and injuries to the respiratory system. We are talking about exceeding the level, that is, from 90-100 mm aq. pillar or more.
Anything in this range is normal; dynamic changes are bound to happen throughout the day. They are not manifestations of pathology.
This must be taken into account during continuous measurements, including in bedridden patients.
Reasons for decreased central venous pressure
There are no fewer culprits for a drop in central venous pressure, but they relate to specific conditions.
Among the possible:
- Cardiogenic shock. Oddly enough, this change can provoke both an increase and a decrease in CVP levels. Because the process itself is unstable, sharp jumps occur. This is extremely dangerous.
- Dehydration. Heavy. By restoring the volume of fluid circulating in the body, a complete cure can be achieved. But control of central venous pressure is needed to prevent acute heart failure or to stop it in time, in the initial period.
- Central venous pressure drops with other forms of shock: traumatic, anaphylactic. However, this is a consequence. When the primary cause is corrected, it is possible to stabilize the levels and bring the body back to normal. The advisability of installing a catheter and measuring CVP in such situations is controversial and is decided at the discretion of specialists.
- There may be problems with the heart due to pulmonary embolism or acute respiratory failure. However, these are rather exceptions to the rule. Such pathological processes are mainly accompanied by jumps in central venous pressure with a parallel decrease in myocardial contractility.
Forecast
Since changes in CVP usually occur against the background of severe pathological conditions, the prognosis depends on the cause that provoked them:
- When the level of pressure in the veins decreases due to blood loss, the use of infusion therapy with blood replacement solutions leads to complete recovery.
- With CVP hypotension against the background of sepsis and septic shock, 50-75% of patients are cured.
- In case of CVP hypertension against the background of acute heart failure, the restoration of the patient’s health completely depends on the results of treatment of the underlying pathology.
Author of the article: Yulia Dmitrieva (Sych) - In 2014, she graduated with honors from Saratov State Medical University named after V. I. Razumovsky. Currently working as a cardiologist at the 8th City Clinical Hospital in the 1st clinic.
Visual assessment of the patient
An increase in venous pressure can be accurately detected only by measurement results. For this you need a device, a phlebotonometer.
However, changes can be suspected through simple observation, assessment of some visual factors and palpation of blood vessels.
The following points are characteristic of an increase in the level of central venous pressure:
- Swelling of the veins in the neck. At rest, they look large, are clearly visible, and can be palpated without problems. In this case, there is no reaction to changes in body position; the reason is stagnation of blood, impaired outflow.
- When performing a special test with pressure on the right hypochondrium, the pulsation intensifies and signs of swelling become more noticeable.
These methods are not informative enough, but they are good for rough estimates.
A decrease in central venous pressure is detected somewhat more difficult, using a ruler.
The patient is placed on the couch with his head and torso elevated. Approximately 45 degrees so that the body is higher than the legs. Pulsation of the jugular veins (in the neck) should be visible at a level of 3.5-4.5 cm above the collarbone. Its absence indicates a low indicator.
As for the diagnosis of the underlying pathology, it is carried out urgently or begins after correction of the disease, partial stabilization of the condition.
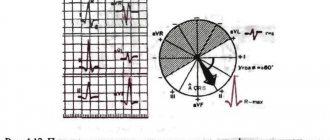
The list of measures depends on the specific disorder. At a minimum, this is an ECG, blood pressure measurement, ECHO-CG, if necessary, coronography, MRI, duplex scanning, etc.
Decoding the results
Causes of increased central venous pressure:
- Pulmonary embolism.
The most common reason forcing a doctor to measure CVP. The source of thromboembolism in most cases is the veins of the lower extremities.
If a blood clot breaks off, it travels through the inferior vena cava system first to the right side of the heart and then to the pulmonary artery. If a large trunk of the pulmonary artery becomes blocked, instant death occurs.
If small branches are affected, then the person feels shortness of breath and pain in the heart area (in this situation, a phlebotonometer is extremely necessary).
- Myocardial infarction (necrosis of the heart muscle).
- Cardiogenic shock (occurs when 40% of cardiomyocytes die).
- Pericarditis is a condition in which fluid accumulates in the pericardial cavity.
- Various arrhythmias (atrial fibrillation, paroxysmal tachycardia).
- Pneumothorax is the accumulation of air in the pleural cavity.
- Shock due to the release of exotoxins and endotoxins.
- Chronic obstructive pulmonary disease.
The reasons for the decrease in central venous pressure may be:
- heavy blood loss amounting to more than 20% of the total circulating blood volume;
- taking vasodilators;
- uncontrolled use of diuretics;
- profuse vomiting;
- diarrhea.
The physician should evaluate CVP values together with all clinical and laboratory data. A central venous pressure of less than 6 cm of water column is considered low, and a value of more than 12 cm of water column is considered increased.
Sometimes, to assess the dynamics of a patient’s condition, doctors need to monitor changes in central venous pressure. To do this, infusion therapy is carried out and changes in indicators on the phlebotonometer are monitored.
An increase of more than 5 cm of water column indicates poor contractility of the heart. An increase of less than 2 cm of water column indicates possible blood loss. In this case, infusion therapy must be continued.
To assess the patient's condition, the so-called express index is used. It more accurately reflects the patient's dynamics. The index is measured based on data from central venous pressure, blood pressure and heart rate.
In some cases, even a visual examination can determine the condition of a person’s venous system. It is considered normal if the veins in a person’s neck do not stand out in a vertical position.
If in the “standing” position pronounced pulsation and protrusion of veins are observed, this indicates an increased rate. Lying on the bed, the outline of the veins may stand out.
If the veins in this position are not visible at all, then this indicates low blood pressure.
In a reclining position, a distinct outline of the veins indicates increased pressure values. There is also a specific sign of high blood pressure - this is the pulsation of the jugular veins in response to palpation of the liver.
Treatment methods
Treatment depends on the specific condition. So, against the background of a decrease in the volume of circulating fluid or connective tissue, intravenous solutions are administered, and if necessary, blood transfusions are prescribed.
Cardiogenic shock and heart failure are corrected symptomatically. Then the disorder is corrected (after the patient has been removed from the emergency condition).
Pericardial tamponade requires puncture, drainage of the cavity, pumping out fluid, exudate or blood.
It is important to monitor CVP levels throughout the initial treatment, reducing or increasing the dose of the drug if necessary.
How is treatment and normalization carried out?
Treatment of a patient with an increase or decrease in pressure in the veins and right atrium depends directly on the factor that provoked this condition:
- In case of cardiovascular failure, restorative therapy of the contractility of the heart muscle is carried out.
- For hypovolemia, administration of blood substitutes or crystalloids is prescribed.
- Shock conditions - eliminate the cause of shock with subsequent restoration of organ function.
- Cardiac tamponade - a puncture is performed to remove excess fluid.
To normalize and prevent central venous pressure, venotonics are prescribed, which have the following effects:
- strengthen the walls of blood vessels, making them less permeable;
- have a positive effect on the tone of the veins, increasing their elasticity;
- actively counteract inflammatory processes.