What is donation
Even our normal daily lives are fraught with danger, not to mention police officers, firefighters, airplane pilots and other professionals whose work is inherently fraught with risks.
No one can guarantee you that today's trip to work will not end in an accident. And then a blood transfusion may be needed. This procedure can save the patient’s life during operations, bleeding, burns, severe injuries, childbirth, anemia, hemophilia, cancer, liver diseases, etc.
It is blood and its components that are important components in the salvation of a person. And they can only be obtained from a living donor - one who voluntarily gives his blood to another.
Despite all the efforts of scientists, at the moment, unfortunately, it is impossible to replace donor blood with artificial one. It exists and even has its advantages, but the disadvantages of artificial blood do not allow its use. Disadvantages include toxicity, too high production costs, and the lack of multifaceted therapeutic effects on the body.
That is why the world so needs to support donation - the voluntary donation of blood and its components in medical institutions for further transfusion to patients in need.
Today there is a shortage of donor blood. And although there is a myth that only a rare group is needed - the fourth, in fact, each is equally important. Yes, there are more donors from the first, second and third groups, but they are needed more often. And if blood is rare, then there are fewer patients who need it.
More than 100 cool lessons, tests and exercises for brain development
Start developing
The first place among the necessary groups is occupied by the second, since it is the most common, which means there is a high probability that there will be a need to use it.
Judging by the AB0 system, which is the most popular, there are 4 blood groups in total: group I - 0, group II - A, group III - B, group IV - AB. Also no less important is the Rh factor, which can be positive or negative.
Chief Physician of the O.K. Blood Center Gavrilova DZM Olga Andreevna Mayorova - about how the capital’s blood service is organized, which blood components are most in demand and how a novice donor can organize the process with maximum comfort for themselves and benefit for the city.
Is there enough donor blood in Moscow now?
Fortunately, there is no shortage of blood and its components in the city. Difficulties can only arise with the selection of blood for patients with rare phenotypes and antibodies - but we are also solving this problem to the best of our ability by creating special reserves. The selection of blood components for recipients is carried out according to at least ten, and more often according to twenty to thirty different indicators. This is a rather complex and time-consuming process; sometimes it is difficult to choose the right material.
Perhaps for such complex patients it is possible to find a donor among relatives?
In fact, there are strict contraindications against the use of related donor blood. In some cases, patients may experience immunological reactions, especially with hematological diseases. We always try to find a non-relative donor for such patients. But we are happy to invite relatives, if they are ready for this, to make a reciprocal donation: someone helped you, and you help others. This is nothing more than a form of conscious gratitude.
Indeed, in Moscow there are several very difficult patients, whose names we know from memory: they need special, rare blood. As a rule, for them we keep a special supply of donor blood with a special mark: this saves us from the need in an acute moment to search for donors in the database and call them, asking them to urgently donate blood components.
What type of blood is usually missing?
There is an increased need for Rh negative blood components in the city: the number of Rh negative donors is decreasing from year to year. Why is this happening? Migration factors may have an influence: it is known that negative Rhesus is extremely rare among representatives of Asian peoples. We also note that recently even young donors are beginning to experience health problems earlier, and among our donors citizens over 40 years of age predominate. So, finding a healthy donor is becoming increasingly difficult.
In what seasons is donated blood most needed?
As a rule, the risk of a shortage of blood and its components in Moscow occurs during the New Year holidays, as well as in the summer. The reason here is not at all that the number of acute injuries is becoming more frequent: donors are simply leaving the city. We have learned to cope with the New Year holidays: we create blood reserves in advance. In addition, we continue to work on holidays: for the whole country the New Year holidays last 10 days, but for us it lasts no more than 5 days. With the summer holidays, the situation is more complicated: they are longer, and the volume of donor activity decreases significantly. In small towns it is quite possible to stock up on blood and its components in advance, but on the scale of Moscow, with its enormous needs, this is almost impossible. In addition, some blood components have a short shelf life - for example, platelets cannot be frozen and are stored for no longer than 5 days. It is impossible to make a full stock.
Which blood components can be preserved for a longer period – and in what way?
Each blood component has its own storage mode. Platelets , as I already said, are very vulnerable and difficult to freeze. They are stored at a temperature of 20-25 degrees, subject to continuous stirring - for this purpose special devices, thrombomixers with a thermostat are used. Fortunately, our service is well equipped with these devices. Red blood cells are stored at a temperature of +4 degrees - that is, under the conditions of a conventional pharmaceutical refrigerator. Shelf life - from 35 to 52 days, on average 42 days. They are frozen effectively: our center and several blood transfusion departments have the necessary supply of cryopreserved red blood cells. As for leukocytes , the donation of these elements is not our prerogative. This is an extremely labor-intensive process, which in Moscow is carried out by only one organization - the National Medical Research Center for Pediatric Hematology, Oncology and Immunology named after. D. Rogacheva. The lifespan of leukocytes is only a few hours, they are used mainly for severe forms of fungal sepsis, moreover, the donation process requires serious preparation, and, as a rule, they are donated only by career donors.
In our service, the most difficult component of blood to obtain is plasma . It freezes well, and its frozen shelf life is 3 years, however, unlike red blood cells and platelets, it cannot be immediately issued to city hospitals. To use plasma, the donor must be re-examined 6 months after donation. This is called quarantine: until we are sure that the donor is healthy, we do not have the right to transfer plasma to medical organizations.
What happens to the collected plasma if the donor for some reason does not show up for additional examination after quarantine?
In such a situation, there is a way to secure the plasma - for this you need to carry out a certain chemical treatment. As a result, we obtain pathogen-inactivated plasma, which can be used for medicinal purposes. However, this process is associated, firstly, with significant financial costs, and secondly, with some losses in plasma properties. It is best if the donor still finds the opportunity to come for the examination. But the components of donor blood, red blood cells and platelets, are sent to the medical network immediately after testing: the tests performed are enough to be sure of the quality of the blood.
What blood components are most in demand now?
In recent years, a general trend has been observed in world medicine: the consumption of red blood cells is increasing, and the consumption of plasma is falling. This is due to new trends in transfusiology, new aspects and technologies for the treatment of hematological and oncological diseases. Thus, now we often have to replace blood cells rather than plasma. There is even an excess of plasma in the city - but, fortunately, the decrease in consumption is offset by a long shelf life. Blood plasma is too valuable a material to be written off: the accumulated surplus will be used to produce medicines.
Can we say that the Moscow blood transfusion station is technically equipped enough to carry out all the tasks assigned to it?
Undoubtedly. Our station is equipped to the highest standard - and what's more, modernization has never stopped for us. We can say that we received the most modern equipment somewhat ahead of the curve, when the request for new methods of donation was at the formation stage. Today we have everything we need to supply the medical network with blood and its components.
We talked about blood components - is whole blood now donated for transfusions?
Currently, whole blood is transfused to patients only in special cases. Although this is not prohibited by law, medicine is already well aware of the risks of developing post-transfusion complications when transfusion of whole blood. Therefore, 99.9% of collected whole blood must be processed and separated into components - this is how we obtain red blood cells.
Are there any differences when donating various blood components? Does the donor feel them?
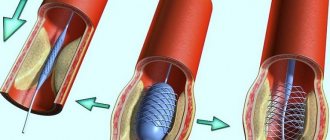
For each component, different sampling algorithms are provided. Donors are most familiar with whole blood donation: many experienced it for the first time centrally, in universities and enterprises. This is the simplest type of donation; it does not require any special devices and can be carried out on-site. Nowadays, blood is donated for red blood cells using this method. But donors donate plasma and platelets using apheresis technologies, only in a hospital setting - either in our blood center or in one of the departments. The process of donating plasma and platelets is much longer: a donor donates whole blood in 10 minutes, plasma in 40 minutes, and platelets in up to an hour and a half.
Who decides which blood components a donor will donate?
The decision is made by the transfusiologist during the reception and examination of the donor. However, every donor has the right to express their wishes and concerns. For example, for some it is very difficult to remain in the same position for an hour and a half - this means that it will be difficult for him to donate platelets. As a rule, experienced personnel donors are inclined towards a certain type of donation: our specialists do not interfere with this. But for the first time, only whole blood is donated. We must see how the donor will cope with blood loss, then find out the donor's infection status, and only then will he be given the opportunity to choose.
The donor's infection status is determined during the donation process - why not in advance?
Previously, it was indeed a common practice to take a blood test from a donor 1-2 days before donation. The danger is that a day or two before donating blood, the donor may be a carrier of an infection: the viral agent is in his blood, but markers of infectious diseases will not show this. Thus, we risk sending potentially contaminated blood to the city. With current practice, we are guaranteed to collect only healthy blood and its components from donors. Yes, some blood will be discarded based on infection tests, but usually this is no more than 1 percent of all cases.
That is, no more than 1 percent of donor blood is rejected?
The presence of infection is not the only reason why blood may be discarded. Other reasons are a lack of protein in the blood, a violation of tightness, deviations in certain biochemical parameters. In total, up to 5% of all donated blood is rejected. In all countries of the world, this figure is approximately the same: science does not yet know a way to significantly reduce the percentage of donor blood that is rejected.
Fortunately, we are often able to detect whether a donor has an infection at the registration stage: then he simply will not be allowed to donate, and the blood will not have to be discarded.
Have medical contraindications for donation changed in recent years? Are there new grounds for medical withdrawal?
All contraindications for donation are regulated by Order of the Ministry of Health of the Russian Federation No. 364 “On approval of the procedure for medical examination of a blood donor and its components.” This order has been around for many years, but it does not need to be changed: our field of activity is quite conservative, and the provisions of the order are formulated quite universally.
Yes, now in global practice there is a tendency to soften contraindications for blood donation. This is quite reasonable: every year it becomes more and more difficult to find absolutely healthy donors. The most severe contraindications still remain severe somatic diseases, a history of cancer, as well as hepatitis, HIV, and syphilis. But neurological diseases, for example, are no longer considered such a strict contraindication: it all depends on the manifestations and severity of the disease. This also applies to other features of the donor’s body. Previously, a strict contraindication was, for example, the presence of piercings or tattoos; We are currently looking for an opportunity to examine the donor and, if no dangerous signs are identified, he will be allowed to donate.
What to do if controversial issues arise during the examination of a potential donor by a transfusiologist?
If during the examination a contradiction is revealed between the information that the donor gives about himself and the opinion of the transfusiologist, the decision on donation will be postponed for a short time, and the potential donor will be given a referral for additional examinations. For example, if a transfusiologist sees a postoperative scar on a donor, he should refer him for a consultation with a surgeon. The surgeon will give his opinion, which will help the transfusiologist make the final decision. Even though this is a rather complex scheme, sometimes completely harmless conditions can pose a threat both to the donor himself and to all blood recipients.
How do donors usually feel when they are refused a donation?
As a rule, our employees are ready to explain to the donor in detail and with reason why such a decision was made in relation to him. Most often, donors agree with our decision. In addition, each such precedent becomes a reason for a detailed self-examination - as a result, a serious illness can be identified.
What happens if the donor test done at your center turns out to be really alarming? Do you inform the donor that you have found something serious in his tests?
Yes, of course, and we report such news only personally – but we definitely report it. That’s why it’s so important that all our donors leave their current contact information in the form!
If a donor's analysis raises concerns, we invite him to our center privately and have a personal, private conversation. The only exception is when we receive a positive HIV test. In this situation, we are obliged to send a blood sample to the MHC AIDS for verification - and, accordingly, the MHC staff will communicate with the donor. There are often cases when we get false positive results. For example, it happens that a female donor has a false positive reaction to syphilis, and this is associated with early pregnancy.
What to do if your tests are positive? Will a person be able to become a donor again after undergoing treatment?
There is a clear algorithm for restoration of donation - if we are not talking about absolute contraindications. Most often, this is a matter of repeating the test after a certain period - and after that you can donate blood again.
Is it true that when donating blood for the first time, a donor cannot receive payment for it?
Yes, that's absolutely right. The first donation – if the person has never been registered as a donor anywhere before – is always free. Further, the donor can follow one of two paths provided by the Moscow healthcare system. The first way is paid donation, regulated by orders and law. To become a paid donor, you need to undergo a fairly extensive examination. As a rule, paid donors are carriers of a rare phenotype or donors with negative Rhesus. Usually the blood of these donors is extremely important, we even personally ask them to come and donate blood from time to time.
The second type of donation is using measures of social support for the population. This process is regulated by Resolution No. 51 of the Moscow Government: starting from the second donation, a donor with any blood type, even the most common, can take advantage of all support measures, receive them in the department where he donated blood - on the day of donation or through a savings system.
Is it true that you feed donors before and after donation?
Before donation, we give each donor sweet tea and cookies. This procedure is not enshrined in law, but it has a long history and is of great importance: its main task is not to feed, but to relax and reassure the donor. After a glass of sweet tea, donating blood is much easier to tolerate. After donation, the donor is indeed supposed to replenish the body’s resources, but we do not feed, we only provide compensation for food. This is much more convenient, since, firstly, each donor has his own tastes and his own diet, and secondly, the given set of food products would be quite cumbersome.
Is it true that sometimes the blood service can refuse to donate to a visiting donor not for medical reasons, but simply because you have such blood in excess?
Cases of such a refusal are quite rare, but, indeed, sometimes it happens that in a given particular department a certain blood group is available in excess. I would advise donors to carefully follow the “traffic light” on the website of our center and the blood service of the FMBA of Russia. Green color means there is a lot of such blood in this department. Yellow – may end soon. Red – this kind of blood is really needed. You can choose a department where your blood will be accepted with open arms.
Is it true that sometimes a donor has to wait in a long line before he can donate blood?
Yes, this happens: our center is also open on weekends, and many Muscovites can only donate blood on weekends. But in fact, only those donors who came to donate on a first-come, first-served basis will have to wait a long time. Those who use the pre-registration system wait much less.
If you are going to donate blood, how much time should you budget for the entire process?
Be prepared for the fact that, taking into account all the formalities, the blood donation process will take at least four hours. Firstly, the donor needs time to fill out a detailed questionnaire, select a measure of social support, undergo an examination, and prepare for donation. Secondly, even if you have always tolerated donation easily, it is worth allowing a little time for unforeseen reactions, mild illness, etc. Donors who donate platelets and plasma are given a medical certificate that will allow them not to come to work on the day of donation.
We know that for many citizens it is important to receive the title of an honorary donor of Moscow, as well as an honorary donor of Russia. Does presentation for an award always take place in a formal atmosphere?
According to the established procedure, the title of honorary donor is actually awarded in a solemn atmosphere. However, here everything depends on the wishes of the donor himself. We are often asked that all formalities be resolved as quickly as possible so that we can receive the certificate in hand and not waste time on the ceremony. There are others - those who require official recognition. For such donors, we will definitely organize a ceremony to award the title. It seems to me that, regardless of the chosen style, the honor of the donor is not diminished in any way: it’s not about who presented you with the award and badge and in what room. It's about how many lives you end up saving.
Types of Blood Donation
In different cases and for different diseases, the patient may need both the blood itself and its components: plasma, red blood cells, platelets and leukocytes. Therefore, there may be a donation of plasma, whole blood or blood cells.
Whole blood is taken in the amount of 450 milliliters. In apheresis, a procedure to remove individual blood components, something specific is taken by separating plasma, platelets, red blood cells, white blood cells or granulocytes from the blood.
The remainder is returned to the donor's bloodstream. Also, saline solution is added to the components returned back, thus helping to normalize the pressure.
More often, doctors need individual components rather than the whole blood itself. Considering that donation is allowed once every 2 weeks, if you donate components 10 to 20 times a year, you can become an honorary donor in 3-6 years. But more on that later.
Plasma donation has its own characteristics. Plasma can be used for up to 3 years after transfusion from a donor. To avoid infection with viruses, it is frozen and stored for six months.
The donor needs to come back to the transfusion station after 4-6 months to get tested and check whether there are any viruses in his blood that did not manifest themselves before donation, but may be in the plasma. If everything is in order during repeated tests, then the plasma can be used.
If the test results are unsatisfactory or if the donor does not come a second time, then the plasma is considered unsafe and is destroyed.
Formally, doctors must notify the donor about the need to re-take tests, and also call him and invite him. But more often they forget about this, so the donor needs to come on his own.
Unlike plasma, red blood cells are stored for no more than a month, platelets can be used for 5 days, and white blood cells can only be used for a day. After the expiration date, all components are disposed of.
Requirements and contraindications for donation
Less than a year ago, a new order of the Ministry of Health came into force, according to which some points regarding absolute and temporary contraindications for donors were changed.
First, let's look at absolute ones. People who have:
- Syphilis, HIV, tuberculosis, hepatitis B and C.
- Blood diseases, stage II–III hypertension and other diseases of the cardiovascular system.
- Psoriasis, eczema, furunculosis and other skin diseases.
- Lack of hearing, speech or vision, as well as myopia greater than minus 6 diopters.
- Mental disorders that are dangerous for the patient himself and the people around him.
- Achilles gastritis, calculous cholecystitis, liver cirrhosis.
- Kidney damage and urolithiasis.
- Bronchial asthma, emphysema.
- Radiation sickness.
- Amputation, organ removal or transplantation.
- Diseases of the nervous system.
- I and II disability groups.
- Oncological diseases.
And now temporary. Citizens who meet one or more of the following points cannot be a donor:
- Age less than 18 years.
- Pulse less than 55 or more than 95 beats per minute.
- Hemoglobin is less than 140 g/l.
- Blood pressure: upper less than 90 and more than 149 mm Hg. Art., lower less than 60 and more than 89 mm Hg. Art.
- Body temperature is above 37 degrees.
- Body mass index is less than 18.5 and more than 40.
- Less than a year ago, an exacerbation of a stomach or duodenal ulcer was relieved.
- Less than 12 months have passed since vaccination against rabies, less than a month against plague, tuberculosis, smallpox, rubella, hepatitis B, COVID-19, less than 10 days against tetanus, diphtheria, whooping cough, cholera, influenza.
- Pregnancy or less than 3 months after lactation.
- Less than 4 months have passed since the operation, including the abortion.
- Medical and cosmetic procedures such as acupuncture, tattooing, piercing, etc. Must be completed over 4 months.
- Less than 4 months ago there was last contact with carriers and patients with HIV, hepatitis B or C, and syphilis.
- The allergic disease lasted for less than 2 months in the acute stage.
- Less than a month has passed since recovery from infectious diseases and acute or chronic inflammatory processes in the acute stage.
- Less than 2 weeks have passed since the last antibiotic intake, and less than 3 days have passed since taking analgesics, anticoagulants and antiplatelet agents.
- The last use of alcohol was less than 2 days ago.
Previously, there were restrictions regarding menstruation and tooth extraction. It was necessary to wait 5 and 10 days respectively. The new law removed clauses about this. There is also no longer any restriction related to the question of up to what age one can be a donor. Therefore, you can come for a donation even at the age of 60, if your health allows it.
It is also often asked whether women who are taking birth control are allowed to donate. And the answer is: yes, you can. But under no circumstances should pregnant women undergo donation.
If you are not completely clear about who can and cannot be a donor, and also doubt whether you are suitable for this, just call the transfusion station in your city. Doctors will answer your questions and help.
In what cases is blood transfusion required?
Transfusion is done due to severe blood loss. If the patient loses about 30% of blood within a few hours, then this procedure should be performed. It is also done urgently if a person is in shock after surgical treatment.
Transfusions are often prescribed to patients who have been diagnosed with anemia, serious blood diseases, inflammatory processes in the body and purulent-septic diseases, strong and severe intoxications of the body.
The procedure is prescribed to people with the following diseases:
- leukopenia – a sharp decrease in the level of leukocytes;
- hypoproteinemia – low level of protein in the blood;
- sepsis – blood infection by microbes;
- violation of ESR.
For transfusion, blood with all its components, drugs and blood substitutes are mixed. Medicines are added to the donor’s normal blood to increase the therapeutic effect, while reducing the risk of complications after the procedure.
Red blood cells are often injected into the patient's body. To do this, the red blood cells are first separated from the frozen plasma. After this, a liquid with a high concentration of red cells is poured into the recipient’s body. This method is used for anemia, acute blood loss, with the development of malignant tumors, after tissue and organ transplantation.
A mass of leukocytes is infused for agranulocytosis, when the level of these cells rapidly decreases, and for the treatment of severe complications of diseases of an infectious nature. After the procedure, the level of white cells in the blood increases, which has a beneficial effect on the course of recovery.
When to use fresh frozen plasma:
- severe blood loss;
- DIC syndrome;
- hemorrhages - blood leaks through damaged vessel walls;
- overdose of coagulants;
- diseases of an infectious nature.
Patients with blood diseases especially need transfusions. Some patients have to do this procedure once a week, or even more often.
Transfusions are also given to people after chemotherapy. If the tumor has affected the bone marrow, after therapy not only malignant cells stop growing, but also healthy ones.
Women often need transfusions after a difficult birth during which they lost a lot of blood. Sometimes doctors do not recommend using a man's blood for this. Women's is considered safer, and for a young mother this is especially important.
Preparing for a transfusion
When preparing to donate blood, you must remember that one day before and on the day of donation, you must exclude fried, fatty and smoked foods from your diet. You can't eat spicy food either. It is also not recommended to consume the following products:
- sausages, frankfurters, sausages and other similar products;
- mayonnaise;
- sunflower and butter;
- drinks that contain coloring substances;
- bananas;
- nuts and seeds;
- avocado;
- chocolate;
- dairy products;
- eggs.
Alcohol should be avoided 2 days before donation.
You should definitely have breakfast: drink sweet tea, you can replace it with compote or fruit drink, eat porridge or pasta with water, vegetables and fruits, in addition to those listed above, an apple is best. From flour, bread, ordinary cookies without additives or crackers are preferable.
You should not come for donation after working the night shift or if you have insomnia. On the contrary, you need to get a good night's sleep. If you feel unwell in the morning, it is better to completely refuse donation that day.
Avoid physical activity at least 24 hours before the procedure. And you should refrain from smoking for an hour.
Blood donation process
To get to most blood transfusion stations, you must make an appointment in advance. Therefore, before coming in person, call and clarify this issue at the reception.
It is easier for the body to adapt to changes and tolerate blood loss in the morning. Therefore, donors, especially beginners, are advised to arrive for the procedure before 12:00. After this time, experienced donors usually come.
The first visit to the blood collection station may take a little longer, as first-timers must fill out several documents.
First of all, you need to register. To do this, you need a passport; men may also be asked to provide a military ID. Foreigners must provide a residence permit or temporary residence permit.
After this, the donor fills out a questionnaire in which he must provide the following information regarding his health:
- general well-being;
- past infectious diseases;
- contact with infectious patients;
- trips abroad;
- use of narcotic and psychotropic substances;
- vaccinations;
- surgical interventions and much more.
Answers must be given honestly, otherwise both the donor and the patient who will receive the transfusion may suffer.
Next comes the turn of clinical and laboratory examination. It consists of:
- examination by a doctor, during which blood pressure, temperature, pulse are measured, the skin is examined, weight and height are measured, and the general well-being of the donor is determined;
- determination of blood type and Rh factor (the procedure is mandatory only for beginners; when donating again, this step is skipped);
- general blood test;
- determination of hemoglobin level;
- detection of HIV, syphilis, hepatitis B and C.
All information provided by donors is confidential. In addition, the results of the examination remain secret from outsiders and can only be obtained by the donor himself.
Before the actual transfusion procedure, the donor is escorted to the dining room, where he is offered sweet tea and cookies. And after this, the blood collection procedure itself begins.
As I already wrote, the total volume of collected blood is about 450 ml. Usually donation does not cause pain, burning or other painful or painful sensations. Although everything is very individual and depends on the sensitivity of the person. Some people may feel slightly dizzy.
But more often the donor feels a small prick and that’s it. According to most people, collecting blood from a vein is not as unpleasant as collecting blood from a finger.
But if illness occurs, it is most likely caused by a decrease in blood pressure due to a decrease in hemoglobin levels. A healthy body easily copes with this and does not experience significant changes in well-being.
The procedure takes place in a special inclined chair. Before inserting a needle into a vein, the skin is disinfected. The blood flows through the tube into the container. Donating whole blood takes no more than 15 minutes, collecting plasma takes about half an hour, and collecting other components can take up to 2 hours.
The beginning of the history of organized donation
The first half of the 20th century is called a heroic era in the development of transfusiology. And, alas, as often happens, one of the engines of progress was the great war, when blood was needed to save the wounded.
The history of regular blood transfusions began with the First World War: for example, the first mobile transfusion station was organized in England. And in 1922, the first blood service was created in London under the auspices of the Red Cross. During the interwar period, donor organizations and blood banks began to emerge in many countries; when it became clear that another big war was around the corner, this process accelerated greatly.
Another important achievement during the First World War was the ability to preserve donor blood. Because blood clots quickly outside the body, transfusions initially could only be done directly, through a syringe, or even by suturing blood vessels. The study of blood clotting and the discovery of the first anticoagulants (substances that prevent clotting) in 1914–1915 led to a real revolution in transfusiology. And direct transfusions began to become a thing of the past.
Gradually, blood transfusions evolved from isolated events into routine procedures. Thus, in 1938, almost 10 thousand transfusions had already been performed in New York; London and Paris were not far behind.
What do we have in our homeland? The first scientifically based transfusion taking into account blood groups was carried out in Soviet Russia back in 1919. And in 1926, the world’s first blood transfusion institute was even created under the leadership of A.A. Bogdanov (later - Hematology Research Center). At that time, very unusual research was carried out there - Bogdanov himself promoted the idea of exchange blood transfusion for the purpose of rejuvenation and binding communists by blood ties (and died during one of his experiments). Another Soviet experience of those times, which seems very strange to us now, was cadaveric blood transfusions. But at the same time, the real foundations of the Blood Service were created in the country, which subsequently saved many lives - from the first blood banks to propaganda and stimulation of donation.
Actions after the procedure
Immediately after donation, you should not make sudden movements. You need to get up carefully, and it’s better to even sit or lie down for 10–15 minutes. The legs should be raised.
It is normal to feel slightly dizzy and weak. Don't worry - they will pass soon. But if you don’t feel well and get worse, immediately call the medical staff and tell them you’re feeling unwell. Other donors, on the contrary, feel a surge of strength and vigor.
A bandage will be placed over the area where the needle was inserted. Do not remove or wet it for at least 3 hours to avoid bruising.
You should not smoke for the first couple of hours. You should not shower on this day. Also, do not play sports and avoid physical activity for 2 days. There are also restrictions regarding vaccinations: they can only be done after 10 days.
In general, blood restoration is a short process. It takes about a month, sometimes a little more. But individual components are renewed in different ways: red blood cells will be restored in a month or a month and a half, leukocytes and platelets need a week, and plasma will be completely restored in a couple of days.
To speed up the process, you need to eat properly and regularly. Be sure to drink plenty of fluids and eat more protein. But you should give up alcohol for at least 2 days.
How often can you donate blood?
Men are allowed to undergo up to 5 donations per year, women even less - up to 4 times. In this case, at least 2 months must pass between two blood donations. And after 5 regular donations, you need to take a break for 3 months or more.
But if you donate only plasma, the period is significantly reduced: the procedure can be repeated again 2 weeks after the last donation. But you cannot donate plasma more than 20 times a year.
It will not be possible to undergo the procedure ahead of schedule, since each donor, as well as all his visits to the blood collection station, are noted in a single register. Violating the instructions is harmful to the donor’s health, since his body will not have time to recover before the appointed time.
Where to look for blood collection points
Regional centers and large cities most often have their own blood collection centers. Anyone wishing to become a donor can contact these institutions to find out whether they can be helpful, who should not undergo the procedure, how to undergo an initial medical examination, what needs to be done to become a donor, where to go, etc.
Typically, the requirements for future donors are standard everywhere, so there shouldn’t be any special problems.
To find out if there are suitable centers in your city and where they are located, use the DonorSearch web platform. This is a major project uniting Russian donors.
In addition, the Blood Service service will be useful, where you can find up-to-date information about donation and operating blood collection stations, as well as the official website of the Podari Zhizn Foundation, where you can find information about charitable events related to blood donation.
Benefits, privileges and payment
In order for the medical sector to be fully provided with donor blood and its components, it is necessary to have more than 40 donors for every 1,000 people.
Unfortunately, there is now an acute shortage of donors and their blood. In order for as many people as possible to become involved in this activity, the state has taken measures to provide social support for donors.
Firstly, after donation, you are issued a coupon for free food or monetary compensation in the amount of 500–1,000 rubles. It is impossible to say the exact figure, as it varies depending on the region.
Secondly, the donor is issued a certificate, thanks to which you can count on 2 days of leave while maintaining your earnings. This document must be given to the employer, and he has no right to refuse.
Moreover, the law allows you not to notify your boss about donating blood, and then simply bring the certificate to the accounting department. But I wouldn't advise you to do that! It is better to negotiate peacefully with your superiors.
If you donate blood on an ongoing basis, collect certificates and do not spend time off right away, you can accumulate up to 3 weeks of days off and extend your vacation. You cannot replace time off with monetary compensation.
Thirdly, you can donate blood for money. This can be done in public or private clinics, but not in all. Typically, rewards are offered to donors who have a rare blood type. You can find out about the payment amount and conditions directly at the transfusion station itself.
On average, donation is paid at the following rate:
- Whole blood – from 1,000 to 2,000 rubles.
- Plasma costs about 2–4 thousand rubles.
- Red blood cells – 5,000–6,000 rubles.
- Platelets from 7,000 to 9,000 rubles.
Fourthly, you can receive the status of an honorary donor.
Early history
Since ancient times, people have guessed about the importance of blood for the body. But there was no idea how to properly use it in medicine. The opportunity to put the matter on a scientific basis appeared only after 1628, when William Harvey formulated the theory of blood circulation. As usual, the first experiments were carried out on animals, and then in France and England there were even attempts to transfuse blood from animals to humans. But due to severe complications, a ban on such transfusions soon followed. It should be noted that transfusion at that time was a very complex procedure: there were no intravenous needles or syringes. All this was invented later.
Honorary donor status
In order to become an honorary donor, you must donate at least 40 times if you are talking about donating whole blood, and at least 60 times if you are donating plasma. Considering the number of possible donations per year, it will take from 3 to 10 years to obtain status.
It is important to donate blood without receiving compensation for donation. This is a mandatory rule. All cases where the donor received money for the procedure are not counted.
After the donor has a sufficient number of donations, he fills out an application and after a couple of months receives a certificate with an honorary donor badge.
What privileges can he count on:
- for the annual state payment, which depends on the cost of living, the payment now amounts to 15,108 rubles;
- for skip-the-line service at government agencies;
- a 50% discount on the purchase of drugs at a pharmacy with a prescription;
- on vacation at a time convenient for the donor;
- for priority receipt of discounted vouchers to sanatoriums.
You can also receive the status of an honorary donor of Moscow. To do this, you need to donate blood only in this city. The requirements in this case are somewhat simpler: it is enough to donate whole blood 20 times or plasma 30 times. Once the donor has an identification document confirming his status, he will need to donate blood and plasma at least 3 and 7 times annually, respectively.
This status implies the presence of its own benefits: free travel on public transport and a 50% reduction in payments for housing and communal services.
You can be an honorary donor to both Moscow and Russia at the same time.
Paid or free?
Should donors be compensated for donating blood? This question has arisen many times over the past 100 years, and different answers have been given.
When the first donor services began to appear at the beginning of the 20th century, blood was donated mainly by relatives of patients or altruistic volunteers. But the need for blood grew, and “professional” donors began to appear in many countries, for whom blood donation became a way to earn money (especially during the Great Depression). Paid donation has begun to take a dominant position.
But there were also voices against it: among paid donors, the proportion of people with dangerous infections was too high. Thus, when testing of donor blood for hepatitis B was introduced in the United States in later times, it turned out that the proportion of infected people among paid donors was three times higher than among free ones! And gradually a course was taken towards gratuitous donation, in which donors take more responsibility for their health and minimize the risk for both the recipient and the donor himself.
Now in many Western countries the transition to gratuitous donation has already practically occurred, and in some places paid donation is simply prohibited by law. It is clear that not all countries are yet ready to abandon donation fees: this transition depends on the general level of well-being and cannot be abrupt. Nevertheless, it is necessary to strive for it.
Harms and benefits of donating blood
Another important question for future donors: is it harmful to be a blood donor? No, donation is absolutely safe for a healthy body.
The body’s recovery occurs quite quickly - within a month the blood will be completely renewed. But even until this moment a person will not feel any special changes. And over time, regular donors develop resistance to bloodletting.
Some people believe that you can get an infection during the procedure. But that's not true. When donating blood, only disposable and sterile instruments are used. And before a catheter is inserted into the donor, his vein is disinfected.
Safety measures are also observed at blood collection points. Doctors strictly follow all the rules, carry out sanitary treatment before donations, walk only in shoe covers, and use disposable instruments.
If the donor becomes ill during the procedure, doctors provide assistance. Also, if necessary, donation can be interrupted at any time.
We figured out that there is no harm to the body. And now another question: is it useful to donate blood?
Studies show that donors are several times less at risk of heart attack and heart attack. Also, thanks to the procedure, the body learns to more easily adapt and adapt to any extreme situations, which has a positive effect on health.
In addition, the immune system is strengthened, metabolism is improved and life expectancy increases.
Signs of incompatibility
If the victim is infused with inappropriate donor biomaterial, this will cause specific symptoms. More often there are such deviations:
- Study: which blood type is considered the best: positive and negative aspects
- The patient becomes restless.
- The occurrence of discomfort and sharp pain in the lumbar region. This marker indicates that changes have begun to occur in the kidneys.
- Pallor of the skin.
- Increased breathing, shortness of breath.
- Increased body temperature or chills from feeling cold.
- Hypotension.
- Bacterial toxic shock. The violation is rare and occurs due to infection during transfusion.
5% show the following symptoms:
- Nausea and vomiting.
- Turning blue.
- The occurrence of severe convulsions.
- Involuntary urination and defecation.
In rare cases, there is a possibility of hemolytic shock. With this complication, it is necessary to immediately save the patient.