Headache, dizziness, decreased visual acuity, nosebleeds, vomiting, sleep disturbances, short-term fainting - all this can be signs of high blood pressure in a child. The prevalence of arterial hypertension (AH) in children and adolescents is currently second only to asthma and obesity among chronic childhood diseases! A number of studies indicate that almost every 5 child in our country is susceptible to hypertension...
How to suspect high blood pressure (BP) in a child? In addition to those listed above, this is to learn how to correctly measure a child’s blood pressure. This is done a little more difficult than for an adult. Of course, the doctor will do this faster and more accurately, but you can also learn how to measure blood pressure at home.
HOW TO CORRECTLY MEASURE A CHILD'S BP?
1. First, understand what pressure will be normal for your child. To do this, you need to use three percentile tables (tables of percentages of different values):
- In Table 1, find your child’s age and height (for boys and girls, these are different parts of the table) and remember your child’s “height percentile” (from 5% to 95%).
- In Table 2 (for boys) or in Table 3 (for girls) look for the child’s age, correlate it with the “height percentile” and then find the value for the upper (systolic) and lower (diastolic) pressure. The optimal value will be up to 90%. Above is already above the norm.
2. In order to measure blood pressure, you need a tonometer, but most importantly, the correct - children's - cuff. For electronic tonometers there is only one children's cuff (diameter 15-22 cm). For mechanical ones, the diameter of the cuff for children starts from 7 cm. The size of the cuff corresponds to the circumference of the arm at the place where it is applied (measured with a measuring tape).
3. Measure blood pressure in your arms three times with an interval of 2-3 minutes, and calculate the average value. Compare with recommended.
4. Keep a blood pressure diary. If there was a one-time increase, it is recommended to measure 2-3 times during the day at rest while sitting, as well as in case of characteristic complaints (headaches, nosebleeds, dizziness).
Arterial hypotension in children and adolescents
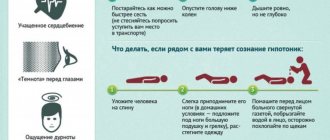
In this regard, expanding knowledge of the main etiopathogenetic mechanisms, features of the clinical course and treatment of arterial hypotension in childhood and adolescence is of particular relevance. Arterial hypotension is a symptom that reflects a decrease in blood pressure in the arterial system. Among the many classifications of hypotonic conditions for practical activities, including in pediatrics, the classification of N.S. is used. Molchanov (1962), where two variants of hypotension are distinguished. 1. Physiological hypotension, in which there are no subjective complaints, no symptoms of vegetative dystonia. This includes: – hypotension as an individual variant of the norm; – hypotension due to increased training (in athletes); – adaptive compensatory hypotension of residents of high mountains. 2. Pathological hypotension (primary and secondary). Primary arterial hypotension develops against the background of autonomic dystonia (VD) syndrome, in which there is a manifestation of clinical symptoms characteristic of increased parasympathetic tone of the ANS. Primary hypotension may have an unstable reverse course or occur in the form of a pronounced persistent form (hypotonic disease). With hypotension, there is a persistent decrease in blood pressure, accompanied by dizziness, headaches and orthostatic dysregulation. In pediatric practice, this diagnosis is not made, because the decrease in blood pressure in children and adolescents is reversible and its normalization is possible with age. Secondary (symptomatic) arterial hypotension is a consequence of organic pathology of the cardiovascular system (carditis, cardiomyopathy, heart rhythm disturbances); nervous system (tumors, hydrocephalus, post-comatose states, etc.); endocrine diseases (hypothyroidism, hypofunction of the adrenal cortex, polyneuropathy in diabetes mellitus); hematological pathology (anemia of various origins); chronic intoxication, as well as the result of the use of inadequate doses of medications (antihypertensives, certain antiarrhythmics, antidepressants, antihistamines). Obviously, arterial hypotension, which is one of the manifestations of autonomic dysfunction, is more appropriate to classify as secondary. Currently, primary arterial hypotension is considered as a multifactorial pathological condition, in the development of which endogenous and exogenous factors take part, in most cases acting in a complex manner. The main factors predisposing to the formation of primary arterial hypotension in children and adolescents are shown in Figure 1. The mechanisms of the development of arterial hypotension are complex and remain poorly understood. It is now considered proven that with hypotension there is a violation of the mechanism of autoregulation of central hemodynamics, expressed in the development of a discrepancy between cardiac output and total peripheral vascular resistance (TPVR) due to a decrease in the latter. At the same time, during the course of hypotension, OPSS continues to steadily decrease (Fig. 2). Various biologically active compounds with antihypertensive properties (nitric oxide, prostaglandins, taurine, natriuretic peptides, serotonin, kinins, etc.) are essential. In children and adolescents, the most significant mechanism for reducing peripheral vascular resistance is the autonomic one [1–4]. It is known that one of the most important functions of the ANS is vasomotor regulation. In the absence of autonomic imbalance, the interaction of the sympathetic (ST) and parasympathetic (PST) divisions of the ANS determine the adequacy of the autonomic influence on various functional systems of the body, and primarily on the activity of the heart and vascular tone. During VD, the interaction between the two sections of the ANS is changed, and both unidirectional ST–PST activity (compensation phase) and multidirectionality and uncoordination of their activity (decompensation phase) are possible. In the clinic, the unidirectionality of ST–PST activity is characterized by very moderate vegetative manifestations, accompanied by lability of vascular tone. Multidirectional ST–PST activity is characterized by maximum severity and manifestation of clinical symptoms, including vascular and muscular dyskinesias [5]. From the above it follows that arterial hypotension is characterized by miscoordination of the activity of two parts of the ANS with a pronounced predominance of PST (Fig.? 3). This is confirmed by the results of VNS spectrography [5], as well as changes in the content of neurotransmitters in the bloodstream, expressed in an increase in the level of acetylcholine and a decrease in the concentration of catecholamines [2,3]. Low activity of the sympathetic-adrenal system reduces the tone of precapillaries-arterioles, which is one of the leading hemodynamic factors in lowering blood pressure. In children and adolescents who have suffered a traumatic brain injury, with residual perinatal changes in the central nervous system, chronic psycho-emotional stress, a disruption of the neurogenic pathway of blood pressure regulation is often observed, as a result of a loss of balance between the processes of excitation and inhibition with the predominance of the latter in the cortex, in the stem structures, in the central vegetative centers with the formation of one of the forms of neurosis. In this case, hemodynamic disorders develop, one of the manifestations of which is endothelial dysfunction with a decrease in peripheral vascular resistance [1]. The mechanism of development of arterial hypotension in the presence of neurogenic and autonomic dysregulation is shown in Figure 4. Thus, the development of arterial hypotension in children and adolescents should be considered as a violation of a number of physiological regulatory mechanisms responsible for stabilizing systemic blood pressure. Clinical manifestations of arterial hypotension The main symptom of arterial hypotension is a decrease in blood pressure. The symptoms of hypotension are diverse, labile, transient, often transient in nature and generally reflect the manifestations of VD with a predominance of parasympathetic influences. Diagnostically significant clinical signs relate primarily to changes in the cardiovascular system, smooth muscle tone and neuropsychiatric disorders (Table 1). The criteria for the severity of arterial hypotension include [2]: • stable pattern of decrease in blood pressure; • intense cephalgia; • presence of vegetative crises; • orthostatic dysregulation (dizziness) and fainting; • degree of maladjustment (physical and psycho-emotional). Fainting is the most common symptom of severe arterial hypotension. Fainting (syncope) is a sudden short-term loss of consciousness with a sharp decrease in muscle tone due to a transient disorder of cerebral circulation. When faced with fainting, the pediatrician in each specific case needs to find out its causes, conducting a differential diagnosis between fainting that developed against the background of arterial hypotension of neurovegetative origin and somatic, neurological and other diseases, often manifesting with fainting states. Thus, fainting can be a symptom of a brain tumor, heart rhythm disturbances, anemia and other serious diseases. The main causes of fainting are given in Table 2. Clinical characteristics of fainting are given in Table 3. Autonomic crises (paroxysms, panic attack syndrome) with arterial hypotension are, as a rule, vagoinsular in nature. In this case, the following are observed: adynamia, profuse sweating, hypothermia, bradycardia, weak pulse, drop in blood pressure, even fainting, there may be abdominal pain with nausea, vomiting, headache, possible spasm of the larynx with difficulty breathing. It should be noted that complete classic autonomic crises in childhood and adolescence are rare and are observed in 12.7–22% of cases [5]. However, abortive, monosymptomatic crises occur quite often - in more than 50% of children with VD [5]. With hypotension against the background of PST, this may be a sudden short-term feeling of lack of air, interruptions or freezing of the heart, a feeling of a lump in the throat, etc. Having suddenly begun against the background of psycho-emotional stress, the crisis also ends suddenly. It is important for the attending physician to correctly assess these symptoms, since the presence of crises, even abortive ones, being one of the criteria for the severity of arterial hypotension, requires timely and adequate therapeutic correction of autonomic dysfunction, preventing their development. Diagnosis of arterial hypotension is based on correct determination of blood pressure levels. The strict rule is to measure blood pressure 3 times with an interval of 3–5 minutes. When diagnosing, unified criteria for arterial hypotension and the centile method are used, based on the distribution of blood pressure indicators taking into account the age, gender and height of the child. In practical work, uniform criteria can be used, but they are less accurate than the centile distribution of blood pressure (Table 4). With the centile method, arterial hypotension is considered to be blood pressure values below the 10th centile. A tendency to hypotension can be indicated when blood pressure values are below the 25th centile. Daily monitoring allows us to identify initial shifts in the circadian rhythm and blood pressure. When assessing the temporary index (the time of decrease in blood pressure during the day), it is important to know that an indicator value exceeding 25% indicates pathology: - with labile hypotension, the index fluctuates in the range of 25–50%; – with a stable form – above 50%. To confirm the neurovegetative genesis of arterial hypotension, it is necessary to conduct a comprehensive examination. The examination plan includes: 1. Analysis of clinical and anamnestic data. 2. Collection of genealogical history. 3. Assessing the level of physical activity (inactivity or excessive physical activity). 4. Analysis of the frequency and nature of traumatic situations. 5. Psychological testing (if indicated). 6. Clinical and biochemical (glucose, electrolytes, acute phase proteins, cholesterol and other lipid fractions) blood tests. 7. Electrocardiography (at rest and during physical activity). 8. Echocardiography (with assessment of intracardiac hemodynamics). 9. Electroencephalography (for visual assessment of changes in the bioelectrical activity of the brain). 10. Study of the functional state of the ANS (assessment of autonomic tone, CIG, clino-orthostatic test). 11. Consultations with specialists with an in-depth examination to exclude the symptomatic nature of hypotension - a cardiologist, psychoneurologist, ophthalmologist, endocrinologist (individually, according to indications). Treatment of arterial hypotension in children and adolescents Treatment should be started only after the cause of its decrease has been established. Obviously, with secondary hypotension, the object of therapeutic intervention is the underlying disease, in which a decrease in blood pressure is only its symptom. In case of arterial hypotension of neurovegetative origin (one of the most common types of hypotension in children and adolescents), it is necessary not only to take measures to normalize blood pressure, but also to correct autonomic imbalance. In this regard, the main directions of therapy are: 1. Leveling autonomic disorders by influencing both the higher autonomic centers and the activity of the peripheral parts of the ANS (parasypathetic and sympathicotonic). 2. Eliminating or minimizing the negative impacts of the environment and antisocial behavior of adolescents (smoking, drinking alcohol and drugs). Currently, non-drug and drug methods of treating arterial hypotension are generally accepted. For children and adolescents with labile arterial hypotension and moderate manifestations of vegetative dystonia, it is advisable to prescribe non-drug therapy. For long-term and persistent hypotension and severe autonomic imbalance, a combination of non-drug therapy with the prescription of medications is indicated. At the present stage, non-drug therapy is a systematic complex of therapeutic and recreational activities, including: • various forms of psychotherapy, individually selected depending on the specific background condition (autogenic training; rational psychotherapy; group; family; play, etc.). This allows you to change your attitude and increase tolerance to psycho-emotional traumatic factors - in other words, to correct the patient’s relationship with the environment; • normalization of the daily routine, providing for the need to alternate mental and physical activity, especially in adolescents; a full night's sleep lasting at least 8–10 hours with an elevated headboard, which stimulates the formation of pressor amines [2]. It is known that sleep is the main synchronizer of biorhythms in the body, in particular, the biorhythms of the functional activity of the cardiovascular system, parasympathetic and sympathetic sections of the ANS [8]; • balanced diet, in which the frequency of meals is at least 4–5 times a day without limiting salt; sufficient, but not excessive drinking regimen, because with hypotension the hydrolability of tissues is increased; • vitamin therapy, justified by the deficiency of the most important micronutrients in childhood and adolescence, regardless of the time of year and nature of nutrition, through regular intake of vitamin-mineral complexes. For vagotonia in adolescents, it is advisable to prescribe the drug Multi-Tabs Active, which contains, in addition to a balanced combination of 11 vitamins and 8 essential minerals, a plant adaptogen - ginseng root extract. For energy-metabolic correction when adapting to physical and psycho-emotional stress and overcoming stress, higher, but age-appropriate doses of minerals and vitamins are recommended. With vagotonia, the need for B vitamins increases significantly [6], which, when used in combination, have a metabolic, neurotrophic effect and a positive effect on vascular homeostasis; • therapeutic massage of the neck and collar area, calf muscles, hands. Massage is most effective for hypotension, accompanied by cephalgia, unpleasant sensations in the heart area, emotional lability, and decreased mental performance; • hydrotherapy (hydrotherapy), which has proven itself in pediatric practice in the form of dousing, rubbing, and cool showers. The action of these procedures is based on a tonic effect not only on the skin’s vascular system, vascular tone, but also on the immune system. Children should begin dousing and wiping in the summer with water at a temperature of 36–37? with a gradual decrease to room temperature (every 3–4 days by 1?). Daily, cool rain showers are effective; underwater shower - massage (jacuzzi). Prescribing medicinal baths at home with various herbal tonic additives (infusion of butterbur, birch, currant leaves; essential oils of orange, basil, rosemary, etc.) requires great caution, because non-compliance with recommendations on the temperature of the water (optimal t - 36.5 –37?) and the duration of the procedure (7–12 minutes) can lead to a paradoxical effect, up to the development of syncope. It is necessary to keep in mind the possibility of developing an allergic reaction to plant materials, because it is known that with parasymaticotonia there is a tendency to various allergic reactions. In the conditions of sanatorium-resort treatment, balneotherapy in the form of therapeutic baths with natural mineral water is widely used; • acupuncture, the principle of which is to normalize neurovegetative interactions, improve microcirculation and, accordingly, restore the supply of oxygen to tissues. In recent years, an effective method of acupuncture in the form of thermal pulsation with exposure of acupuncture points to infrared radiation has been developed and put into practice; • physiotherapy using procedures that have a stimulating effect, leading to normalization of vascular tone. Electrosleep with an individually selected pulse frequency is very effective. Electrophoresis according to Vermeule on the collar zone with solutions of caffeine, bromocaffeine, mesatone gives positive dynamics in dizziness, persistent cephalalgia, fainting and orthostatic dysregulation [4]; • aromatherapy (treatment with aromas), which has a clear effect on the cardiovascular system, neuropsychic sphere and has anti-inflammatory, antiviral and antimicrobial effects. Aromatic essential oils of rosemary, clary sage, orange, basil, anise, cloves, thyme, having a stimulating and tonic effect on the vascular wall, increase blood pressure and improve microcirculation. Correcting the activity of the nervous system, the indicated aromomalas reduce irritability, nervous tension, eliminate phobias, a sense of anxiety, lack of self -control, increase mental and physical activity [9]. Application: - massage - 3-5 drops of oil per 20-30 ml of massage cream or oil; - Aromo lamp - 1-3 drops per 30 ml of warm water. In the presence of allergic burden, the treatment begin with caution. Medicine therapy should be carried out in the absence of the effect of a set of non -drug measures, differentiated depending on the clinical manifestations and causal factors that caused vegetative dysregulation with the development of arterial hypotension in children and adolescents. The following groups of drugs are used: • plant adaptogens; • holinolytics; • nootropic drugs; • Cerebroprotectors; • antioxidants; • antidepressants and tranquilizers. In most cases, therapy of hypotension begins with adaptogens - funds that stimulate the central nervous system and the activity of the sympathetic department of the SLS. In the presence of inhibitance, apathy, reduced mental performance, increased drowsiness, accompanied by headaches, dizziness, fainting, children and adolescents are prescribed adaptogens of plant origin. Possessed by the adrenomimetical effects, these means contribute to the formation of adaptive reactions by regulating the equilibrium between the processes of excitation and inhibition in the cortex and subcortical vegetative centers, the activation of the functions of internal organs, and the increase in vascular and muscle tone. Such plant agents include: lemonnik, aralia, ginseng, leveze, pink radio (gold root), Eleutherococcus, Tatar, leaves and bark of hazel, hare cabbage. An ideal adaptogen for children is the root of the licorice. Adaptogens are prescribed once a day in the morning in the form of infusions, tinctures and decoctions. The duration of the course of treatment is 3 weeks. Adaptogens should be prescribed with caution in case of heart rhythm. For individual of them, there are age -related restrictions and contraindications: - for ginseng - increased bleeding (taking from 12 years); - for lemongrass - increased intracranial pressure, the presence of convulsive readiness; - For aralia - hyperkinesis, a restless superficial sleep. Of the drugs, the most used and effective in pediatric practice is Midodrin - A - ADrenomimetics [1]. Anticholinergic drugs with simultaneously adreno- and cholinolytic activity are prescribed for hypotension, accompanied by irritability, superficial night sleep, dysfunction of the sinus node of neurovegetative genesis. Nootropic drugs are shown to children and adolescents with a pronounced clinic of autonomic dystonia. At the same time, hypotension with its variety of symptoms is only an integral part of a whole complex of clinical manifestations of dystonia. This is observed in cases where a history of perinatal encephalopathy was a history and residual -organic changes in the central nervous system are noted. The use of nootropic preparations is pathogenetically substantiated, since they have a stimulating effect on the highest mental spheres that are not sufficiently formed in this contingent (attention, memory, speech, control of mental activity). In addition, these drugs have a positive effect on metabolic processes in the central nervous system and contribute to the maturation of brake and regulatory systems of the brain [10]. According to the chemical structure of nootropics, this is a heterogeneous group of drugs. In pediatric practice, piracetams, glycine, pyriditol, gameck -uergic drugs have proven themselves well. Gopanthenoic acid, unlike other GABA -GARGIC drugs, is a natural mediator of the GABA in the nervous tissue. Due to the features of the molecular structure, gopanthenoic acid penetrates through the hematoencephalic barrier and affects the functional activity of the central nervous system. The drug has the most soft psychostimulating effect in combination with moderate sedative [12]. The advantages of gopanthenic acid when compared with other nootropes include its neuroprotective and neurotrophic effects [10,12]. Cerebrovascular drugs are prescribed to improve brain hemodynamics and microcirculation in children and adolescents who have suffered a brain injury, as well as have perinatal pathology with the development of further vegetative dysregulation with bright and persistent clinical symptoms of hypotension. Among the indicated group of drugs for hypotension, course treatment with zinnarisine, vinpocetin is used. Of the drugs of multicomponent action, which includes an improvement in cerebral blood flow and a neurometabolic effect, Actovegin and vegetable products - ginkgo -bit, oxybral are used. Antioxidant therapy is used to reduce the intensification of lipid peroxidation, which resulted in stabilization of cell membranes, restoration of their permeability and, accordingly, an increase in energy supply of cells disturbed in the conditions of autonomic dysregulation. Literary data indicate the presence of a distinct relationship between vegetative disinfected and destabilization of cell membranes with the development of cells of cells and a violation of their functions, especially in conditions of chronic stress reaction [13,14]. Currently, there are a large number of different drugs with antioxidant effects. These include vegetable products, fat -soluble vitamins A, E; Amber acid in combination with citric, Kilikhinon, etc. Antidepressants, anxiolytics, large tranquilizers in pediatric practice are assigned strictly individually, while the neuropsychiatric man should be determined to be determined by the specifics of the symptoms and the need for differential diagnosis with neuro -psychic manuals. Teenagers with hypotension with insufficient activity, a sense of constant fatigue, sleep disturbance, apathy Pediatrician can recommend a natural antidepressant of plant origin - St. John's wort in various dosage forms [15]. Thus, only a consistent comprehensive, individual, epiopathogenetic approach to the treatment of arterial hypotension with its polyisystem symptoms will allow you to control its course, prevent its progression and contribute to the distinct improvement of the quality of life in childhood and adolescence.
Literature 1. Leontyeva I.V. Lectures on pediatric cardiology. – M., 2005. pp. 405–503. 2. Leontyeva I.V. Arterial hypotension in children and adolescents.// Lecture for doctors. – M., 2002, 62 p. 3. Gitun T.V. Diagnostic reference book for a cardiologist. – M.: AST, 2007, pp. 316–329. 4. Belozerov Yu.M. et al. Neurocirculatory dystonia.// In the book. Guide to pharmacotherapy in pediatrics and pediatric surgery. Clinical cardiology. – M., 2004. – P. 170–172. 5. Kushnir S.M., Antonova L.K. Autonomic dysfunction and autonomic dystonia – Tver., 2007, 215 p. 6. Belokon N.A., Kuberger M.B. Diseases of the heart and blood vessels in children: A guide for doctors in 2 volumes. – M.: Medicine, 1987. – T.1. – P. 303–337. 7. Korovina N.A. et al. Autonomic dystonia in children.// Guide for doctors. – M., 2006, 67 p. 8. Zaslavskaya R.M. Chronotherapy for patients with hypertension. //Medical Market.–1998. – No. 29. – P.18–21. 9. Potapenko V.P. Low pressure. Causes and effective treatment. – M.: AST; St. Petersburg: Sova, 2007.– 94 p. 10. Zavadenko N.N. Hyperactivity with attention deficit in children: diagnosis and treatment.//RMZh.– T.14.–№1, 2006, pp. 51–56. 11. Putilina M.V. Modern ideas about nootropic drugs.// Attending physician. – No. 5, 2006, pp. 10–14. 12. Sosina V.B. Possibilities and prospects for the use of Pantocalcin in clinical practice.//RMZh.–T.14.–No. 2, 2006, pp. 109–111. 13. Kurochkin A.A. et al. Neurocircular dystonia in children and adolescents (literature review and clinicians’ views on controversial issues of terminology, etiology, pathogenesis, clinical picture and treatment). // Russian Bulletin of Perinatology and Pediatrics. – 1999. – No. 6. – P. 21–25. 14. Neudakhin E.V. Autonomic changes in chronic stress response in children.// Abstracts of the All-Russian Congress “Pediatric Cardiology 2002”. – M., 2002. – P. 207. 15. Okorokov A.N., Bazenko N.P. Neurocircular dystonia. –M.: Med. lit., 2004, – 192 p.
WHEN does a child need to have their blood pressure measured?
In accordance with the order of the Ministry of Health of the Russian Federation dated July 3, 2000 No. 241, blood pressure should be measured at the age of 3 years (before entering a nursery school, kindergarten), 1 year before school (at 5-6 years), immediately before school (6 -7 years), after finishing 1st grade (7-8 years), at the ages of 10, 12, 14-15, 16 and 17 years.
- In children under 1 year of age, this pathology is most often associated with concomitant diseases - pathology of the kidneys, endocrine system, as well as congenital heart disease (coarctation of the aorta).
- From one to 6 years of age, pathologies of the kidneys and endocrine system are also the leading causes. Such children are observed by specialists and should be additionally examined by a cardiologist.
- From the age of 7, cases of so-called essential hypertension (primary, for unknown reasons) are detected.
- During puberty, this type of hypertension becomes the leading one.
Normal values
Optimal rates depend on the age of the child. For a one-year-old baby, the minimum value is 90/50 mmHg. In children from 2 to 9 years old, the norm is 100/60, in adolescents – 110/70, after 16 years – 120/70. Sometimes the values for each age are calculated using the formula 90+(age in years * 2) - systolic pressure; 60+age in years – diastolic pressure.
All these figures are quite arbitrary. If the indicators differ slightly from normal, but the child feels well, is alert and active, there is no reason for alarm. Hypotension is typical for residents of high mountain areas, athletes (during rest), it can be inherited. The decrease in indicators can be primary or secondary - due to some disease. The examination will determine the causes of hypotension.
WHAT TO DO IF A CHILD HAS HIGH BP?
If this was discovered during an examination by a doctor, then keep in mind that children have so-called “white coat” hypertension due to the child’s emotional lability. If this turns out to be not an isolated case, then you should definitely keep a diary where you can record the child’s blood pressure readings. Moreover, it is necessary to measure at the same time. It is also additionally necessary to conduct examinations to assess damage to other organs (the so-called target organs): clinical blood test, clinical urine test, biochemical blood test with assessment of the lipid spectrum, electrolytes, glucose and renal markers, ECG, echocardiography, fundus examination , Ultrasound of the kidneys with assessment of blood vessels, 24-hour blood pressure monitoring.
Based on the results of the examination, treatment is prescribed with recommendations for control and lifestyle. In short, if a child has high blood pressure, it is recommended that he:
- first of all, normalization of lifestyle,
- healthy 8-10 hour sleep, regular physical activity in the form of walking, running, swimming, skating, skiing, cycling 30-60 minutes a day, limiting weight lifting (static loads),
- limiting work on gadgets to 30-40 minutes a day,
- proper nutrition (limiting table salt, reducing light carbohydrates),
- normalization of weight in case of excess.
If a hypertensive crisis occurs with a worsening condition, call an ambulance; it is not recommended to take medications on your own if they have not previously been selected by a doctor; incorrect dosage selection can worsen the condition!
Primary hypotension
If no diseases are detected, and the pressure remains stably low, we can talk about primary hypotension. This is a functional disorder that the child “outgrows” over time.
In case of primary hypotension, observation by a neurologist and cardiologist is recommended. Often indicators are unstable during adolescence, but then normalize. Such basic measures as a well-thought-out regime of rest and exercise, proper nutrition, walks in the fresh air, and moderate exercise will help improve the quality of life. Pharmacological drugs are usually not prescribed; it is enough to change lifestyle for the child’s condition to improve.
WHAT IS THE DANGEROUS OF HIGH BLOOD PRESSURE IN A CHILD?
Every third child with this disease may develop hypertension in the future. High blood pressure affects both the general condition of the child - fatigue, retarded mental and physical development - and various organs, such as the eyes, kidneys, and heart.
But, I would like to emphasize that in children prevention and treatment are more effective than in adults and a complete cure is possible!
Pediatrician and pediatric cardiologist Ekaterina Aleksandrovna Yakunina.
Causes of secondary hypotension
Values may decrease as a result of slowing metabolism in some diseases. It is recommended to consult an endocrinologist. Hypotension often occurs after traumatic brain injury. A timely visit to a neurologist will help avoid complications.
Diseases of the cardiovascular system are another common cause. It is necessary to do a cardiogram, ultrasound of the heart, and consult a cardiologist. Hypotension often develops against the background of infectious diseases, intoxication, and allergic reactions. If the underlying disease is treated, the values return to normal.
Sometimes blood pressure may decrease due to chronic blood loss. In teenage girls, this can happen due to heavy periods, in which case you need to consult a pediatric gynecologist. If you have other symptoms indicating blood loss, it is worth getting tested to detect hidden bleeding. May require consultation with a gastroenterologist and other specialists.
Symptoms
If hypotension manifests itself in a newborn, then the parents do not have any special problems, because it is difficult to determine from his condition that there are health problems. This is explained by the fact that the child sleeps a lot, rarely cries, and is in constant peace. Children who have decreased muscle tone, legs and arms can extend more than 180 degrees at the joints. In addition, the following symptoms are observed: a delay in the rate of motor development and impaired swallowing and sucking. Dizziness, fainting, nosebleeds, emotional lability, decreased performance, joint and muscle pain, sudden deterioration in health, and headache may also occur. With a slight increase in blood pressure, the child’s health may be good. Although the child may quickly get tired and irritated. But if the pressure rises strongly, the child will always feel unwell. Among his complaints are the following: headache, dizziness, pain in the heart, palpitations, memory impairment. If a hypertensive crisis occurs. Symptoms such as severe headache, nausea, blurred vision, convulsions, impaired consciousness and others may be observed.
Classification of conditions accompanied by low blood pressure.
- Physiological hypotension is low blood pressure, which is a variant of the norm or is temporary.
- Hypotension as an individual variant of the norm, i.e., a feature of a given person that does not cause him discomfort.
- Hypotension due to increased training (in athletes).
- Hypotension is adaptive (in residents of highlands, tropics and subtropics).
- Pathological hypotension is a disease whose main manifestation is low blood pressure, a condition that requires diagnosis, mandatory treatment and observation.
- Neurocirculatory hypotension (primary, which is an independent disease, most often caused by impaired vascular tone and vascular function).
- Idiopathic orthostatic hypotension. An independent disease, the main symptom of which is a drop in pressure when changing body position.
- Symptomatic (secondary) hypotension:
- acute form (with shock, collapse, fainting, allergic reaction);
- chronic form;
- a form with severe orthostatic syndrome, that is, with severe dizziness when changing body position.
- Reduced blood pressure in diseases of the nervous system.