What is hydrocephalus?
The term hydrocephalus is formed from two Greek words: “hydro” - water and “cephalus” - head (“dropsy of the brain”). In hydrocephalus, there is a significant buildup of cerebrospinal fluid (CSF) inside cavities of the brain called ventricles. An increase in the volume of cerebrospinal fluid (CSF) occurs when the balance between the production of cerebrospinal fluid and its absorption and further removal from the body is disturbed. This may be the result of a deficiency in the circulatory system or excessive production of cerebrospinal fluid. Hydrocephalus can be congenital or acquired. The concept of congenital hydrocephalus means that it appears from the moment of birth. The disease can be provoked by various factors: traumatic brain injury, brain tumor, necrosis, meningitis, etc. The frequency of this disease is high throughout the world. According to the literature, hydrocephalus affects 5-15 children out of every thousand newborns. Treatment consists of diverting CSF outside the cerebrospinal fluid system into body cavities where it can be absorbed (absorbed). An effective operation allows a child to live and develop normally, study in a regular school, and an adult to return to a full, active life. However, patients and their loved ones must be able to recognize the signs and symptoms of postoperative complications so that medical care can be provided in a timely manner.
Classification
Based on the openness of the cerebrospinal fluid outflow pathways, hydrocephalus occurs:
- closed;
- communicating;
- substitutive.
According to the characteristics of the deformation of the outflow tract:
- internal;
- external;
- mixed.
By type of cerebrospinal fluid pressure:
- hypotensive;
- hypertensive;
- normotensive.
By etiology:
- congenital;
- after the inflammatory process;
- tumor;
- vascular;
- idiopathic.
Other types of classification:
- with the flow;
- by compensation phase;
- by activity;
- according to the speed of development.
Anatomy and physiology
In order to better know and understand the disease, we will give you some information about the anatomy of the skull, the structure of the brain, as well as the process of formation and absorption of cerebrospinal fluid (Fig. 1). The brain occupies most of the cranial cavity. It is penetrated by a large number of blood vessels and is surrounded by cerebrospinal fluid as a buffer. The fluid is located in 4 cavities (ventricles) located inside the brain. The ventricles have delicate structures known as villous plexuses (choroid plexuses). These structures produce a significant amount of CSF - about 500 ml per day. The fluid circulates continuously and contains a large number of substances essential for nutrition and ensuring the normal functioning of the nervous system.
CSF also provides a protective cushion for the brain. CSF circulates in the ventricular system and is removed through 3 holes in the 4th ventricle and then enters the subarachnoid space surrounding the brain and spinal cord.
CSF constantly circulates in the brain and spinal cord, constantly being in the process of a) formation, b) circulation and c) absorption. In a healthy body these processes are balanced. Hydrocephalus develops if CSF is not cleared from the ventricular system through the cerebrospinal fluid tract. Less commonly, hydrocephalus is caused by excess production of CSF, such as with villous plexus papilloma.
Cause
Neurosurgeons count more than 180 reasons that can cause the development of hydrocephalus. It can be congenital (when a child is born with an excess amount of cerebrospinal fluid in the head) or acquired as a result of other problems:
– traumatic (develops after a trauma, for example, birth trauma, cerebral hemorrhage), – inflammatory (develops after neuroinfections), – tumor (the tumor blocks the outflow of cerebrospinal fluid or stimulates increased production), – vascular (due to vascular diseases of the brain), – idiopathic (when the reason is not clear).
At risk are premature babies and children with excised spina bifida (since the spinal cord is connected to the brain, hydrocephalus often manifests itself as a concomitant disease). Most often, hydrocephalus is detected before the age of three months; boys develop it more often than girls.
Diagnostics
In newborn children, the bones of the skull have not yet fused and hydrocephalus is determined visually. The head enlarges, the bones of the skull diverge, the fontanelle is tense and bulging; the skin is thin and shiny; The veins in the hairline area look full and swollen. Also symptoms are: vomiting, apathy, excitability, downward displacement of the eyes (“setting sun symptom”), etc. However, when the cranial sutures are not fused, the signs and symptoms of increased intracranial pressure seem subtle.
In older children and adults, the bones of the skull are fused and, when the ventricles expand, compression of the brain tissue occurs. Symptoms of increased intracranial pressure appear: headaches, nausea, vomiting, blurred vision, lack of coordination, psychopathological personality changes, lack of concentration and lethargy. These symptoms require additional instrumental diagnosis.
Signs of the disease
The symptoms of the disease are dictated mainly by reduced perfusion of brain tissue, overstretching of groups of nerve fibers (conducting pathways) due to increased ICP.
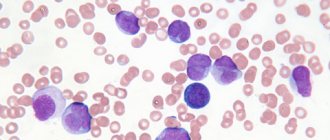
- In acute pathogenesis, weak microcirculation (hypoperfusion) leads mainly only to functional disorders of intracranial metabolism. This is
a change in energy metabolism, a reduction in the level of creatine phosphate and ATP, an increase in the concentration of lactic acid and inorganic salts of phosphoric acids. The acute clinical picture is reversible. - The long-term existence of hypoperfusion causes irreversible transformations at the structural level. These are
defects in the vascular endothelium and disruption of the BBB, axonal damage (destruction of axons, up to their complete disappearance). Dropsy of prolonged duration ultimately causes brain atrophy. - The morphology of signs in hydrocephalus in combination with high intracranial pressure is characterized, first of all, by atrophy of the substance of the brain and periventricular edema. There is also damage to the vascular mesenchyme, disruption of brain homeostasis, axonal lesions, and in rare cases, neuronal death. These signs are combined with the clinical picture of the primary pathology that provoked hydrocephalic syndrome.
The symptomatic complex characteristic of hydrocephalus in early childhood includes such distinctive features as:
- increased head size;
- frequent regurgitation;
- restless behavior of the child;
- bulging of a large fontanel;
- divergence of cranial sutures;
- the severity of the venous pattern on the scalp;
- delayed psychomotor development, less often physical;
- throwing the head back;
- “setting sun” syndrome (Graefe);
- congestive optic disc;
- paraplegia of the lower extremities (in severe, advanced conditions).
In adults and older children, the clinical picture depends on the rate of progression of hydrocephalus. In the acute form of the disease, combined with high ICP, the following are observed:
- a bursting and pressing headache that spreads to the orbits of the eyes (one of the features is the peak of pain in the morning after a night's sleep, and then, during the day, the severity of the pain syndrome decreases);
- nausea, which usually accompanies morning headaches (vomiting often occurs in the morning, after which a person notices an improvement in the condition);
- visual disturbances usually include blurred vision, blurred vision, double vision and a burning sensation in the eyes;
- fatigue, drowsiness, lethargy;
- convulsive phenomena (like an epileptic seizure);
- when the brain stem is compressed due to dislocation of brain structures - oculomotor disorders, forced head position syndrome, clouding of consciousness (up to a coma), respiratory failure.
Hydrocele of the brain in the chronic stage manifests itself:
- signs of dementia (dementia), emotional instability;
- apraxia of walking, more often it manifests itself with a shaky and uncertain gait, disproportionately large steps (being in a lying position, patients often do not experience difficulties in imitating walking and twisting a “bicycle” with their legs);
- decreased muscle strength, sometimes patients complain of pain in the neck;
- severe imbalance (in the final stages), which is expressed by a person’s inability to move and sit independently;
- partial or complete loss of sensitivity (not always!):
- urinary and/or fecal incontinence (with a massive lesion).
The pathology is dangerous due to its life-threatening complications! In no case should you ignore an urgent visit to the doctor if one or more symptoms from the lists provided are identified. Timely visit to the hospital for the purpose of diagnosis and receiving adequate medical care increases the chances of a favorable prognosis, including complete recovery.
On average, out of 10 patients who do not receive treatment at the right time, 6-7 people die soon (this also applies to children). Those who did not undergo therapy but survived are doomed to disability with neurological disorders, mental and physical disabilities with a tendency to progress.
Types of diagnostic tests
- Ultrasound is a simple, inexpensive test that helps evaluate the extent to which the ventricles of the brain are dilated. Currently, it is the simplest and safest method for diagnosing hydrocephalus.
- Computed tomography (CT) - This is a technique of drawing with a thin beam the contours of the skull, brain, ventricles and subarachnoid space. It is carried out to determine the size and shape of the ventricles and identify abnormalities such as tumors, cysts or other pathologies.
- Magnetic resonance (nuclear magnetic resonance NMR) is a non-surgical diagnostic method that uses radio signals and a magnet. MRI data determines the shape and severity of hydrocephalus. These studies are indispensable for clarifying the causes of dropsy.
- Cisternography (radiography of the cisterns at the base of the skull) is a test that requires the injection of a radioactive substance into the CSF. It is used to clarify the type of hydrocephalus: communicating or obstructive, as well as to determine the direction of CSF flow.
- Pneumoencephalography is now used much less frequently than in the past. In some cases, it is necessary to pump air with a needle into the spinal cord.
- Angiography (X-ray of blood vessels) is a special technique for injecting a contrast agent into the arteries that cross the brain. After some time, anomalies are detected at the level of blood vessels and the presence or absence of pathological disorders.
- A neuropsychological examination consists of a series of questions and answers to identify the presence of abnormalities in the functioning of the brain.
Endoscopic operations
Endoscopic surgical techniques are used in the treatment of occlusive hydrocephalus, among them:
- ventriculocisternostomy;
- ventricular cystocisternostomy;
- ventriculoplasty of the aqueduct of Sylvius;
- septostomy;
- etiotropic endoscopy (getting rid of the causative factor - removal of a tumor, cyst, hematoma, etc.).
In 90% of cases, the method of endoscopic ventriculocisternostomy is used. The purpose of this operation is perforation of the bottom of the third ventricle of the brain under endoscopic control through a miniature trepanation window. The anastomosis created during the endoscopic procedure allows you to restore the natural path of outflow of cerebrospinal fluid between the third ventricle and the basal cisterns of the brain.
Endoscopy of any kind is a more gentle tactic of neurosurgery; it does not require the implantation of foreign bodies into the body and is less likely to cause postoperative consequences. Despite the promising characteristics of endoscopic methods, in some cases it is impossible to do without shunting or the use of open microsurgery.
Modern neurosurgery technologies have been honed to perfection in the Czech Republic; brain surgery in this country is a leading field of medicine. Neurosurgical care in clinics in the Czech Republic is no worse than in Germany and Israel, but the price is much lower (about 2 times). People with this diagnosis are operated on here at the most exemplary level, and upon completion of the full course of rehabilitation they are discharged with excellent and good results.
Treatment
Currently, occlusive (obstructive) hydrocephalus is treated surgically. Surgical intervention consists of draining excess cerebrospinal fluid outside the cerebrospinal fluid system: into the abdominal (abdominal) cavity or into the atrium. Sometimes CSF may be drained into the pleural cavity. In these cavities, cerebrospinal fluid is absorbed and excreted along with waste products of the body.
To drain the CSF, the surgeon implants a drainage system (shunt). The system material is silicone and polypropylene. Both of these materials are well tolerated by the body. All elements of the system are implanted under the skin; there are no external areas.
Shunt System Components
The system consists of two catheters and one one-way valve. The ventricular catheter is located in the ventricle of the brain, and the peripheral (peritoneal or cardiac) catheter is placed in the abdominal cavity or in the right atrium, respectively. Both catheters are connected to a valve that regulates the unidirectional flow of cerebrospinal fluid. The valves are designed to operate in different pressure ranges (high, medium, low and very low). The neurosurgeon, having determined the patient’s intracranial pressure, selects the appropriate valve, depending on the severity of the disease, the patient’s age and clinical nuances.
Almost all valve models have a reservoir that your doctor can use to “bleed” the system to determine if it is working properly. From the reservoir, by inserting a thin needle through the skin, you can take samples of cerebrospinal fluid for laboratory tests or administer medications. Patients and their loved ones are not recommended to test the drainage system by “bleeding” the reservoir. This action can be dangerous unless your doctor has given you specific instructions about it. In patients suffering from non-communicating (obstructive) hydrocephalus, cerebrospinal fluid should be drained from the cerebral ventricle using a ventricular catheter. In patients with communicating hydrocephalus, a CSF drainage system is implanted from the lumbar space of the spine into the abdominal cavity - the lumboperitoneal system.
Varenka: they weren’t the ones who pulled them out!
When Lena brought her Varya home to Sortavala one year ago, and she was admitted to their local hospital, the doctors threw up their hands in bewilderment:
“We’ll lie down and watch.” - You mean die? - Well, yes.
And then Lena realized that she couldn’t just wait for her daughter to die. She called a paid ambulance and rushed to St. Petersburg. And from there by train, with Varya in her arms, to Moscow. “She will die on your way!” - they told her goodbye at the hospital. But she found a paid doctor who would accompany her and went.
She already knew that in Moscow there was Dmitry Zinenko, for whom hydrocephalus was not a death sentence or a horror story.
“And they weren’t the ones who pulled it out,” said Dmitry Yuryevich, looking at Varya, whose head weighed four kilograms out of six kilograms of total weight.
In Moscow, Vara was fitted with a new shunt, brought into the atrium, and later into the abdominal cavity. And the girl came to life. Lena and Varya completed two courses at the St. Petersburg rehabilitation center. And after the first year, Varya began to raise her head. And a year later she began to roll over, crawl, sit up and walk along the support.
– The main thing is that we are now at home and all together! – Lena couldn’t be happier.
Three-year-old Styopa, developed for his age, dashingly climbed onto a chair and reached for the paints that his mother had hidden. And now she and Varya are already painting something on the floor. They worked well together - twins.
“The relatives in Var dote on their souls,” says Lena. “And the main thing is that since Varya returned home, we never have quarrels, no one yells at anyone. Unless the children fight with each other sometimes. Well, children!
Surgery and hospitalization
Implantation of the shunt system is carried out by a neurosurgeon under sterile operating room conditions. In preparation for surgery, the hair is shaved to achieve maximum cleanliness. The operation is performed under general anesthesia, usually not for a very long time. The neurosurgeon drills a small hole in the skull bone, then makes a small incision in the dura mater that protects the brain and inserts a ventricular catheter into the lateral ventricle. To implant the rest of the bypass system, another incision is made and a tunnel is created subcutaneously to implant a peritoneal or cardiac catheter. The end of the catheter is carefully inserted either into the abdominal cavity or into the jugular vein leading to the ventricle of the heart. Catheters are connected to the valve using connectors on the valve itself. All parts of the shunt are thus connected into a single drainage system. At the end of the operation, small sterile dressings are applied to each incision.
Immediately after the operation, the patient is taken to the postoperative department. The patient is here from 1 hour to 1 day under close observation, then he is transferred to the ward. Most patients are discharged 7-10 days after clinical rehabilitation.
Alenka: she can do anything!
For 10 years, Svetlana tirelessly explains to neurologists at appointments that a “ventricle” is not a “small stomach”, it is a part of the brain. And the shunt is not in my daughter’s stomach, but in her head.
But she is not tired, she is ready to continue doing this. Enlighten. Inspire. Inform.
“Why am I writing about my daughter and her successes? Sometimes you really want to climb deeper into the den and not let anyone in there. But I see how these posts inspire those parents who are just faced with this diagnosis. They see Alenka on a horse, at a reading competition, at a meeting with producer Maxim Fadeev - and believe in the best.
One day, Alenka, my eldest daughter Nastya, and I went on a horseback riding trip. I was nervous about my eldest and kept shouting to her: “Nastya, hold on! Nastya, hold on!”
Finally, the instructor couldn’t stand it and said: “Yes, she’s holding up better than anyone else,” and points to Alenka. I laugh: “Yes, I know, I’m shouting to the eldest.”
Alenka is confident both in the saddle and on stage. Not a single performance at school goes on without her. Even when she couldn’t walk yet, she played... Kolobok!
What she hasn’t been able to do yet is seriously take up music (we are often in hospitals, it’s difficult to organize a regular schedule of classes) and dancing (dances for wheelchair users are not suitable for her - she has already left the wheelchair, and the usual ones are not yet possible).”
But, looking at Alenka and her mother, we can confidently say: “This is not working out YET!” Once upon a time, doctors, looking at shunt-dependent Alena, only said: “Sit near the intensive care unit and don’t rock the boat!”
And only Dmitry Yuryevich Zinenko (now the head of the neurosurgical department of the Yu.E. Veltishchev Research Institute of Pediatrics) said: “You can do anything! Either fly into space or go diving.”
“It is no coincidence that all of us, his patients, are jokingly called “Zinen addicts.” He gave us a chance for an ordinary life.
Alenka, for example, does not allow me to stick a disabled sign on my car. And there are children with hydrocephalus who were not registered as disabled at all. They just live like everyone else. Of course, it is impossible to completely relax and not think about the shunt. In any state, I control it with at least the edge of my consciousness.
Didn't you fall? Did you hurt yourself? Doesn't she feel sick? If you feel sick, go straight to the ambulance and the hospital. If a child with a shunt vomits, the first thing we do is rule out problems with the shunt. Everything else is poisoning, infection - later. And yet I try not to get hung up on thoughts about the shunt, but just live. So, I think Alenka should still try to take up music: she has perfect pitch.”
Participation in care
Children with implanted shunts should be monitored by a neurosurgeon throughout their lives. Most patients suffering from hydrocephalus, after implantation of a shunt system, can lead a normal life, but constant monitoring by loved ones in collaboration with a neurosurgeon is necessary.
The neurosurgeon monitors each patient to prevent drainage failure. The first time after implantation or re-operation - regularly, with a gradual transition to examinations once a year.
Relatives are advised to be able to recognize early signs of complications. Quick and accurate assessment of health problems is very important. Flu symptoms may mask symptoms of a blocked shunt. Quickly identifying them will allow you to plan a repeat operation and avoid an emergency.
Patients and their loved ones should pay close attention to signs and symptoms of complications. The main causes are: blockage, infection and excessive drainage.
Varenka: the suffering was associated with the shunt
– Even as a child, I knew that I would have a son, Stepka, and a daughter, Varenka. But somehow it didn’t work out,” says Elena Kirina from the city of Sortavala (Karelia). My husband and I did not have children for seven years. They were examined and treated. Finally they told me that I was pregnant and had twins, I fell to the floor with joy and began to cry. And then at 14 weeks, on an ultrasound, it became clear that Varyusha has Dandy-Walker syndrome, the cerebellum is not developing and she most likely will not survive, and if she survives, she will become disabled. They offered us an abortion, but Styopka could have been harmed during the abortion. And in general, I have always been against abortion. We decided to give birth. I cried for the rest of the pregnancy. At 33 weeks labor began. They performed a caesarean section. I didn’t see Varya at all - she wasn’t breathing, they immediately took her away.
On the 9th day, Varya began to develop hydrocephalus. At three months she had her first shunt installed. But the girl suffered. In total, she underwent eight surgeries. Her shunt was clogged and her cerebrospinal fluid was infected. In essence, she was doomed. She spent a whole year in hospitals in Petrozavodsk and St. Petersburg. And Lena, who could not leave Stepan for long (he also had health problems), spent more time on the road this year than with her daughter.
“I had a small child at home, and I cried endlessly and wanted to strangle myself. Because my other child was dying alone in the hospital.
The problem was that Varya was kept in the infectious diseases department, believing that her symptoms were a consequence of the virus. And her suffering was associated precisely with the shunt.
Blockage
The main type of complication is blockage of the system. Blockages can occur at any level of drainage. The holes in the ventricular catheter may become clogged with brain tissue or villous plexus tissue. It can also be blocked due to excessive contraction of the ventricular cavity due to too intense drainage of fluid from the ventricular cavity (constricted ventricle syndrome). Intestinal loops or necrotic tissue may adhere to the peritoneal catheter. Shunts inserted into a ventricle of the heart can become blocked by blood clots, pieces of brain matter, or tumor cells.
The shunt system may also be disconnected by disconnection of various elements of the shunt or by changes in the position of the catheter caused by the growth of the child. X-rays are necessary to check the integrity of the shunt.
Partial blockage of the system parts provokes the appearance of symptoms of increased intracranial pressure. Episodic headaches, nausea, apathy and decreased sensory functions may occur. Decreased performance at school or at work is the most common phenomenon in these conditions.
In case of complete blockage, symptoms develop more quickly (headaches, nausea, vomiting, blurred vision, loss of coordination and confusion). The patient falls into a stupor or coma. In such cases, urgent hospitalization is necessary for observation and appropriate treatment.
The surgeon performs a series of tests to locate and determine the extent of drainage blockage. Sometimes it is necessary to remove and replace part or all of the system.
Dmitry Zinenko: hydrocephalus is a mysterious disease
– Hydrocephalus is the most mysterious disease of the central nervous system, which still does not have a generally accepted definition. But, despite this, we have learned to cure hydrocephalus,” says Dmitry Yuryevich Zinenko, head of the department of neurosurgery at the Research Institute of Pediatrics. – If you treat it on time and adequately, then it goes away without consequences for the child.
– Can I play sports?
– Children live full lives. True, it must be said that the cause of hydrocephalus can be: hypoxia, hemorrhage, trauma, infection and other diseases that are accompanied by brain damage, which determines the severity of the child’s condition, and not hydrocephalus as such. But it is hydrocephalus that can be recognized in a timely manner and adequately treated.
– Can specialists “overlook” it?
– Hydrocele of the brain is most often diagnosed in children under one year of age. It always occurs with increased intracranial pressure, which has clear manifestations: a rapid increase in head circumference, swollen veins on the head, and a swollen fontanel. A bright picture, impossible not to notice. If we talk about diagnostics, then more often we are dealing with overdiagnosis.
In 90% of cases, the diagnosis of “hydrocephalus” is made where it does not exist.
But when the patient has a shunt installed, then other problems appear. More often we encounter, on the contrary, an underestimation of the severity of the child’s condition. The pressure becomes low, not high. And this further hinders the child’s development.
Sometimes you have to deal with the following opinion: they installed a shunt, the ventricles got smaller – and that’s good. And if the child still cannot stand upright, this is perceived as a natural manifestation of the disease itself.
But in fact, if the ventricles have become smaller, this is a disaster. The head has stopped growing - this is a disaster. A child cannot stay upright for a long time - this is a disaster. These are all signs that the shunt is working too well. It is necessary to change the shunt and reduce the outflow of fluid. To save money, shunts are generally installed, which do not meet all the needs of the body.
- Poor quality?
– How can I tell you... You can buy a Zhiguli. Good car. But she has her limits. Or you can buy a Mercedes. It has more opportunities and higher security. But the price is different. That's how it is with shunts. Unfortunately, fixed pressure shunts are such “Zhiguli”. They are available, but lead to a huge number of complications. It's like a faucet that is always open to the same flow of liquid, which may not be suitable for a particular child.
You need to immediately install a programmable shunt. Then we can regulate the outflow of fluid for each child individually without repeated operations. They are expensive, but in the long run they avoid many complications and would be cheaper overall for the health care system. And most importantly, it’s safer for the child.
– You operated on little Matvey together with the famous Indian surgeon Sandeep Vaishya, when you reduced the volume of his head, a consequence of hydrocephalus. Was this a unique experience for you?
– Of course, any exchange of experience is priceless. We also perform such operations, but it was useful to work with an excellent surgeon, see his technique, and discuss approaches. This operation is exclusive today only because such large heads have become rare these days. Hydrocephalus can be successfully treated in the early stages. You don't have to wait until your head gets that big.
Birthday head: volunteer surgeons treat orphans with hydrocephalus
Infection
Infection is the second type of complication. It poses a significant risk for any surgical procedure, most often when implanting a foreign body.
It manifests itself in the form of redness or suppuration along the edges of the suture or along the path of the drainage system under the skin. The surgeon fixes his attention on these signs. If left untreated, the wound may erode or open, and in more serious cases, the infection may cause chills and fever. Typically, the drain needs to be removed. Sometimes antibiotic therapy can be administered without removing the system.
Since the shunt is a foreign body, the patient may experience an allergic or inflammatory reaction. Inflammation at one of the drainage sites should be immediately shown to a neurosurgeon.
Excessive drainage
Excessive drainage of cerebrospinal fluid occurs when the valve is incorrectly selected according to the pressure parameter. If the valve opening pressure is too low, it can cause excessive drainage, causing the cerebral ventricle to compress and deforming the brain tissue. The patient experiences headaches that are most severe when standing.
In addition, nausea, vomiting, drowsiness and nervous system disorders, in particular double vision, appear. School-age children experience a decline in mental abilities.
Features of rehabilitation
When the procedure is completed and the shunt is in the head, the patient will begin to feel unwell. It is often accompanied by mild nausea, dizziness, headaches of varying intensity, and mild numbness of the limbs. All these sensations can be expressed with different strengths. This is the norm.
On the second day after the operation, the doctor should assess the success of the bypass. To do this, the patient needs to undergo an MRI, which will help check the condition of the brain and eliminate the likelihood of complications developing after the intervention. If everything is in order, then repeated examinations are carried out another week and immediately upon discharge from the hospital. The total recovery time in hospital is 14 days.
The person will look normal after the shunt is installed, because... all its components are practically invisible.
Rehabilitation process
After discharge from the hospital, a person must lead a special lifestyle that will allow his body to recover as correctly as possible after the surgery. The installation of the shunt itself requires special attention, because... many factors can have a negative impact on a person’s future condition and cause complications.
The person recovering is required to follow simple rules:
- Complete cessation of alcohol and cigarettes until the body is completely restored.
- Avoid any physical activity. A complete ban on lifting heavy objects and all kinds of household or country work.
- Refusal to drive a car and all types of work that require concentration. There is a risk of an inadequate reaction to stressful situations, which will also lead to complications.
- Home regime for 30 days. At the same time, it is prohibited to visit swimming pools and ponds, or to stay outside for longer than necessary, especially if the weather conditions seem unfavorable.
- No touching of the head in the area of the postoperative opening. Any contact with this area can cause injury and rapid infection. It is also prohibited to try to remove the shunt yourself.
- Take all prescribed medications according to the doctor's instructions. The patient is prescribed anticonvulsants. At the same time, it is important to monitor your well-being, because... they have a number of side effects.
Throughout the entire rehabilitation period, it is very important to strictly follow the instructions of your doctor. This is the only way to avoid problems in the future and return to normal life as quickly as possible. The patient will live a full life for a very long time with virtually no restrictions. The life expectancy of those who had to undergo shunting is practically no different from the average statistical indicators of healthy people.
It is very important to work on yourself, setting yourself up psychologically for a quick recovery. Rehabilitation without this will be less successful.
The need to replace the shunt
The need for a shunt remains forever. Therefore, a shunt patient should take his problem as seriously as possible. This is not as convenient as most patients would like, but the result with the ability to live peacefully is much more important.
From time to time the shunt needs to be changed. Gradually it loses its effectiveness. The reason for this is blockage, wear, and various accidental damage. It is impossible to say how long the shunt will last. They are designed for a service life of up to 10 years. However, they often have to be replaced much earlier, regardless of quality. Especially when it comes to children. Along with their gradual growth, lengthening and a shunt will be required. Replacement is very quick and painless.
If you first need to check the equipment or replace it, you should immediately contact your doctor, because specialist intervention will be necessary. It can only be removed by an experienced employee of a medical institution.
Is the patient considered disabled?
Patients who have undergone brain shunt surgery can expect to be assigned a degree of disability. This is determined by a commission that makes a decision based on the research conducted. Both a child and an adult can be recognized as disabled if they are identified as having impairments in the main categories of life activity, which include the following abilities:
- self-service;
- orientation in space;
- movement;
- education;
- self-control;
- communication;
- work activity.
Disability will need to be continually confirmed through examinations.
More information about shunt systems for the treatment of hydrocephalus
The result of the operation largely depends on the quality of the shunt system. In recent years, in many hospitals, neurosurgeons have been using shunt systems produced by the largest American company Medtronic. The company's engineers, together with leading US neurosurgeons, have developed a range of valves of various models and sizes (including valves for newborns).
One of the latest achievements in the production of liquor drainage devices is the Delta valve. This is a unique valve, has no analogues from other manufacturers. It was created to avoid such a common complication as excessive CSF drainage. If all other valves pass as much fluid as they are designed for pressure, then the Delta valve allows as much fluid as is needed to remain in the ventricle to maintain intracranial pressure within physiological limits. When implanting the Delta valve, the patient is maintained at normal pressure, regardless of the rate of cerebrospinal fluid production and, most importantly, regardless of the patient’s body position (lying/standing).
The technological features of the materials from which the system valves are made prevent deformation and sticking during pumping; the dome of the valve reservoir is designed to withstand repeated punctures with a thin needle (the holes self-tighten). Catheters are made of high-quality latex-free silicone, so they do not stick together or form loops, which significantly reduces the risk of system blockage.
The valves are equipped with connectors for connection to catheters; their design facilitates connection and reduces the possibility of disconnection and disconnection of the system.
A radiopaque mark is applied along the length of the catheters, this allows you to see the shunt on an x-ray. The same substance is applied to the valve with a dot code indicating the pressure of the valve. There are no metal parts in the shunt system. This is very important when conducting CT and NMR studies, because metal will produce artifacts, and a magnet in NMR may shift the location of the system (if it had metal parts).
All systems are sterile and supplied in double sterile packaging. To reduce the risk of infection, Medtronic has developed a unique BioGlide hydrogel. It is applied to the inner and outer surfaces of catheters, as well as the outer surface of the valve, and does not peel off. Before implantation, the neurosurgeon can treat the system parts with antibiotics, and the hydrogel will hold them for 3 days for postoperative antibiotic therapy inside the patient’s body. This way, the risk of infection is minimized.
Matvey: waiting for his mother
Matvey's head grew so large from hydrocephalus that until he was three years old he could not even lift it. No, not by oversight. Yes, the young 17-year-old mother abandoned him immediately after giving birth. But the caring hands of Elena Evgenievna Shatskaya, the head physician of that institution for orphans in the Ryazan region, who accepted Matvey, and her colleagues did everything possible for him. And even the impossible. Bypass surgery, shunt testing, replacement. Everything was complicated by a congenital brain defect.
When the capabilities of regional neurosurgeons were exhausted, Elena Evgenievna reached the federal ones. And now a unique operation to reduce the head (cranioplasty) of three-year-old Matvey was performed in two stages by the best Russian neurosurgeons together with the invited Indian surgeon Sandeep Vaisha.
After the first operation, the baby turned over on his stomach, and after the second, he began to get up on all fours and raise his head.
Today, 4-year-old Matvey can sit down on his own and remain in a sitting position for quite a long time. This means that now he eats and walks while sitting. His diet has expanded (it turns out he loves bananas and strawberry curds), his visibility has increased, and new emotions have appeared.
– Even such a difficult combination of diagnoses is not a reason to “give up” on a child. We cannot guarantee him the ordinary life of an ordinary baby, but we can improve the quality of his life, give him a chance, and use the rehabilitation potential that he has. I don’t know if he will study in a regular school, but there is hope that he will go!
Our most important worry is that in a year we are obliged to transfer our smiling boy to a boarding school for children with severe mental retardation. But if only he had a family! We would be very happy to provide them with all our rehabilitation opportunities,” Elena Evgenievna dreams. “I’m sure he will make someone’s parental happiness!”
Emotional support
The physical side of hydrocephalus is only part of the problem of this disease. The patient and his relatives need to take into account his emotional factors.
Although surgery should resolve your hydrocephalus to some extent, you may feel fearful, depressed, irritable, or doubtful. If the patient is a child, it should be taken into account that he has the same feelings as an adult. If your child is feeling out of shape or uncomfortable because they need to visit the doctor frequently or have repeated tests, it is best to reassure them with simple explanations. If he knows what awaits him, he will be more willing to cooperate with you. Children, like adults, as a rule, do not like unpleasant surprises. A calm atmosphere among loving loved ones is the best environment for children. It is advisable to explain the phenomenon of hydrocephalus in words that the child can understand.
It is very important to know how the child feels and be able to explain to him what he is experiencing. The needles hurt. It is natural to cry and want to get rid of them. Being admitted to hospital is a new challenge for your child. You must tell him the truth in order to gain and secure his trust. Sincerity is the best way to maintain your child's trust.
Children over ten years of age are generally able to comprehend more complex concepts. They may associate signs and symptoms with their illness. Restrictions associated with the disease are easier for them to bear. Tell your doctor about your feelings and give him the right to guide you. Some people share their feelings with close friends, others need professional help. The health professionals treating you or your child are interested in your well-being and their goal is to do what is best for you and your loved ones.
Patients and the patient's parents should communicate with their doctor quite frequently. It is important to actively participate in this communication so that your doctor can better understand your needs and the needs of your loved ones.
Alenka. Reset stigmas
Svetlana Lisunova, an activist of the MBOO helping children with neurosurgical diseases “He needs you”, Alenka’s mother with post-hemorrhagic occlusive hydrocephalus, says:
“I stood under the door of the intensive care unit and only heard: “This is already a corpse. Why are you clinging to her”, “Imagine that it’s an abortion”, “It’s better to cry once now than to cry all your life later”
Difficult birth. Brain hemorrhage. They immediately said about their daughter: “she won’t survive.” And that’s probably why they didn’t do much about it. She lay in intensive care for 12 hours without artificial ventilation. She just lay there and gasped.
“Sick leave? If he dies, come and get sick leave.” They weren’t allowed to baptize: “There’s no point in shaking dirty robes here.” They didn’t take expressed milk: “We don’t need your goat urine here.”
At three months, Alenka, without waiting for her death, was nevertheless discharged home. Within a week, Svetlana realized that hydrocephalus was growing. Alenka cried sharply, burped heavily, her eyes literally popped out of her head - she was probably tormented by severe headaches. The accumulating cerebrospinal fluid began to put pressure on the brain.
Svetlana is a doctor by training. She could recognize hydrocephalus. What's next? Of course, she, an orthopedist by specialty, took a course in neurosurgery in a very truncated form. But what exactly? I got out the textbooks. “A condition incompatible with life... die in the first days of life... parents suffering from drug and alcohol addiction...”
Svetlana devoted the next ten years of her life to refute each of these lines of that rotten textbook. Reset stigmas.
Today she is an activist in the public organization “He Needs You.” And her Alenka is a 10-year-old beauty and an excellent student. Her friends, wards, colleagues - hundreds of parents of children with hydrocephalus.
There is not a single person with addictions among them. The vast majority of cases of hydrocephalus she encounters are rooted in birth injuries and cerebral hemorrhages. A small percentage of children received congenital hydrocephalus (usually it is also associated with intrauterine injuries - accidents, etc.). And a small percentage of hydrocephalus is associated with infections suffered by the mother during pregnancy.