Synonyms: hydrocephalic syndrome, hypertensive-hydrocephalic syndrome, HGS. ICD-10 code: G91
Medical editor: Druzhinkina V.Yu., neurologist. November, 2020.
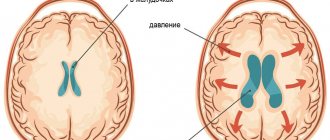
Hydrocephalic syndrome is a pathological condition characterized by excess production of cerebrospinal fluid (CSF), which accumulates under the meninges and in the ventricles of the brain.
The clinical picture of hypertensive-hydrocephalic syndrome can be explained by two concepts:
- hypertension (increased intracranial pressure);
- hydrocephalus (increased amount of cerebrospinal fluid in the brain).
Important! Hydrocephalic syndrome as a term is accepted only in the former USSR (in the CIS) and in modern Russia. Western doctors attribute hydrocephalic syndrome to a manifestation of brain pathologies.
The syndrome is often diagnosed by pediatric neurologists, and, as a rule, without reason. HHS is a fairly rare pathology, and in 97% of cases the diagnosis of hydrocephalic syndrome has no right to exist.
Causes
There are congenital causes of hydrocephalic syndrome (HHS in newborns) and acquired ones.
Congenital causes of hydrocephalic syndrome
- course of pregnancy and childbirth with complications;
- hypoxic (intrauterine hypoxia and intrauterine growth retardation, their manifestation in fetal bradycardia) and ischemic (injuries during childbirth) brain damage;
- premature birth (up to 36 weeks);
- head injuries during childbirth (subarachnoid hemorrhages);
- intrauterine infections (toxoplasmosis, influenza, cytomegalovirus infection and others);
- congenital abnormalities of brain development;
- delayed birth (at 42 weeks and later);
- long water-free period (more than 12 hours);
- chronic maternal diseases (diabetes mellitus, chronic pyelonephritis, arterial hypertension and others).
Acquired causes of hydrocephalic syndrome:
- tumors, abscesses, hematomas, parasitic cysts of the brain;
- foreign bodies in the cranial cavity;
- fractures of the skull bones with the introduction of fragments into the brain;
- causeless intracranial hypertension;
- infectious diseases (malaria, tick-borne encephalitis);
- post-stroke disorders;
- metabolic disorders.
Photo: cerebrospinal fluid pressure on the brain with hydrocephalus.
Symptoms of hydrocephalic syndrome
Signs of hydrocephalic syndrome in newborns
Parents note that the child does not latch on well, constantly cries for no apparent reason, and sometimes moans.
The child has:
- decreased muscle tone (“seal feet” and “heel feet”);
- weak innate reflexes (swallowing, grasping);
- tremor (trembling of the limbs, chin) and convulsions may occur;
- spitting up like a fountain;
- strabismus;
- when examined by a doctor, positive Graefe's sign is observed (the eyeball is directed downward - a white stripe is visible between the pupil and the upper eyelid) and the rising sun sign (the iris is almost half hidden behind the lower eyelid)
- opening of the sutures of the skull (in particular the sagittal);
- bulging, tension of the fontanelles;
- in dynamics there is an increased increase in head circumference (by 1 cm every month), which is significantly ahead of age standards;
- head thrown back, which is especially noticeable during sleep;
- cyanosis, pale skin;
- increased respiratory movements;
- When examining the fundus, swelling of the optic discs is observed.
Clinical manifestations of HGS in children
Symptoms of hypertensive-hydrocephalic syndrome in older children usually develop after an infection or brain injury.
A characteristic symptom is headache, which often occurs in the early morning hours, nausea and vomiting, which follow it and do not bring relief. The pain is dull, aching or bursting; localized in the area of the temples, forehead and brow ridges.
Children complain that it is difficult for them to raise their eyes and lower their heads. Dizziness often occurs (young children define it as “swinging on a swing” or “instability of objects”).
During an attack of pain, pale skin, weakness and lethargy are noted. Bright light and loud sound cause irritation and increase unpleasant sensations.
Walking “on tiptoes” due to increased tone of the leg muscles, squint, drowsiness and slow thinking, poor memory and attentiveness are also typical. Such children do not eat well because they feel nauseous.
Hydrocephalic syndrome in adults
HGS in adults develops as a result of traumatic brain injuries, tumors, neuroinfections and after a stroke.
Signs of hydrocephalic syndrome are similar to those in older children:
- visual impairment (double vision, strabismus);
- severe headaches;
- nausea and vomiting, especially severe in the morning;
- disturbance of consciousness up to coma and convulsions.
Therapeutic measures
It is important to remember that hydrocephalus syndrome in an infant can only be treated using methods approved by a doctor. Self-medication is strictly prohibited due to the possibility of causing harm to the child’s body.
Therapy is complex. Treatment measures are prescribed individually, taking into account the severity, characteristics of the clinical picture, and the patient’s age. The main method of therapy is medication.
For treatment purposes, the following groups of drugs are used:
- diuretics;
- sedatives;
- nootropic;
- antibiotics;
- venotonics;
- antitumor.
Numerous positive reviews characterize activities that allow a child to develop certain skills and abilities, develop his abilities, and adapt him to social life. A good effect is characterized by therapeutic massage and moderate physical activity. HGS can also be treated with numerous physiotherapeutic procedures.
Diagnostics
Diagnosis of hydrocephalic syndrome is difficult. Not all instrumental methods help establish a diagnosis in 100% of cases. In infants, regular measurement of head circumference, checking reflexes, dynamics of body weight gain, and neurological examinations are important.
Also in the definition of GGS is used:
- electroencephalography;
- lumbar puncture of the spinal cord to take cerebrospinal fluid to measure its pressure (the most reliable method);
- neurosonography (ultrasound examination of the anatomical structures of the brain, in particular the size of the ventricles);
- assessment of fundus vessels (swelling, congestion or vasospasm, hemorrhage);
- computed tomography () and nuclear magnetic resonance (NMR).
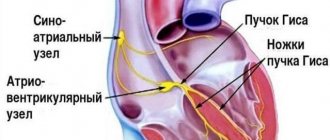
Anatomy of the central nervous system of newborns
The central nervous system is the main part of the nervous system, which includes the brain and spinal cord, located in the cranial cavity and the spinal canal. The central nervous system is responsible for controlling all vital processes in the body, thinking, speech, coordination, and the functioning of all senses.
The brain consists of the following sections:
- cerebral hemispheres (left and right)
- diencephalon
- midbrain
- bridge
- cerebellum
- medulla
Ultrasound examination of these sections allows us to assess the condition of the gray and white matter of the brain and exclude the presence of congenital pathology in the fetus (hemorrhages, tumors, malformations, cysts, hydrocephalus, dislocations, etc.), as well as possible changes associated with childbirth.
The liquor system consists of:
Internal liquor spaces
- Lateral ventricles of the brain (right and left)
- Third ventricle of the brain
- Fourth ventricle of the brain
External liquor spaces
- Subarachnoid space
- Interhemispheric fissure
In accordance with this, hydrocephalus can be external - when the size of the interhemispheric fissure increases; internal - with expansion of the lateral ventricles (VLD, VLS), third and fourth ventricles (V3, V4); and mixed.
Each ventricle contains a choroid plexus (Plexus chorioidei). These plexuses play an important role in the production of cerebrospinal fluid - a fluid that circulates in the ventricles of the brain, the subarachnoid space of the brain and spinal cord, and the cerebrospinal fluid ducts. Overproduction of cerebrospinal fluid leads to hydrocephalus and an increase in the size of the cerebrospinal fluid containing spaces.
Normal values for sizes V3, V4, MS, MD, VLS, VLD, m/p gap, bone/marrow diastasis, see below
Treatment of hydrocephalic syndrome
Treatment of hydrocephalic syndrome is carried out by neurologists and neurosurgeons with the involvement of ophthalmologists. Patients with HGS need to be observed and treated in a specialized neurological center.
Treatment in newborns
Children require outpatient or surgical treatment, depending on the cause. Main therapeutic measures:
- prescribing a diuretic drug - diacarb (reduces the production of cerebrospinal fluid and removes excess fluid from the body, primarily from the cranial cavity);
- it is possible to take nootropics - some experts claim that these drugs improve blood supply to the brain (Encephabol, Actovegin), but there are no convincing large-scale studies on this topic;
- for hyperexcitability, sedatives are indicated;
- massage.
Treatment for infants is quite long, taking several months.
Treatment of HGS in older children and adults
In adults and older children, therapy also depends on the cause of hydrocephalic syndrome. If it is the result of a neuroinfection, then appropriate antiviral or antibacterial therapy is carried out.
In case of traumatic brain injuries and tumors, surgical intervention is indicated. Diuretics and nootropics are also used.
Advantages of treatment at the Neonatus Sanus Osteopathy Clinic
Our clinic of osteopathy and neurology on Vasilyevsky Island “Neonatus Sanus” - health from birth, has extensive practical experience in the prevention and treatment of newborns, infants and infants.
We know how and love to work with young children!
Our clinic employs experienced osteopathic doctors and neurologists. A lot of attention is paid to each child in order to understand the child, accurately assess his condition, give recommendations to parents and, if necessary, carry out effective osteopathic treatment.
In our center you can get the best examination, treatment and recommendations from leading specialists in St. Petersburg.
Complications and prognosis
Complications of hypertensive-hydrocephalic syndrome are possible at any age:
- delayed mental and physical development;
- blindness;
- deafness;
- coma;
- paralysis;
- epilepsy;
- urinary and fecal incontinence;
- death.
The prognosis is most favorable for hydrocephalic syndrome in infants. This is because they experience transient increases in blood pressure and cerebrospinal fluid, which stabilize with age.
In older children and adults, the prognosis is relatively favorable and depends on the cause of HGS, the timeliness and adequacy of treatment.
Sources:
- Bitterlich L.R. On the issue of differential diagnosis, classification and differentiated treatment of hydrocephalus and hirdocephalic syndromes in children. - International Neurological Journal, No. 1 (79), 2021.
- Order on approval of the standard of specialized medical care for children with hydrocephalus. — Ministry of Health of the Russian Federation, 2013.
- Federal clinical guidelines for the provision of medical care to children with consequences of perinatal damage to the central nervous system with hydrocephalic and hypertension syndromes. — approved Union of Pediatricians of Russia February 14, 2015
News
Author: neurologist S.V. Zaitsev
This article is over 18 years old, all this time it has been actively multiplying and spreading across websites, social networks and blogs.
The main goal was achieved, many parents (and doctors) gained some clarity in perinatal neurology, many babies were “saved” from hospitalization, unnecessary examinations and pills. For many doctors and massage therapists, the “volume of work” has decreased significantly.
It seems that everything has been clear for a long time, unfortunately, the article has not lost its relevance at all, so I am writing again and again...
Despite free access to any scientific information, and so far more than 90%! Children in their first year of life come for consultation to specialized neurological centers about a non-existent diagnosis - perinatal encephalopathy (PEP). Child neurology is a relatively new field, but is already going through difficult times. At the moment, many doctors practicing in the field of infant neurology, as well as parents of infants with any changes in the nervous system and mental sphere, find themselves “between two fires.” On the one hand, the position of the school of “Soviet child neurology” is still strong - excessive diagnosis and incorrect assessment of functional and physiological changes in the nervous system of a child in the first year of life, combined with long-outdated recommendations for intensive treatment with a variety of medications. On the other hand, there is often an obvious underestimation of existing psychoneurological symptoms, inability to strategically plan, ignorance of the possibilities of modern neurocorrection (orthopedics, ophthalmology, neuropsychology, speech therapy, defectology, etc.), therapeutic nihilism and fear of the practical application of modern methods of neurorehabilitation and drug therapy; and, as a result, lost time, unused internal reserves and the development of neuropsychic disorders in preschool, school and adolescence. At the same time, unfortunately, a certain “formality-automaticity” and “cost-effectiveness” of modern medical technologies lead, at a minimum, to the development of psychological problems in the child and his family members. The concept of “norm” in neurology at the end of the 20th century was sharply narrowed, but is now intensively and, not always justifiably, expanding. The truth is somewhere in the middle...
According to perinatal neurologists of the country's leading medical centers, so far, no less 80-90%!
Children in their first year of life are referred by a pediatrician or neurologist from a district clinic for a consultation regarding
a non-existent
diagnosis - perinatal encephalopathy (PEP):
The diagnosis of “perinatal encephalopathy” (PEP or perinatal lesion of the central nervous system (PP CNS), in the old days was very common in pediatric neurology and extremely convenient: it described almost any, real or imaginary, dysfunction (and even structure) of the brain in the perinatal period of a child's life (from approximately 7 months of intrauterine development of the child until 1 month of life after birth), arising as a result of pathology of cerebral blood flow and oxygen deficiency.Later, bringing to life the “continuity of neurological diagnostics,” perinatal encephalopathy (PEP) necessarily smoothly transformed into two other favorite neurological diagnoses: MMD (minimal cerebral dysfunction) and VSD (vegetative-vascular dystonia).
The diagnosis of “perinatal encephalopathy” (PEP) was usually based on one or more sets of any signs (syndromes) of a probable nervous system disorder, for example, hypertensive-hydrocephalic syndrome (HHS), muscular dystonia syndrome (MDS), hyperexcitability syndrome.
After a thorough clinical examination, sometimes in combination with additional studies, the percentage of reliable diagnoses of perinatal brain damage (hypoxic, traumatic, toxic-metabolic, infectious, etc.) quickly decreases to 3-4% - this is more than 20 times! The most bleak thing about these figures is not only the certain reluctance of individual doctors to use the knowledge of modern neurology and conscientious delusion, but also the clearly visible psychological (and not only) comfort of such overdiagnosis.
Hypertension-hydrocephalic syndrome (HHS): increased intracranial pressure (ICP) and hydrocephalus
As before, the diagnosis of hypertension
“
hydrocephalic syndrome” (HHS)
or “intracranial hypertension” (increased intracranial pressure (
ICP)
), one of the most common and “favorite” medical terms among pediatric neurologists and pediatricians, which can explain almost everything! and at any age, complaints from parents. This is extremely comfortable for a doctor!
For example, a child often cries and shudders, sleeps poorly, spits up a lot, eats poorly and gains little weight, eyes widen, walks on tiptoes, his arms and chin tremble, there are convulsions and there is a lag in psycho-speech and motor development: “only he is to blame — hypertensive-hydrocephalic syndrome (HHS)
or increased intracranial pressure." Isn’t it a very useful and convenient diagnosis?
Quite often, as the main argument for parents, “heavy artillery” is used - data from instrumental research methods, completely outdated and uninformative echoencephalography ( ECHO-EG
) and rheoencephalography (
REG
), or examinations “from the wrong opera” (
EEG
), or incorrect, in isolation from clinical manifestations, subjective interpretation of normal variants during neurosonography or tomography.
In fact, intracranial hypertension is a very serious and quite rare neurological and neurosurgical pathology. It accompanies severe neuroinfections and brain injuries, hydrocephalus, cerebrovascular accidents, brain tumors, etc.
Hospitalization is mandatory and urgent!
In addition, there is no direct and reliable connection between intracranial hypertension and translucent vessels on the face and scalp, walking on tiptoes, trembling hands and chin, hyperexcitability, developmental disorders, poor academic performance, nosebleeds, tics, stuttering, bad behavior, etc. d. and so on.
That’s why, if your baby has been diagnosed with “perinatal encephalopathy (PEP) or perinatal damage to the central nervous system (PP CNS), intracranial hypertension or hypertensive-hydrocephalic syndrome (HHS)”, based on the “bulging” eyes (not to be confused with the true Graefe symptom , a symptom of the “setting sun”!) and walking on tiptoe, then you shouldn’t go crazy in advance. In fact, these reactions may be characteristic of easily excitable young children. They react very emotionally to everything that surrounds them and what happens. Sensitive parents will easily be able to notice such a relationship.
It is absolutely unreasonable to begin treatment for this unspecified “serious” pathology on the recommendations of one doctor based on the above “arguments”; in addition, such unfounded treatment may not be safe at all.
But! There is another, no less important aspect of the problem that must be taken into account in this situation. Sometimes medications are really necessary, and wrongful refusal of them, based only on mom’s (and more often dad’s) own conviction that medications are harmful, can lead to serious troubles.
Now a few words about the equally “adored” hydrocephalus
and
hydrocephalic syndrome
.
Unfortunately, in ordinary life such an erroneous “diagnosis” occurs in almost every fourth or fifth baby. It turns out that some doctors often incorrectly call a stable (usually slight) increase in the ventricles and other cerebrospinal fluid spaces of the brain hydrocephalus (hydrocephalic syndrome). This does not manifest itself in any way through external signs or complaints and does not require treatment. Sometimes, when performing neurosonography, an ultrasound doctor finds pseudocysts
- but this is not a reason to panic at all! Pseudocysts are single round tiny formations (cavities) containing cerebrospinal fluid and located in typical areas of the brain. The reasons for their appearance, as a rule, are not reliably known; they usually disappear by 8-12 months. life. It is important to know that the existence of such cysts in most children is not a risk factor for further neuropsychic development and does not require treatment. However, although quite rare, cysts form at the site of subependymal hemorrhages, or are associated with perinatal cerebral ischemia or intrauterine infection. The number, size, structure and location of cysts provide specialists with very important information, taking into account which, based on a clinical examination, final conclusions are formed.
Description of NSG is not a diagnosis and not a reason for treatment!
Most often, NSG data provide indirect and uncertain results, and are taken into account only in conjunction with the results of a clinical examination.
Once again, I must remind you of the other extreme: in difficult cases, sometimes there is a clear underestimation on the part of parents (less often, doctors) of the problems the child has, which leads to a complete refusal of the necessary dynamic observation and examination, as a result of which the correct diagnosis is made late, and the treatment does not lead to the desired result. Therefore, if increased intracranial pressure and hydrocephalus are suspected, diagnosis should be carried out at the highest professional level.
What is muscle tone and why do doctors and parents “love” it so much?
Look at your child’s medical record: is there no such diagnosis as “muscular dystonia”, “hypertension” and “hypotension”? — you probably just didn’t go with your baby to the neurologist’s clinic until he was a year old. This is, of course, a joke. However, the diagnosis of “muscular dystonia” is no less common (and perhaps more common) than hydrocephalic syndrome and increased intracranial pressure.
Changes in muscle tone can be, depending on the severity, either a variant of the norm (most often) or a serious neurological problem (this is much less common).
It is sometimes quite difficult for even a competent doctor to notice the difference between physiological changes and pathological symptoms in one consultation. The fact is that changes in muscle tone are not only associated with neurological disorders, but also strongly depend on the specific age period and other characteristics of the child’s condition (excited, crying, hungry, drowsy, cold, etc.). Thus, the presence of individual deviations in the characteristics of muscle tone does not always cause concern and require any treatment.
But even if functional disorders of muscle tone are confirmed, there is nothing to worry about. A good neurologist will most likely prescribe massage and physical therapy (exercises on large balls are very effective). Medicines are prescribed extremely rarely, usually for severe muscle hypertension of a spastic nature.
Hyperexcitability syndrome (syndrome of increased neuro-reflex excitability)
Frequent crying and whims with or without cause, emotional instability and increased sensitivity to external stimuli, sleep and appetite disturbances, excessive frequent regurgitation, motor restlessness and shuddering, trembling of the chin and arms (etc.), often combined with poor growth weight and bowel dysfunction - do you recognize such a child?
All motor, sensitive and emotional reactions to external stimuli in a hyperexcitable child arise intensely and abruptly, and can fade away just as quickly. Having mastered certain motor skills, children constantly move, change positions, constantly reach for and grab objects. Children usually show a keen interest in their surroundings, but increased emotional lability often makes it difficult for them to communicate with others. They have a subtle mental organization, they are very impressionable, emotional and easily vulnerable! They fall asleep extremely poorly, only with their mother, they constantly wake up and cry in their sleep. Many of them have a long-term reaction of fear when communicating with unfamiliar adults with active reactions of protest. Typically, hyperexcitability syndrome is combined with increased mental exhaustion and fatigue.
The presence of such manifestations in a child is just a reason to contact a neurologist, but in no case is it a reason for parental panic, much less drug treatment.
Constant hyperexcitability is not causally specific and can most often be observed in children with temperamental characteristics (for example, the so-called choleric type of reaction).
Much less frequently, hyperexcitability can be associated and explained by perinatal pathology of the central nervous system. In addition, if a child’s behavior is suddenly disrupted unexpectedly and for a long time for virtually no apparent reason, and he or she develops hyperexcitability, the possibility of developing an adaptation disorder reaction (adaptation to external environmental conditions) due to stress cannot be ruled out. And the sooner the child is examined by specialists, the easier and faster it is possible to cope with the problem.
And, finally, most often, transient hyperexcitability is associated with pediatric problems (rickets, digestive disorders and intestinal colic, hernia, teething, etc.).
At an early age, the child’s condition is extremely changeable, so minimal developmental deviations and other disorders of the nervous system can sometimes be detected only during long-term dynamic monitoring of the baby, with repeated consultations. For this purpose, specific dates for planned consultations with a pediatric neurologist in the first year of life have been determined: usually at 1, 3, 6 and 12 months. It is during these periods that most serious diseases of the nervous system of children in the first year of life can be detected (hydrocephalus, epilepsy, cerebral palsy, metabolic disorders, etc.). Thus, identifying a specific neurological pathology in the early stages of development makes it possible to begin complex therapy on time and achieve the maximum possible result.
And in conclusion, I would like to remind parents: be sympathetic and attentive to your kids! First of all, it is your active and meaningful interest in the lives of children that is the basis for their future well-being. Do not try to cure them of “supposed illnesses,” but if you have any concerns or concerns, seek independent advice from a qualified professional.
Author: neurologist S.V. Zaitsev
September 27, 2017
Source