Acute lymphoblastic leukemia
More than 80% of all leukemias in children are acute lymphoblastic leukemia (ALL). The reason for its development is the chimeric TEL/AML gene, the formation of which occurs in utero, possibly as a result of spontaneous errors in the process of DNA replication and repair. The accumulation of genetic abnormalities in the tumor clone leads to a block of normal cell differentiation and disturbances in the process of proliferation and apoptosis.
In accordance with the French-American-British (FAB) classification, three morphological variants are distinguished: L1, L2, L3.
Clinical symptoms of ALL are determined by the degree of bone marrow infiltration by lymphoblasts, as well as the presence of extramedullary spread of the process. General symptoms of tumor intoxication are often observed, namely, increased body temperature, decreased appetite, weakness, and lethargy. During the process, several periods are distinguished: initial, extended, and remission.
The full-blown period is characterized by a rapid onset and a variety of clinical symptoms. Symptoms of general intoxication include bone pain due to leukemic infiltration of bone tissue (the diaphyses of long tubular bones are most often affected), and arthralgia caused by leukemic infiltration of joints. The skin and mucous membranes become pale. Unfortunately, they often develop hemorrhages caused by hemorrhagic syndrome, as well as bleeding (nasal, gastrointestinal, renal). Enlargement of peripheral lymph nodes (cervical-supraclavicular, axillary, inguinal) is one of the main symptoms of the disease. Almost all patients experience enlargement of the liver and spleen due to the proliferation of leukemia cells. In some cases, in patients, damage to the skin and mucous membranes manifests itself in the form of leukemides, necrosis, gingivitis and stomatitis.
Thus, several symptom complexes characteristic of ALL can be identified:
- hyperplastic – lymphadenopathy, bone pain, heaviness and pain in the left and right hypochondrium, hepatosplenomegaly;
- anemic - dizziness, flickering spots before the eyes, shortness of breath during exercise, palpitations, noise in the head and ears;
- hemorrhagic – skin hemorrhages, bleeding gums, nosebleeds;
- intoxication – increased body temperature, weakness, lack of appetite, ossalgia;
- syndrome of infectious complications - the addition of severe pneumonia.
During diagnosis, the morphological features of bone marrow and peripheral blood blasts are assessed. In addition to detecting tumor cells of the lymphoid line of hematopoiesis using Romanovsky-Giemsa staining, the following research methods are carried out:
- cytochemical - allow blasts to be classified as lymphoid or myeloid lineages (test for myeloperoxidase, phospholipids, glycogen), individual cell lines;
- immunophenotypic – determine immune cell markers (CD);
- cytogenetic – determine karyotype anomalies and chromosomal aberrations (deletions, translocations, inversions, etc.);
- molecular biological – allow you to determine the number of cells with a certain aberration in the entire mass of the bone marrow.
To confirm the diagnosis of ALL, a comprehensive examination is necessary, in which the leading role is given to the morphological method.
Currently, the treatment programs BFM (BFM: Berlin-Frankfurt-Münster) and CF (MB: Moscow-Berlin) are used.
All treatment can be divided into basic and accompanying. Basic therapy consists of systemic and local chemotherapy and, if necessary, radiation therapy. Accompanying treatment is necessarily prescribed to prevent infectious complications and correct post-cytostatic reactions. The following stages are distinguished in the treatment of malignant processes: induction of remission, consolidation of remission (usually several phases), maintenance treatment.
2. Causes of leukemia
The exact causes of leukemia are still not known. But certain things have been found to increase the risk of developing certain types of leukemia. Risk factors are:
- Exposure to large amounts of radiation;
- Exposure to certain chemicals (eg at work), such as benzene;
- Having undergone some types of chemotherapy to treat other types of cancer;
- Down syndrome and other genetic problems;
- Smoking.
However, these risk factors are quite arbitrary. Most people who are at potential risk do not get leukemia. And most people who have leukemia are not at risk for any known factor.
Visit our Oncology page
Acute myeloid leukemia
Acute myeloid leukemia accounts for 15% of all acute leukemias in children. The existing FAB classification (French-American-British) allows you to divide AML into the following options:
- M0 (minimally differentiated AML), which is characterized by medium-sized blast cells with a round nucleus, absence of granulation and Auer rods in the cytoplasm;
- M1 (AML without maturation), in which less than 90% of non-erythroid cells are blast cells with a predominant mesogeneration with round nuclei and a high nuclear-cytoplasmic ratio;
- M2 (AML with maturation), characterized by medium-sized blast cells with a high and moderate nuclear-cytoplasmic ratio (20 - 90% of all non-erythroid cells), in their cytoplasm the presence of azurophilic granules and Auer rods is expressed;
- M2 bases (basal cell), blast cells are characterized by the presence of basophilic granularity, makes up no more than 0.5% of acute non-lymphoblastic leukemia;
- M3 (promyelocytic) variant is characterized by large blast cells with irregularly shaped nuclei, coarse granulation and Auer rods in the cytoplasm;
- M3v (hypogranular) with no granularity;
- M4 (myelomonoblastic): blast cells with round and irregular nuclei, low to moderate nuclear-cytoplasmic ratio, some blast cells may contain granularity, Auer rods;
- M5a (monoblast without maturation), in which monoblasts make up over 80% of monocytoid cells, large-sized blast cells with bean-shaped or lobed nuclei, some of them show granularity, Auer rods are not detected;
- M5b (monoblastic with maturation): monoblasts make up less than 80% of monocytoid cells, large with monocytoid-shaped nuclei, cytoplasm without granulation, Auer rods are not detected;
- M6 (erythromyelosis): more than 50% of blastomas in the bone marrow are represented by erythroblasts;
- M7 (megakaryoblastic) leukemia, in which the blast cells are polymorphic, with branched basophilic cytoplasm, and there are no specific morphocytochemical signs.
Scheme of hematopoiesis with precursor cells of acute myeloid leukemia
The clinical picture of AML also consists of anemic, hemorrhagic and toxic syndromes, which are a consequence of decreased production of red blood cells, platelets and granulocytes.
In 50% of patients, there is an increase in the size of the liver (hepatomegaly) and spleen (splenomegaly) due to infiltration of organs by tumor cells.
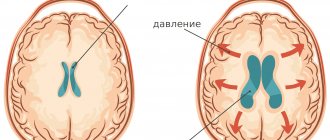
Extramarrow manifestations of the disease are associated with leukemic infiltration of the central nervous system and metastatic damage to the membranes and substance of the brain and spinal cord (neuroleukemia). In these situations, there is a constant headache, vomiting, lethargy are possible, swelling of the optic discs is detected, there may be nystagmus, strabismus, and other signs of damage to the cranial nerves, stiff neck muscles, and Kernig's sign are detected.
Cytochemical, immunophenotypic and morphological examination of blasts in the bone marrow and peripheral blood also plays a decisive role in diagnosis.
Remission of the disease can be achieved through high-dose polychemotherapy followed by transplantation of hematopoietic stem cells from an HLA-genoidentical related or alternative (unrelated, haploidentical) donor in patients at high risk of relapse. Thanks to adaptive protocols, it is possible to achieve remission in 90% of children.
Symptoms
The course of different types of disease is not accompanied by specific symptoms of leukemia. On the contrary, its manifestations are the same for all types of pathology and are poorly diagnosed in the initial stages. These include:
- increased susceptibility to colds and seasonal ailments;
- night sweats;
- joint and bone pain;
- swelling of the lymph nodes;
- instability of body temperature, constant sharp changes;
- pallor, grayish skin tone;
- general malaise, weakness;
- long-term healing of even minor injuries;
- causeless loss of body weight.
In the later stages of the disease, more distinct signs of leukemia appear:
- characteristic yellowness of the skin and eye whites;
- deterioration of vision, up to complete dysfunction;
- severe headaches;
- difficulty breathing, pneumonia;
- frequent nausea, vomiting;
- problems with cardiac activity;
- numbness of the facial muscles, partial or complete.
In later stages, due to increased fragility of blood vessels, subcutaneous and internal hemorrhages often develop. Ulcerative-necrotic tissue lesions and severe tonsillitis may appear.
Chronic myeloid leukemia
Chronic leukemia is a variant of hemoblastosis, the substrate of which is maturing cells. In children, only chronic myeloid leukemia occurs, which is characterized by proliferation of granulocytic lineage, hyperplasia of myeloid tissue, myeloid metaplasia of hematopoietic organs, associated with chromosomal translocation t(9;22)(q34;q11), which results in the formation of the chimeric oncogene BCR-ABL.
During chronic myeloid leukemia there are three phases:
- Chronic phase: no significant symptoms.
- Acceleration phase: increased levels of leukocytes (>50 x 109/l), blasts in peripheral blood and bone marrow (>10%); anemia and thrombocytopenia; persistent thrombocytosis (> 1000 x 109/l).
- Acute (blastic) phase: myeloblasts >30% in the blood or bone marrow; lymphoblasts >30% in blood or bone marrow; the presence of blast cells in the cerebrospinal fluid.
At its onset, the disease is difficult to diagnose, since the main symptoms are caused by the general tumor symptom complex and are transient. The most common symptoms that appear later are hepatomegaly and splenomegaly. Increasing intoxication leads to weakness, fatigue, increased body temperature, and bone pain.
In the peripheral blood, hyperleukocytosis is observed (up to 200 - 300 x 109/l or more) with an increase in the content of granulocytes up to 95% and a predominance of immature cells of the granulocytic series: promyelocytes, myelocytes, metamyelocytes, myeloblasts, basophils (up to 10%) and eosinophils (up to 5 %). Characterized by anemia and increased ESR. The platelet level is mostly normal, but hyperthrombocytosis may be observed (up to 600 x 109/L or more).
In bone marrow puncture, an increase in the number of myelokaryocytes is noted due to the proliferating pool of granulocyte cells with an increase in basophils and eosinophils. Later, inhibition of erythronormoblastic and megakaryocytic hematopoietic lineages is noted.
The mainstay of therapy and standard treatment for chronic myeloid leukemia is currently the use of tyrosine kinase inhibitors (TKIs). These drugs have a mechanism of targeted action on BCR-ABL-positive tumor cells and should be prescribed to all patients after confirmation of the diagnosis. To assess the effectiveness and tolerability of TKI therapy, regular monitoring of hematological, cytogenetic and molecular genetic and other parameters in the patient is recommended.
Bibliography
- Kuznik B.I. Clinical hematology of childhood: textbook. allowance / B. I. Kuznik, O. G. Maksimova. - M.: University Book, 2010. - 496 p.
- Rumyantsev A. G. Practical guide to childhood diseases. T. 4. Hematology/oncology of childhood / A. G. Rumyantsev, E. V. Samochatova. - M.: Medpraktika-M, 2004. - 792 p.
- Rumyantsev A.G. Evolution of treatment of acute lymphoblastic leukemia in children. Pediatrics, 2016; 95(4): 11-22.
- Möricke A., Zimmermann M., Reiter A., et al. Long-term results of five consecutive trials in childhood acute lymphoblastic leukemia performed by the ALL-BFM study group from 1981 to 2000. Leukemia. 2010 Feb;24(2):265-84. doi: 10.1038/leu.2009.257.
- Creutzig U, van den Heuvel-Eibrink MM, Gibson B, et al. AML Committee of the International BFM Study Group. Diagnosis and management of acute myeloid leukemia in children and adolescents: recommendations from an international expert panel. Blood. 2012 Oct 18;120(16):3187-205. doi: 10.1182/blood-2012-03-362608.
- de la Fuente J, Baruchel A, Biondi A, de Bont E, Dresse MF, Suttorp M, Millot F; International BFM Group (iBFM) Study Group Chronic Myeloid Leukaemia Committee. Managing children with chronic myeloid leukaemia (CML): recommendations for the management of CML in children and young people up to the age of 18 years. Br J Haematol. 2014 Oct;167(1):33-47. doi: 10.1111/bjh.12977.
Types of disease
The modern classification of leukemia includes several principles of division into types. First of all, it is worth mentioning the division of cases of the disease according to the nature of the course into:
- acute, characterized by rapid development and the formation of a large number of immature blood cells - blasts;
- chronic, which are characterized by a long course and pathological production of mature leukocytes with altered properties.
Another principle for classifying leukemia is based on the level of differentiation of the affected cells, which can be:
- undifferentiated;
- quotational;
- blast.
In addition, oncologists distinguish many types of leukemia according to the types of cells whose pathological changes underlie the disease. According to this principle, lymphoblastic, monoblastic, myeloblastic, lymphocytic, myeloma and other types of disease are distinguished.
Forecasts
The success of leukemia treatment depends on many factors, but in most cases the prognosis is favorable. Acute forms are more complex, since the rapid course of the disease leaves less time for the doctor to act. In the chronic form, favorable outcomes, according to statistics, account for up to 85% of cases.
In any case, there remains a chance for a long-term remission and complete relief from the disease. In adults, the probability of a positive outcome is at least 40%, in children - up to 90%.