On an empty stomach or not? Instructions on how to take blood tests correctly
Every time a doctor prescribes blood tests, the question arises of how to properly prepare for the procedure in order to get the most accurate result.
The head of the clinical diagnostic laboratory, Candidate of Medical Sciences Olga Anatolyevna Litinskaya spoke about the most basic rules of preparation.
1. Most tests are done on an empty stomach. This means that 6-8 hours should pass between the last meal and the procedure. These tests include all biochemical indicators, some hormones, serological tests (HIV, hepatitis, syphilis), coagulogram. Before donating blood, at least 10-12 hours must pass for lipid spectrum indicators (cholesterol, triglycerides). Before taking a general blood test, you can indulge in a light breakfast. But after it, blood can be donated no earlier than 2-3 hours later. Juice, tea and coffee, especially with sugar, are also prohibited. But you can drink some water in the morning and brush your teeth. Dinner the day before should be light, without fatty foods, as this can lead to “turbidity” of the blood serum and complicate diagnosis. 2. Many hormones are subject to daily fluctuations, so they must be taken strictly before 12.00. These are thyroid hormones, parathyroid hormone, ACTH, cortisol and some others. 3. The test result may be affected by stress or physical activity (running, climbing stairs). It is advisable to rest for 10-15 minutes before the procedure and calm down. 4. Before donating blood, it is not recommended to take any medications, except in cases where it is necessary to determine the concentration of a substance in the blood. 5. Do not smoke an hour before the test, especially important for donating blood for glucose. 6. You cannot donate blood after an X-ray examination, CT and MRI, or physiotherapeutic procedures. 7. Special requirements for women of reproductive age (before menopause). Hormones such as FSH, LH, prolactin, estriol, estradiol, progesterone are released on certain days of the menstrual cycle. Be sure to follow your doctor's advice. 8. But PCR, genetic and autoimmune tests, allergy tests do not require special preparation. They can be taken at any time of the day. And one more important clarification. Different laboratories may use different methods for working with blood, and even the units of measurement may differ. It is correct to compare only those results that were performed in the same laboratory and at the same time of day. This is necessary for those who regularly donate blood for the same tests. The clinical diagnostic laboratory of the Federal State Budgetary Institution "NMITs TPM" of the Ministry of Health of Russia offers a wide range of laboratory services. We have modern equipment, qualified personnel, extensive experience and federal quality control at our disposal.
Most analyzes are completed in one business day.
Microbiological and PCR studies
- The study is recommended to be carried out before starting antibiotics and other antibacterial chemotherapy drugs (if this is not possible, then no earlier than 12 hours after discontinuation of the drug).
- Avoid taking laxatives, administering rectal suppositories, oils, limit taking medications that affect intestinal motility (belladonna, pilocarpine, etc.) and drugs that affect the color of stool (iron, bismuth, barium sulfate) for 72 hours before stool collection .
- The material obtained after an enema, after taking radiopaque substances (barium during X-ray examination) is unsuitable for research.
Decoding UAC indicators
Carrying out a clinical blood test allows us to identify deviations of the main indicators from the norm, which differ in men, women and children. Moreover, they also differ for children of different ages. Therefore, when interpreting the results, it is necessary to take into account the gender and age of the patient. The main parameter values are presented in the following table.
| No. | Parameter name | Normal value of the parameter depending on the gender of the patient | Purpose | Possible pathologies in case of deviations from the norm to the side | |
| wives | husband. | decrease | increase | ||
| Hemoglobin (Hb) | 120-140 g/l | 130-160 g/l | Transports oxygen from the lungs to tissues, internal organs and carbon dioxide in the opposite direction. | Anemia. | Dehydration, intestinal obstruction, congenital heart disease. |
| Red blood cells (RBC) | 3.7-4.7 g/l | 4.0-5.0 g/l | Red blood cells, in addition to transporting oxygen, help maintain the biological oxidation reaction. | Blood loss, anemia, overhydration. | A slight increase may be a consequence of a burn, diarrhea, or a consequence of taking diuretics. A significant increase indicates the possibility of kidney pathology, various neoplasms, disease and Cushing's syndrome. |
| Color Index (CPU) | 0,85–1,15% | Shows the concentration of hemoglobin in red blood cells. | Anemia. | Stomach cancer, polyposis, lack of folic acid in the body. | |
| Reticulocytes | 0,2–1,2% | Immature forms of young red blood cells produced by the bone marrow. | Aplastic and folate-deficiency anemia, kidney disease. | Iron deficiency, hemolytic anemia, blood loss. | |
| Platelets (PLT) | 180–320×109/l | Plates formed by bone marrow cells that are responsible for blood clotting. | Aplastic, hemolytic anemia, thrombocytopenic purpura, hemolytic disease, lupus erythematosus. | Inflammatory processes, polycythemia, tuberculosis, myeloid leukemia, rheumatoid arthritis. | |
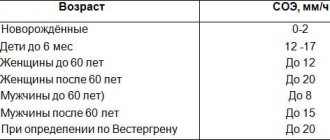
| ESR (erythrocyte sedimentation rate) | no more than 20 mm/h | no more than 15 mm/h | Characterizes the protein content in blood plasma. | Chronic circulatory failure, hyperbilirubinemia, erythremia, high levels of bile acids. | Infectious and inflammatory processes, cancer, pathologies of internal organs (kidneys, liver), endocrine system, autoimmune disorders, intoxication. |
| White blood cells (WBC) | 4.0–9.0×109/l | White blood cells protect the body from various types of infectious diseases (viral, bacterial, parasitic) and help eliminate dying cells. | A decrease in the level of white blood cells is called leukopenia. Indicates the presence in the body of viral diseases, bone marrow hypoplasia, cancer with the spread of metastases in the bone marrow, collagenosis, typhoid fever, rubella, systemic lupus erythematosus, viral hepatitis. | Exceeding the norm is called leukocytosis and indicates the presence of diseases such as meningitis, pneumonia, otitis media, pancreatitis, erysipelas, bronchitis. May be a consequence of purulent processes (sepsis), acute inflammatory disease. | |
| Lymphocytes | 1.0–4.5×109/l | One of the types of leukocytes directly involved in the creation of the immune defense system. | Myocardial infarction, pneumonia, HIV, sepsis, lymphoma, autoimmune diseases. | Influenza, adenovirus, other viral infections, lymphocytic leukemia, tuberculosis, threotoxicosis. | |
| Granulocytes | 1.2–6.7×109/l | They are a type of granular leukocytes that are susceptible to allergic and infectious diseases. | Aplastic anemia, tuberculosis, sarcoidosis, systemic lupus erythematosus, acute rheumatism, pemphigus, scarlet fever. | Allergic and inflammatory processes, myxedema, ulcerative colitis, chickenpox, Khldzhkin's disease. | |
| Monocytes | 0.1–0.6×109/l | Cells that have not yet matured. Penetrating into tissues, they are transformed into macrophages, capable of cleansing the body of dead cells, foreign elements, and various pathogens. | Damage, bone marrow dysfunction, radiation sickness, hairy cell leukemia. | An increased number of monocytes is called monocytosis. Signals about the possible presence of subacute endocarditis, brucellosis, mononucleosis, tuberculosis, syphilis, leukemia, sepsis, malaria, lymphoma, toxoplasmosis. |
Glucose tolerance test
Attention: A glucose tolerance test is prescribed only after consulting a doctor. This study is not performed for patients with type 1 diabetes mellitus.
Blood collection is carried out in the morning, after fasting: at least 12-14 hours must pass from the last meal.
- Before performing the glucose tolerance test, follow a diet for 3 days (no more than 150 grams of carbohydrates per day), exclude intense physical activity, and do not visit the bathhouse or sauna.
- 3 days before the test, stop thiazide diuretics, contraceptives and glucocorticoids (in consultation with your doctor).
- Do not drink water or smoke during the study. Repeated blood sampling is carried out 1 hour and 2 hours after the “load” of glucose.
Carrying out the procedure
Conducting an OAC is a common study. Taking the amount of biomaterial required for analysis is not difficult for either the laboratory assistant or the patient. The procedure is worked out to the smallest detail and consists of several mandatory steps.
- The patient takes off his outer clothing outside the office. In order for blood to flow freely from the wound, you need to keep your fingers warm, so in winter you need to first warm your hands in your pockets and gloves by placing them on the heating radiator. Don't rub your hands together.
- Upon entering the laboratory, the patient sits at the table opposite the laboratory assistant, after which he places his hand on a special pillow for drawing blood.
- To carry out the analysis, a small amount of capillary blood is required, which is usually obtained from the ring finger. This is due to the fact that he practically does not participate in various physical activities, so the risk of injuring the wound in this case is minimal. In addition, the hand and ring finger are separated from each other by an anatomical partition. Therefore, if bacteria gets into the puncture site, the infection will not be able to spread throughout the hand.
- The intended site for taking the test (finger pad) is treated with an antiseptic wipe, after which a small puncture is made on the side with a disposable scarifier to collect blood.
- The first drop of blood released is removed with a sterile napkin or cotton wool. The next portion of the biofluid is carefully collected into a glass adapter using a special tube, and then distributed into capillary blood tubes or placed on a glass slide.
- After completing the procedure, the wound is treated with an antiseptic to speed up the blood clotting process and a sterile cotton swab is pressed onto it.
- With low blood clotting and high blood pressure, bleeding may not stop for about 1-2 minutes. The cotton wool should be pressed as tightly as possible, and the hand should be raised with a finger up.
In young children (newborns) and some patients suffering from various pathologies, it can be very difficult to take blood for analysis from a finger prick. In this case, the puncture can be made on the earlobe or heel. Disposable sterile lancets are used as an applicator to puncture the skin of babies. The uniformity of the applied pressure minimizes pain and does not cause a negative psychological reaction in children.