Why does swelling occur during pregnancy?
Physiological reasons
The causes of this manifestation during pregnancy are:
- overwork;
- high ambient temperature, stuffiness, high humidity;
- wearing shoes with heels;
- long walking, long stay in a stationary position;
- drinking large amounts of salt or liquid.
Small patients are prone to developing edema. A predisposing factor is excess weight. In girls with slight excess body weight, pastiness appears more often, but does not reach a significant degree of severity. In patients with severe obesity, the tendency to peripheral edema increases, the symptom becomes permanent, combined with shortness of breath, pain in the spine, and leg joints.
Preeclampsia
Swelling is characteristic of all late toxicoses, which are essentially successive stages of one pathological process. The change of stages can be either gradual or lightning fast, which makes it important to take into account the severity of the symptom and other manifestations to determine the severity of the condition and the need for emergency measures. The following options for gestosis are possible:
- Dropsy of pregnancy.
It develops due to disturbances in the water-electrolyte balance, increased vascular permeability, and the release of fluid into the tissue. At first, the swelling is insignificant, affecting only the limbs, then the swelling becomes generalized. A characteristic external feature is a glossy skin tone. The patient is worried about thirst. There is a decrease in urination. - Nephropathy.
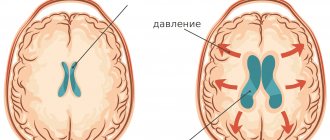
Replaces dropsy in 25% of women. Manifested by edema, proteinuria, increased blood pressure. Swelling varies from slight pastiness of the face and hands to generalized edema. Progressive hypertension is accompanied by headaches, nausea, and vomiting. Other typical symptoms of nephropathy include weakness, dizziness, thirst, shortness of breath, dyspepsia, and lower back pain. - Preeclampsia.
Formed after nephropathy. Swelling persists. The above symptoms are supplemented by heaviness in the back of the head, intense cephalalgia, fatigue, lethargy, lethargy, tremor, sweating of the hands, insomnia or increased drowsiness. A quarter of patients experience visual disturbances. Possible pain in the epigastric region, nausea, vomiting. - Eclampsia.
Replaces preeclampsia for a period not exceeding 3-4 days. Against the background of swelling of the torso and limbs, and other symptoms of preeclampsia, a convulsive seizure occurs, followed by coma, which progresses to restoration of consciousness or worsens.
Inferior vena cava syndrome
Typically diagnosed after 25 weeks of pregnancy. Manifested by tachycardia, weakness, difficulty breathing, increased fetal movement when lying on the back. Cardialgia, fear, anxiety, visual disturbances, noise and ringing in the ears are detected. Postural hypotension develops, and sometimes fainting. Edema with IVC syndrome is found in the lower extremities and is caused by deterioration of blood outflow against the background of compression of a large venous trunk.
Renal pathologies
An increased likelihood of edema during pregnancy is observed in women with a single kidney due to agenesis of the organ or after nephrectomy. An increase in the load on the urinary system can lead to morning swelling of the face, a decrease or increase in urination, the appearance of blood impurities, and cloudy urine. The general condition worsens, drowsiness, weakness, and fatigue are observed. There is a high probability of developing gestational pyelonephritis, which is manifested by dysuria and severe pain similar to renal colic.
Glomerulonephritis occurs against the background of infections, toxic effects, and systemic pathologies. In the acute form of the disease, the face and eyelids suddenly become swollen, weakness, hyperthermia, chills, appetite disturbances, and lower back pain are observed. Urinary output decreases, urine becomes brown, red or pink.
In more than half of patients, glomerulonephritis during pregnancy is chronic. Edema syndrome is pronounced in 5% of patients. Possible involvement of the face, arms, legs. In severe cases, swelling spreads to the entire body, and anasarca develops. The presence of ascites is indicated by a rapid enlargement of the abdomen. Increasing shortness of breath is a sign of hydrothorax.
Varicose veins
In 60-80% of cases, varicose veins are provoked by pregnancy; in other women they are aggravated due to increased stress on the vessels. Typically affects the lower extremities. At the initial stage, a slight pastiness occurs in the evening, especially after prolonged standing, and is combined with a feeling of heaviness and “humming” in the legs. Subsequently, pain and local cramps appear. Severe swelling of the feet, ankles, and lower legs indicates damage to the deep veins.
A rare variant of the disease is genital varicose veins. Swelling of the labia and perineum, bleeding after sexual intercourse, itching, heaviness, and distension in the genital area are possible. There are aching and nagging pains in the lower abdomen and genitals, radiating to the groin, sacrum, and lower back.
Thrombophilia
The pathological condition is caused by disorders of the blood coagulation system and is accompanied by the formation of blood clots. The most common complication of thrombophilia during pregnancy is thrombophlebitis. Swelling of the leg with deep venous thrombosis is combined with bursting pain, cyanosis of the skin, swelling of the superficial veins, increased local temperature, hardening, and soreness of the damaged vessel. Due to thrombosis of the placental vessels, severe gestosis develops with massive edema of the abdomen, upper and lower extremities.
Arterial hypertension
In two thirds of women, it is provoked by pregnancy; after the birth of a child, blood pressure normalizes. There is an increased tendency to edema of the distal legs. Swelling of the hands is possible. The main manifestations of hypertension during pregnancy are dizziness, tinnitus, headaches, increased fatigue, shortness of breath, and tachycardia.
Heart diseases
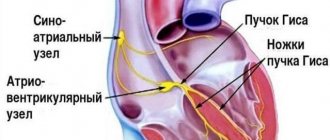
The main cardiac cause of swelling during pregnancy is considered to be circulatory failure due to rheumatic or congenital heart defects. Swelling occurs mainly in the lower extremities: legs, feet, ankle joints. Drowsiness, muscle weakness, fatigue, interruptions in heart function, shortness of breath, bluish tint or pale skin are observed. A more rare cardiac pathology that provokes the development of edema is dilated cardiomyopathy.
Thyroid pathologies
Iodine deficiency, which is quite common in pregnant women, causes edema only when the level of thyroid hormones decreases. In severe cases, clinically significant hypothyroidism develops. The most noticeable swelling is observed on the face and neck, sometimes affecting the entire body. The face is mask-like, puffy. There are no changes in skin color or pressure marks. Rapid weight gain, lethargy, constipation, nausea, and deterioration in the condition of hair and nails are observed.
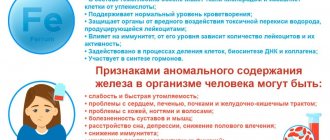
Hypovitaminosis
Swelling, cramps, lethargy, and early toxicosis are observed in pregnant women with hypovitaminosis B6. These symptoms are aggravated by a concomitant deficiency of vitamins B9 and B12. The development of a specific clinical picture is preceded by apathy, weakness, drowsiness, decreased appetite, deterioration in concentration, and a tendency to catch colds.
Arterial hypertension in pregnant women
Chronic hypertension
The prevalence of
chronic hypertension
in pregnant women is 1-5%.
This figure increases with age, and is also higher in obese women. The
diagnosis is based on anamnestic data (pressure level before pregnancy) or an increase in pressure to 140/90 mm Hg. and more until the 20th week of pregnancy. It is very difficult to diagnose chronic hypertension in pregnant women if the pressure before pregnancy is unknown. In such cases, diagnosis is usually based on the presence of hypertension before the 20th week of pregnancy. However, in some women, hypertension during these periods may be the first manifestation of preeclampsia. Moreover, due to the physiological decline in blood pressure during the second trimester, many women with chronic hypertension have normal blood pressure levels before the 20th week of pregnancy.
Hypertension is often classified as mild, moderate, severe, or very severe based on systolic or diastolic pressure levels. During pregnancy, chronic hypertension may be classified as mild or severe .
Although there is no clear definition of mild hypertension, it is generally accepted that a diastolic pressure level of 110 mm Hg or higher (Korotkoff sound V) indicates severe hypertension.
Newborns born to women with chronic hypertension have a serious prognosis, which is mainly due to preeclampsia.
Neither worsening hypertension nor edema are reliable indicators of developing preeclampsia.
The best indicator of preeclampsia is the occurrence of proteinuria (at least 300 mg in 24 hours) in the absence of kidney disease. Risk to Maternal and Fetal
Pregnant women with chronic hypertension have an increased risk of developing preeclampsia and placental abruption, and their babies have increased perinatal morbidity and mortality. The likelihood of these complications is especially high in women who have suffered from severe hypertension for a long time or have cardiovascular and renal pathology. In addition, maternal and child morbidity and mortality increase if a pregnant woman had a diastolic pressure of 110 mm Hg or more during the first trimester.
In contrast, outcomes in women with mild, uncomplicated chronic hypertension during pregnancy and in their children are similar to those in healthy pregnant women.
Treatment
Retrospective studies in pregnant women suggest that antihypertensive therapy reduces the incidence of stroke and cardiovascular events in pregnant women with diastolic blood pressure greater than 110 mmHg.
There is general agreement that pregnant women with severe hypertension should receive drug therapy, but it is unclear how appropriate such therapy is for mild essential hypertension.
The benefits of long-term therapy aimed at lowering blood pressure in non-pregnant, middle-aged and elderly people with diastolic pressure less than 110 mmHg (mild hypertension) are well known. These benefits are greatest after 4 to 6 years of treatment in men over 50 years of age who have risk factors for cardiovascular disease or stroke. However, the majority of pregnant women with mild chronic hypertension are under 40 years of age and have uncomplicated hypertension. Therefore, treatment of mild chronic hypertension in pregnant women is not justified.
.
It is essential that antihypertensive therapy in pregnant women with mild hypertension reduces the risk of preeclampsia, placental abruption, preterm birth, and perinatal mortality.
Currently, there remains uncertainty regarding the appropriateness of treatment for pregnant women with mild chronic hypertension.
Antihypertensive drugs may have harmful effects on the mother, fetus, or newborn,
with some effects appearing after the neonatal period. Antihypertensive drugs can have both an indirect effect on the fetus, by reducing uteroplacental blood flow, and a direct effect, by affecting the umbilical or cardiovascular circulation of the fetus.
Methyldopa is most commonly used to treat chronic hypertension in pregnant women .
Short-term (on average 24 days) therapy with methyldopa during the third trimester does not affect uteroplacental blood flow and fetal hemodynamics.
In addition, after long-term use of methyldopa in pregnant women, no immediate or delayed effects on the fetus and newborn were observed. Atenolol
, on the contrary,
has a pronounced effect on uteroplacental blood flow and fetal hemodynamics
, as well as on fetal growth. Data on the side effects of other beta-blockers when used during pregnancy are contradictory. Moreover, there are no studies on the long-term effects of these drugs in children.
A meta-analysis of 9 randomized trials comparing diuretic therapy with no treatment in 7000 normotensive pregnant women found no difference in the prevalence of side effects between the two groups. The effect of diuretics on fetal growth has not been analyzed. therapy
in pregnant women with mild chronic hypertension leads to a decrease in plasma volume, which can be extremely unfavorable for fetal growth.
The use of angiotensin-converting enzyme inhibitors during pregnancy is contraindicated as these drugs are associated with fetal growth restriction, oligohydramnios, congenital deformities, neonatal renal failure and neonatal death.
Women with chronic hypertension should be assessed before conception
, so that drugs that may be harmful to the fetus (angiotensin-converting enzyme inhibitors and atenolol) are replaced by other drugs such as methyldopa and labetalol. Many women with chronic hypertension receive diuretics; There are differing opinions on whether such therapy should be continued during pregnancy.
When deciding whether to initiate drug therapy in women with chronic hypertension, the severity of hypertension, the potential risk of end-organ damage, and the presence or absence of preexisting cardiovascular pathology must be considered.
The first-line drug is
methyldopa
.
If there are contraindications to its use (such as drug-induced liver damage) and if it is ineffective or intolerable, labetalol
.
Gestational hypertension
Gestational hypertension refers to the occurrence of high blood pressure without other symptoms of preeclampsia after the 20th week of pregnancy in women who previously had normal blood pressure.
In some women, gestational hypertension may be an early manifestation of preeclampsia, while in others it may be a sign of unrecognized chronic hypertension.
In general, the outcome of pregnancies with gestational hypertension is good without drug therapy
.
Preeclampsia
Traditionally, preeclampsia is understood as the appearance of hypertension, edema and proteinuria after the 20th week of pregnancy with previously normal blood pressure
.
The differences between preeclampsia and gestational hypertension are summarized in Table 1. In general, preeclampsia is defined as hypertension plus hyperuricemia or proteinuria
;
it is graded as mild or severe depending on the degree of elevation of blood pressure, the severity of proteinuria, or both. There is currently no agreement on the definition of mild hypertension, severe hypertension, or severe proteinuria. However, focusing on hypertension or proteinuria may minimize the clinical significance of other organ disorders. For example, some women with hemolysis, elevated liver enzymes, and low platelets (HELLP syndrome) have life-threatening complications
(pulmonary edema, acute renal failure, or liver rupture), but there is little or no hypertension with minimal proteinuria.
Moreover, among women with preeclampsia who develop seizures (eclampsia), diastolic pressure is less than 90 mmHg and there is no proteinuria in 20% of cases. Some women with preeclampsia have signs and symptoms that are mistaken for other disorders (Table 2). Etiology and pathogenesis
One of the earliest abnormalities found in women who later develop preeclampsia is the lack of penetration of trophoblast cilia into the spiral arteries of the uterus
.
This placentation defect leads to impaired cardiovascular adaptation (increased plasma volume and decreased systemic vascular resistance) characteristic of normal pregnancy. In preeclampsia, both cardiac output and plasma volume are reduced, while systemic vascular resistance is increased. These changes cause decreased perfusion of the placenta, kidneys, liver, and brain. Endothelial dysfunction, manifested by vasospasm, changes in vascular permeability and activation of the coagulation system, may explain many clinical manifestations in women with preeclampsia. Indeed, many of the pathological manifestations described in such women are associated with decreased perfusion rather than the damaging effects of hypertension. Complications
The main dangers for women associated with preeclampsia are road accidents, cerebral hemorrhage, placental abruption with disseminated intravascular coagulation, pulmonary edema, and renal failure .
The greatest danger to the fetus is severe growth retardation, hypoxemia, and acidosis.
The frequency of these complications depends on the stage of pregnancy at the time of the onset of preeclampsia, the presence or absence of associated complications, the severity of preeclampsia and the quality of medical care. In women with mild preeclampsia who are closely monitored, the risk of developing seizures is 0.2%, placental abruption is 1%, and fetal or neonatal death is less than 1%. The incidence of fetal growth restriction ranges from 5 to 13%, preterm birth - from 13 to 54%, depending on the stage of pregnancy at the time of onset and the presence or absence of proteinuria. In contrast, maternal and infant morbidity and mortality are significant among women with eclampsia and those who develop preeclampsia before the 34th week of pregnancy. Treatment
Early diagnosis, careful medical monitoring and timely delivery are cardinal requirements in the treatment of preeclampsia; childbirth leads to
.
Once a diagnosis is made, further tactics are determined by the results of a study of the condition of the mother and fetus. Based on these results, a decision is made on the need for hospitalization, expectant management or delivery. This takes into account factors such as the severity of the pathological process, the condition of the mother and fetus, and the duration of pregnancy. Regardless of the treatment strategy chosen, the main goal should be, firstly, the safety of the mother
and, secondly,
the birth of a viable child
who will not require long-term intensive care.
Mild degree.
Women with preeclampsia need
careful monitoring
, as sudden deterioration of the condition is possible.
The presence of symptoms (such as headache, epigastric pain and visual disturbances) and proteinuria increases the risk of eclampsia and placental abruption
;
For women with these symptoms, observation in a hospital is indicated. Outpatient observation is possible with strict adherence to recommendations, mild hypertension and normal fetal condition. Monitoring includes monitoring of maternal blood pressure, weight, urinary protein excretion, platelet count, and fetal condition
.
In addition, the woman should be informed about the symptoms of increasing preeclampsia.
As the disease progresses, hospitalization is indicated. It is generally accepted that in women with mild preeclampsia who have reached their due date, labor should be induced to avoid complications for the mother and fetus. In contrast, there is no consensus on the management of mild preeclampsia in earlier stages of pregnancy. The greatest differences of opinion concern the need for bed rest, prolonged hospitalization, antihypertensive therapy, and seizure prevention.
Bed rest is usually recommended for women with mild preeclampsia
at home or in a hospital. It is believed to help reduce swelling, improve fetal growth, prevent the development of severe preeclampsia and improve pregnancy outcomes.
Severe degree.
Severe preeclampsia can progress rapidly, leading to sudden deterioration of both mother and fetus;
in this case, immediate delivery is indicated, regardless of the duration of pregnancy. Urgent delivery is clearly indicated in case of threat of eclampsia, multiple organ dysfunction, pathological condition of the fetus, or the development of severe preeclampsia after the 34th week. However, early pregnancy can be continued under close monitoring to improve neonatal survival and reduce neonatal morbidity. Three recent studies have shown that conservative treatment of women with severe preeclampsia who have not reached their due date results in a reduction in neonatal morbidity and mortality
.
However, because only 116 women received conservative therapy in these studies, and such therapy may pose some risk to the mother and fetus, conservative treatment should be carried out in perinatal centers and include very careful monitoring of the mother and fetus.
The main goal of treatment for women with severe hypertension and preeclampsia is to prevent cerebral complications such as encephalopathy and stroke. The indication for drug treatment is a diastolic pressure level of 110 mmHg. and higher.
Some experts recommend starting treatment at a diastolic pressure of 105 mm Hg. and even less, while others consider a mean arterial pressure value exceeding 125 mm Hg as an indication for starting treatment.
The goal of treatment is to maintain mean arterial pressure at a level not exceeding 126 mm Hg. (but it should not be lower than 105 mmHg) and diastolic pressure - no higher than 105 mmHg. (but not lower than 90 mm Hg) .
The first-line drug for women with severe peripartum hypertension is
hydralazine
, administered intravenously at a dose of 5 mg.
If necessary, administration can be repeated every 20 minutes until a total dose of 20 mg is reached. If the indicated dose of hydralazine does not achieve the desired result, or if the mother experiences adverse reactions such as tachycardia, headache, nausea, labetalol
(20 mg intravenously) can be used; if labetalol is ineffective, then
nifedipine
at a dose of 10 mg/day
. Because hydralazine may cause fetal impairment, some researchers recommend the use of other drugs to treat severe preeclampsia (dihydralazine, diazoxide)
.
Women with preeclampsia have an increased risk of developing seizures
. The degree of risk depends on the severity of preeclampsia and the characteristics of the woman’s body. For many years, experts in the United States have recommended prophylactic use of magnesium sulfate during labor and the postpartum period for all women with preeclampsia. In contrast, experts in other countries considered lowering maternal blood pressure to be an adequate preventive measure. This discrepancy is not surprising because the prevalence of eclampsia in women with preeclampsia is very low and varies widely among different groups of women.
Two randomized trials examined the effectiveness of prophylaxis with magnesium sulfate in women with preeclampsia. In one study, an antihypertensive drug was used in combination with magnesium sulfate in 112 women with severe preeclampsia, and an antihypertensive drug as monotherapy in 116 patients. There was one case of eclampsia in the group of women receiving magnesium sulfate and no cases in the other group. Another study compared magnesium sulfate and phenytoin in preventing eclampsia in 2,137 women with mild preeclampsia. There were 10 cases of eclampsia (1%) in the phenytoin group and no cases in the group of women receiving magnesium sulfate.
In a recent large study, magnesium sulfate was more effective than phenytoin and diazepam in treating and preventing seizures in women with eclampsia.
Therefore, all women with eclampsia should receive magnesium sulfate during labor and for at least 24 hours after delivery. Prevention
For many years, salt restriction and diuretic medications have been used to prevent preeclampsia. It is now known that dietary sodium restriction during pregnancy reduces circulating blood volume without reducing the incidence of hypertension
.
Epidemiological studies suggest that normal calcium intake during pregnancy is effective in reducing the risk of hypertension
, but the effect on preeclampsia (defined as hypertension + proteinuria) was small.
Conclusion
When monitoring pregnant women with hypertension, it is important to distinguish between chronic hypertension, gestational hypertension and preeclampsia. Antihypertensive therapy allows such women to carry their pregnancy to full term. Careful medical supervision and timely delivery are key points in the treatment of hypertension in pregnant women.
| Applications to the article |
| Criteria used to diagnose preeclampsia: • exacerbation of hypertension; • swelling; • proteinuria; • hyperuricemia; • combinations of these manifestations. |
| An indicator of the development of preeclampsia is proteinuria (i300 mg/day) |
| Early diagnosis, careful medical supervision and timely delivery are cardinal requirements in the treatment of preeclampsia |
| All women with eclampsia should receive magnesium sulfate during labor and for 24 hours after delivery. |
Diagnostics
An obstetrician-gynecologist determines the cause of a symptom during pregnancy. According to indications, the patient is referred for consultation to a nephrologist, phlebologist, cardiologist, and other specialists. The examination is carried out using the following methods:
- Anamnesis collection.
The doctor interviews the patient, identifying clinical signs of swelling. Swelling of the feet is indicated by the feeling that the usual shoes have become tight, the inability to fasten the boots, and pronounced, long-lasting marks from the elastic bands of socks on the skin. Swelling of the hands is indicated by problems when removing and putting on rings. - Physical examination.
The specialist determines the prevalence of edema and identifies manifestations indicating the etiology of the symptom. Detects external and palpation signs of ascites and anasarca, listens to the heart and lungs to identify defects and hydrothorax. - Special measurements.
Indicated for suspected hidden edema. Based on determining daily weight gain and diuresis calculation. Normally, the weekly increase in body weight is less than 300 g, the daily volume of fluid consumed exceeds the amount of urine by no more than 20-25%. Deviation of these indicators indicates a high probability of swelling. - Hardware methods.
Safe, fairly informative ultrasound and electrophysiological studies are recommended. A gynecological ultrasound and Doppler ultrasound of the uteroplacental blood flow are performed. For pathologies of the urinary system, ultrasound of the kidneys is prescribed, for hypothyroidism - ultrasound of the thyroid gland, for varicose veins and thrombophlebitis - ultrasound of the lower extremities. Cardiological patients, along with echocardiography, undergo ECG, daily monitoring, and phonocardiography. - Lab tests.
For kidney disease, general and biochemical urine tests are indicated; for hypothyroidism, hormone tests are indicated. To determine the presence and type of thrombophilia, special studies are carried out. Laboratory examination for gestosis includes CBC, OAM, biochemical blood and urine tests, and coagulogram.
Publications in the media
Proteinuria is the excretion of protein in the urine in an amount of more than 50 mg/day, the most common sign of kidney damage.
Classification • Organic - due to kidney pathology, less often - extrarenal pathology • Functional (not associated with kidney disease) •• Orthostatic •• Lordotic •• Physical stress •• Fever •• Stressful •• Cold •• Idiopathic •• Obesity (with body weight more than 120 kg) • By protein composition •• Selective - represented by a protein with a molecular weight of less than 65,000 Da (mainly albumin) or a protein of a certain molecular weight (Bence-Jones protein in myeloma nephropathy) •• Non-selective - medium- and high molecular weight protein • Degree of proteinuria •• Microalbuminuria - less than 30 mcg/day •• Minimal - less than 1 g/day •• Moderate - 1-3 g/day •• Massive (nephrotic) - more than 3-3.5 g/day ( leading sign of nephrotic syndrome). Etiology • Glomerular proteinuria •• Glomerulonephritis •• Renal amyloidosis •• Diabetic glomerulosclerosis •• Renal vascular thrombosis •• Hypertension •• Congestive kidney • Tubular proteinuria •• Pyelonephritis •• Interstitial nephritis •• Urolithiasis •• Gouty nephropathy •• Kalipenic kidney •• Acute tubular necrosis •• Chronic renal graft rejection •• Fanconi syndrome • Overflow proteinuria •• Myeloma nephropathy (Bence Jones proteinuria) •• Myoglobinuria (long-term crush syndrome) •• Lysocymuria (leukemia) •• Hemoglobinuria (intravascular hemolysis). Pathogenesis. Increased filtration of protein from plasma through the glomerular filter (glomerular proteinuria, overflow proteinuria) and/or decreased tubular reabsorption of filtered protein (tubular proteinuria). Pathomorphology • Renal proteinuria - depends on the underlying disease •• Immune inflammation in glomerulonephritis •• Deposition of amyloid masses in renal amyloidosis •• Thickening of the glomerular basement membrane, expansion of the mesangium in diabetic glomerulosclerosis • Extrarenal proteinuria and overflow proteinuria - dystrophic changes in the tubular epithelium are possible • Functional proteinuria - no changes.
Clinical manifestations • Caused by the underlying disease • Possible foamy urine with massive proteinuria • Proteinuria can be a symptom of acute nephritic or nephrotic syndromes; with a relatively rapid, abrupt increase, it acts as a sign of increased activity of glomerulonephritis. Diagnostics • Detection of the fact of proteinuria •• Using strips, precipitation with sulfosalicylic or trichloroacetic acid with refractometry (methods allow you to determine the protein concentration > 20 mg / day) •• Biuret method (azotometric) •• Radioimmune method (allows you to detect prealbumin, albumin, transferrin, 2-microglobulin, 2-macroglobulin, -globulin, etc.) • Clarification of the degree of proteinuria (study of protein in daily urine) • Clarification of the nature of proteinuria - Bence-Jones protein, 2-microglobulin, myoglobin, etc.
Differential diagnosis . Determination of the glomerular or tubular nature of proteinuria. Detection of functional proteinuria. Treatment • With functional proteinuria, there is no need for treatment • Organic proteinuria •• With glomerular proteinuria - protein restriction in the diet •• Drug treatment is determined by the underlying disease.
ICD-10 • N06 Isolated proteinuria with specified morphological lesion • N39.1 Persistent proteinuria, unspecified • N39.2 Orthostatic proteinuria, unspecified • O12 Pregnancy-induced edema and proteinuria without hypertension • O14 Pregnancy-induced hypertension with significant proteinuria • R80 Isolated proteinuria
Treatment
Conservative therapy
Depending on the cause of the symptom, the following treatment measures are carried out:
- Preeclampsia.
Patients are hospitalized (except for cases of mild dropsy). Bed rest is prescribed. Correction of the drinking regime, a special diet with an increased amount of protein, and salt restriction are indicated. Diuretics are not recommended, as they can aggravate the release of vascular fluid into the tissue and contribute to the increase in edema. Antispasmodics, desensitizing, hypotensive, sedative and anticonvulsants, infusion therapy, and oxygen therapy are used. - Kidney diseases.
A special diet is prescribed. In mild cases, herbal remedies are used. For clinically significant forms of glomerulonephritis, the treatment regimen includes loop diuretics, xanthines, potassium-containing agents, antihypertensive drugs, and antiplatelet agents. If you have a solitary kidney, hormones and antibiotics may be required. Iron supplements are needed to increase hemoglobin levels. Pulsed ultrasound is effective in the lumbar region. - Varicose veins
Compression therapy, treatment with phlebotonics and phleboprotectors, anticoagulants, and antiplatelet agents are carried out. Moderate physical activity, lymphatic drainage massage, physical therapy, and a diet with plenty of vegetable fats and fiber are helpful. - Thrombophilia.
Patients with thrombosis are prescribed anticoagulants and thrombolytics. In case of blood rheology disorders, antiplatelet agents are used prophylactically. Hemodilution (erythrocytopheresis, thrombocytopheresis) and hirudotherapy are performed. If there is a lack of coagulation factors and anticoagulants, fresh or fresh frozen plasma is transfused. Sometimes plasmapheresis is necessary. - Arterial hypertension.
As part of antihypertensive therapy, alpha-2 adrenergic agonists, selective beta blockers, myotropic vasodilators, and slow calcium channel blockers are prescribed. To improve microcirculation and metabolic processes in the fetoplacental system, peripheral vasodilators are used. Diuretics and ACE blockers are not recommended for pregnant women with hypertension. - Damage to the thyroid gland.
The basis of treatment is hormonal and iodine-containing medications. For organ disorders due to hypothyroxinemia, cardioprotectors, antiarrhythmic drugs, immunostimulants, vitamin-mineral complexes, and nootropics are additionally used. - Heart defects.
Therapy includes antibiotics, nitrates, beta blockers, cardiac glycosides, anticoagulants, loop and thiazide diuretics. Treatment regimens are drawn up individually, taking into account the characteristics of the pathology, the severity of symptoms, and the duration of pregnancy.
Surgery
Natural childbirth is generally the preferred option. If necessary, caesarean section and minor obstetric operations are performed. Sometimes early delivery is required. Specific surgical treatment is postponed, if possible, until pregnancy or lactation is completed. Patients with varicose veins undergo crossectomy, miniphlebectomy, and endovasal laser coagulation according to indications. Minimally invasive methods for treating heart defects are closed mitral commissurotomy and balloon dilatation of aortic stenosis.