Uterine bleeding is the discharge of blood from the uterine cavity. Unlike a woman’s normal menstrual cycle, it is characterized by abundance, intensity, and duration. Bleeding is caused by a serious disease or pathology. In any case, the manifestation of this disease should not occur without medical assistance. Girls of any age are at risk. Even in the first days after uterine life, bloody discharge from the genitals can be observed.
Every woman should know her cycle. It is considered normal if it is regular, occurs monthly and lasts, on average, 5 days. They begin sparingly, gain abundance towards the middle, and just as slowly begin to decrease. A healthy woman has no pain syndromes during menstruation. Everything else is a deviation or congenital pathology of the uterus. It can also mean a serious gynecological disease or hormonal imbalance. If your period occurs with pain, dizziness and weakness, immediately consult a gynecologist.
It should be understood that the onset of early menstruation in girls under the age of 11, as well as the resumption of bloody discharge in women after menopause (after 55 years), is a serious pathological abnormality and should not occur without medical supervision. There is no menstruation during pregnancy.
Sometimes, within normal limits, small blood discharge may be observed, which occurs during menstruation. The cause may be hormonal imbalance as a result of ovulation. The walls of the vessels become slightly thinner, so blood may come out along with the secretions. Duration 1 to 2 days maximum. Also, colds and inflammatory processes can have such side effects.
This pathology has the first and main symptom - the discharge of blood from the vagina. The volume of blood loss in a woman increases sharply. This can be noticed when changing special hygiene products too often. The cycle lasts more than 7 days. Its interval changes. After sexual intercourse, bleeding is observed. Bleeding after menopause, when the cycle has been stopped for a long time.
Cause of occurrence. Types of bleeding.
The cause of uterine bleeding is ovarian dysfunction. There is a malfunction in the system of the hypothalamus, pituitary gland and ovaries. The release of the pituitary hormone is disrupted, which provokes immaturity of the follicle. Ovulation and menstrual cycle are disrupted. The follicle does not mature in the ovary and the corpus luteum does not mature. The production of estrogen and progesterone stops. The endometrium is shed, resulting in uterine bleeding. It is released for a long time and abundantly.
During bleeding, the risk of developing diseases of the uterus and adnexal system, cancer, mastopathy, adenoma carcinoma increases.
There are many reasons that can cause uterine bleeding. It is necessary to determine the type of blood loss and understand what caused it. The cause may be either a disease of the genital organs or a malfunction in their functions.
Non-genital disorders include the following reasons:
- Some infectious diseases (measles, influenza).
- Cirrhosis of the liver.
- Hypertension.
- Atherosclerosis.
- Disorders of the urinary system.
- Changes in the thyroid gland.
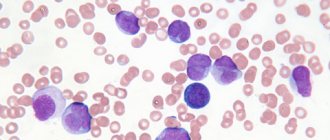
- Blood diseases.
Bleeding may begin during pregnancy. This may have a number of reasons, for example, ectopic pregnancy, as well as:
- scar on the uterus;
- endometritis;
- myoma;
- chorionepitheloma;
- birth canal injuries;
- ovarian pathology;
- uterine rupture;
- destruction of uterine tissue;
- departed placenta;
- early placental abruption or previa.
DUB in the pre- and perimenopausal period
During this period, uterine bleeding increases significantly due to the physiological depletion of the ovarian reserve and disruption of feedback between the levels of gonadotropins and peripheral ovarian hormones (estradiol, progesterone). It starts after the age of 40. The cyclicity is gradually disrupted: first, the intervals between monthly bleeding are reduced, and then they increase and turn into menometrorrhagia.
Treatment of DUB
Treatment is prescribed based on information obtained during diagnosis. Since it is at this age (45-55 years) that the proportion of organic causes of bleeding increases (fibroids, adenomyosis, polyps, tumors), hormonal hemostasis can be used as an exception, while surgical methods (removal of a submucosal node, polypectomy, diagnostic hysteroscopy and therapeutic) allow you to make the correct diagnosis and determine the individually necessary hormonal or surgical treatment.
Diagnosis of DMC
To accurately make a diagnosis, the following procedures are prescribed:
- Testing of the thyroid gland and sex hormones.
- Coagulogram.
- A smear from the cervix to detect cancerous tissue.
- Ultrasound and MRI of the pelvic organs.
- Checking the duration and frequency of the menstrual cycle.
- Separate diagnostic curettage.
- Hysteroscopy
Bleeding during pregnancy
Bleeding can also occur in a woman who is not carrying a child. May be caused by:
- rough sexual activity;
- taking contraceptives;
- trauma to the external genitalia;
- any damage to the uterus;
- inflammatory processes such as vaginitis, erosion, cervicitis;
- cyst and its rupture;
- ovarian rupture;
- introduction of mucous membrane into the uterus;
- benign and malignant tumors, such as fibroids;
- menopausal, juvenile and reproductive bleeding.
Classification:
In 2011, the FIGO (International Classification of Obstetrics and Gynecology) expert group proposed the PALM-COEIN classification system, which distinguishes two main groups of AUB - associated and not associated with organic pathology of the uterus.
The first group (PALM) includes four categories of disorders determined using visual diagnostic methods:
- polyp;
- adenomyosis (Adenomyosis);
- leiomyoma;
- malignancy and hyperplasia.
The second group (COEIN) includes categories of violations caused by:
- coagulopathy;
- ovulatory dysfunction;
- endometrial functional changes (Endometrial);
- iatrogenic changes (Iatrogenic);
- Not yet classified violations.
Bleeding during menopause
During menopause, women may experience uterine bleeding. They are of a different nature. This comes from the frequency of ovulation and hormone production. Quite a common occurrence, but you should consult a specialist. They may also indicate tumors. The reason for urgently visiting a doctor is:
- Copious discharge that special hygiene products cannot cope with.
- Discharge with clots.
- Exceeding the duration of menstruation by more than 3 days.
- Severe pain syndrome.
- Remember that they may indicate polyps, fibroids, imbalances, tumors and other serious diseases of the female reproductive system.
Bleeding due to hormonal imbalance
If the hormonal system changes or is disrupted, a woman may experience uterine bleeding. Women of any age are susceptible to this problem. If the brain function is abnormal, the level and production of the hormone is not controlled. An example of such a disease is pathology of the pituitary gland.
Lethargy and chronic fatigue, malnutrition and exhaustion of the body can cause this problem. Disorders of this type occur in a girl’s body during the first menstrual cycle, as well as after abortion, childbirth and during pregnancy. Prolonged bleeding caused by medical abortion is gaining popularity. Taking hormonal drugs and heredity are considered to be a number of causes.
Treatment should be selected individually; the cause that caused the disease should be determined.
Bleeding during pregnancy
Uterine bleeding during pregnancy most often indicates a miscarriage, ectopic pregnancy, or damage to the placenta. These reasons are accompanied by severe pain in the lower abdomen, nausea, vomiting, and malaise. Blood is bright red or dark scarlet, most often with clots.
The cervix can be damaged during pregnancy during a gynecological examination or sexual intercourse. Such bleeding is usually not prolonged or profuse. In the second or third trimester, bleeding may begin due to damage or placenta previa.
Bleeding poses a serious threat to the health and life of the mother and child. It should be understood that uterine bleeding is very dangerous for pregnant women. The woman should call an ambulance immediately.
Bleeding due to caesarean section
The cause of this bleeding is hemostasis. To do this, a medical intervention is performed in which the walls of the uterus are thoroughly cleaned. A caesarean section leaves behind a scar on the uterus, which prevents its normal contraction. Caesarean section requires a long healing time and may cause uterine bleeding. The woman should be under medical supervision, and after healing, when the first signs appear, immediately seek help.
Hypotonic bleeding is very difficult to stop because it occurs immediately after uterine contraction. Hypotonic shock may occur. In this case, doctors must immediately begin rescue and have a supply of blood for recovery.
The last degree of severity of uterine bleeding after cesarean section is removal of the uterus. It is used in cases where the patient’s salvation directly depends on stopping the bleeding, and other methods are powerless.
Gynecologists classify bleeding according to various criteria. The most common are:
Hypotonic. The fertilized egg is retained in the myometrium of the uterus. The cause is hypotension. Contraction of the muscle tissue of the uterus after childbirth occurs spontaneously. A critical condition occurs when it is completely absent. The bleeding should be stopped immediately. Replenish circulating blood volumes. Continuous measurement of blood pressure and pulse. Treatment is aimed at quickly restoring motor function of the uterus.
Hypotonic occurrence after childbirth requires removal of the placenta. It is this action that helps restore healthy functioning of the walls of the uterus. Perform massage if necessary. Apply ice or irritate the uterus with a swab soaked in ether. If hypotension does not stop, treatment of atony is started.
Atonic. Atonic appear when the uterus is unable to contract. In gynecology, the non-contractility of the uterus is called Couveler's uterus. Zero tone of the uterus does not make it possible to stop bleeding with the help of special injections and medications. To clamp the uterine artery, a thick suture is placed on the lip of the uterus and secured with additional clamps. The ineffectiveness of the method is considered as preparation for removal of the uterus. Critical blood loss is considered to be 1.2 liters or more. Electrical stimulation attempts to contract the blood vessels. Blood is constantly infused to prevent fainting.
Juvenile. Occurs during puberty. The main cause is ovarian dysfunction. Infection, psychological trauma, excessive physical activity, colds, and poor nutrition can cause juvenile bleeding. Climatic conditions are reflected. Treatment is carried out only in a hospital. Depending on the severity, this can lead to anemia. At the first detection, you should immediately call an ambulance, take a horizontal position, apply cold to the groin area and take a hemostatic drug.
Dysfunctional. Occurs when the ovaries malfunction. Absence of menstruation for a long time and heavy discharge are characteristic of this species.
Anuvulatory. Women during menopause and adolescents are susceptible to bleeding. Caused by disruption of follicles and progesterone during the absence of ovulation. It is also called single-phase; during bleeding, the corpus luteum does not form. A dangerous type of bleeding can cause the development of malignant tumors. Duration lasts more than 10 days. Bleeding occurs during a disruption of the pituitary gland, after infections, poisoning and stress.
Profuse. Not accompanied by pain. The amount of fluid lost may vary. The reasons may be different, from a previous abortion to taking hormonal drugs.
Column of a female doctor: on vacation without pads
I hope you know well that regular use of combined oral contraceptives (COCs) allows you to “push back” your period. If you are going to Bali or you are waiting for a meeting with a handsome prince, even light and painless menstruation can seriously spoil the holiday.
"How to postpone your period"
Such a request is not uncommon at a doctor’s appointment. Unfortunately, they usually ask for it urgently, or better yet, yesterday. They are looking for a remedy that is 100% effective, preferably not hormonal, preferably a folk remedy, ideally free. Everything as usual.
- The Internet is full of recommendations. Most often it is recommended to eat either one or 3 lemons a day. Particularly advanced ones suggest replacing lemon with a dose of ascorbic acid. The logic here is simple - ascorbic acid strengthens the vascular wall and, probably, can make it so strong that no enemy will pass through, and menstruation will not occur. Well, lemon is at least tasty. You can try it. From the same series and recommendations to drink parsley decoction. There are a lot of options - warm, cold, all day, every day. These recommendations make no sense, and the authors do not promise any significant effectiveness. The maximum is to postpone menstruation by 3-4 days. If you're lucky.
- The second group of tips relates to the use of hemostatic agents. There is a wider choice here - you can drink nettle decoction, water pepper extract, and take hemostatic drugs. The logic here is simple - these are hemostatic agents? So let them stop it! Of course, one can argue this way only if one completely throws out the remnants of school knowledge from one’s head. Menstruation is not just “blood”, it is the rejection of the endometrium, which was prepared for pregnancy, but the pregnancy did not take place. There are many adherents of this ineffective and unsafe approach; the risks are a little higher than in eating lemons, but welcome.
In order to postpone menstruation with a guarantee, you need to remember this much in advance. Preferably before ovulation. And certainly no later than the 14th day of the cycle. For this purpose, rigid gestagenic drugs are used. The tablets are taken daily continuously, as long as necessary to postpone menstruation.
– Oksana Valerievna, your pills didn’t help me! - Why didn’t they help? On what day did you start taking it? - Since the 14th. As soon as I arrived at the seaside, my period immediately arrived. – How long did you take it? - The whole pack!
20 tablets – exactly 10 days of use. I stopped taking it and after 2-3 days I got a menstrual-like reaction. Apparently I’m not explaining it clearly, unfortunately.
Of course, these are hormonal drugs. Of course, they are far from harmless.
It is still much easier for those who constantly use COCs. This is real freedom!
Manipulation of menstruation may well cause sacred horror. However, it is worth understanding that women using COCs do not and cannot have any menstruation. Bloody discharge during a hormone-free interval is nothing more than ordinary “withdrawal bleeding.” The body cannot count; it is illiterate. Therefore, the body does not care how many days we take COCs - 21, 24 or 63.
So, if you take contraceptive pills, then in order to “skip” menstrual bleeding, it is enough to skip the hormone-free interval.
As is customary in the modern world, “everything is not so simple,” so let’s delve into the details.
- The rule works for monophasic COCs - these are drugs in which all tablets are the same. As a rule, there are 21 tablets in a package.
- Be careful with packs of 28 tablets. If this is a COC (and not purely progestin contraceptives - that’s a completely different story), then the package contains inactive tablets in the 21+7 or 24+4 mode. If we want to postpone menstruation, we should take only active pills.
- If you are using a contraceptive patch, simply continue to apply the patches weekly until you return from vacation.
- If you are using a contraceptive ring, leave it in your vagina for 28 days, changing the ring on the 29th day.
- The most difficult story is with multiphase COCs. Frankly, these compositions are ill-suited to such skip-and-pull initiatives.
In recent years, the Seasonale regimen has been gaining popularity in the Russian Federation, in which monophasic COCs are taken in periods of 84 days. There are only 4 menstrual breaks per year. Gynecologists have long recommended the use of a prolonged regimen of COCs 84+7 or 63+3 for endometriosis, heavy bleeding, and menstrual migraines. Seasonale appealed to athletes, dancers, dog handlers, trainers, jockeys and just always busy business women.
Modern society has long abandoned the idea that menstruation cleanses a woman or “removes toxins.” There is no need for periodic bleeding in women taking COCs. To have or not to have a menstrual-like reaction is the free choice of every COC user.
Sunday start
Surely many of you have noticed that most COC tablets have additional markings for the days of the week. Of course, this idea can reduce the frequency of missed pills and contraceptive failures. However, the connection to the days of the week does not end there.
Traditionally, gynecologists recommend starting to take COCs on the 1st day of menstruation. It would not be a mistake to start taking the drug on the 2nd – 5th day of the cycle. This is where a little trick hides.
It is very convenient to start taking the pills on the first Sunday after the start of menstruation. This allows you to have “period-free” days off throughout your COC use.
If you are going to start your first pack of COCs, do it on Sunday. Please note that if menstruation began on Monday or Tuesday, it is worth using condoms for additional protection during the first week of taking COCs. If menstruation occurs on any day starting from Wednesday, contraceptive protection will begin with the 1st COC tablet.
If you are already taking oral contraceptives, but want to take advantage of the “free weekend”, feel free to shorten the hormone-free interval and start a new pack on Sunday. It is impossible to extend the hormone-free interval - contraceptive effectiveness is seriously affected. The most dangerous omissions of tablets are omissions at the beginning of the package.
Start on the day of admission
This trick is not very common in the Russian Federation, however, many colleagues in the decaying West recommend starting to take COCs on the same day that the doctor selected the drug. In this case, the first package of tablets does not have a contraceptive effect; additional methods of protection will have to be used. However, there is some (fairly high) chance that your period will move to the first hormone-free interval.
To be honest, I am very skeptical about this approach and do not apply it in my practice. I believe that instead of delaying menstruation, it is quite possible to get adaptive bleeding of varying intensity and unwanted pregnancy as a “last greeting” from interrupted sexual intercourse.
Menstruation can be easily pushed back, moved and shifted. It is not painful, not dangerous, completely normal and recommended for action. There is only one small “but” - these benefits of civilization are intended exclusively for advanced modern women who regularly use modern methods of highly effective contraception - estrogen-gestagen drugs.
Oksana Bogdashevskaya
Clots due to uterine bleeding
There are cases when a woman observes the presence of clots during bleeding. Doctors explain this by an anomaly that was transferred by the uterus in utero. The uterine cavity harbors blood, forming clots. Such menstruation brings a lot of discomfort to a woman, especially during a hormonal crisis. This anomaly sometimes causes a large number of clots to appear. The anomaly may also be acquired. They are associated with lifestyle, profession and addiction to bad habits.
Menstruation with clots causes severe pain. To rule out an anomaly, you should seek a gynecological consultation. To rule out the possibility of clots appearing on a hormonal background, take a hormone test and check the thyroid gland. The presence of clots and pain indicate endometriosis. If the diagnosis is confirmed, the disease requires urgent special treatment.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with an obstetrician-gynecologist with ultrasound examination (primary) | 4 200 |
| Taking gynecological smears | 700 |
| Hysteroscopy (diagnostic, therapeutic) | 47 500 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Stopping uterine bleeding
Upon arrival of the ambulance team, the following actions are carried out:
- apply cold to the stomach;
- in case of heavy bleeding, the woman is carried in a horizontal position;
- urgent hospitalization;
- specialist help;
- administration of the required solution depending on the type of uterine bleeding.
If the patient has not given birth and does not have tumors, treatment in the hospital is carried out with the help of hormonal drugs. Treatment begins with an increased dose, gradually increasing from 6 tablets per day to 1 piece. In the absence of anemia, gestogens are used. Hemostatic drugs are prescribed, for example Vikasol, Dicynon, Ascorutin.
During puberty, girls are prescribed medications that strengthen blood vessels and stop bleeding. It is recommended to take vitamins. Herbal medicine and hormonal drugs to regulate the menstrual cycle. Women of fertile age undergo surgery for endometriosis and fibroids. Pathology of the uterus and ovaries, cancer, after menopause requires only surgical intervention, removal of the appendages and uterus.
For proper treatment, it is very important to undergo a timely examination and establish the cause that caused the bleeding. Women exposed to this pathology should immediately seek medical help.
Treatment
To compensate for massive blood loss and eliminate the symptoms of acute anemia, urgent transfusions of blood, red blood cells, and plasma are used. At the international clinic Medica24 there is always a sufficient supply of donor blood and frozen plasma. This makes it possible to quickly replenish blood volume in case of large blood loss.
In case of emergency admission to the intensive care unit of the international clinic Medica24, doctors take quick measures to stop bleeding, such as intravenous administration of crystalloid solutions or uterine tamponade. After stabilization of the condition, comprehensive diagnostics and treatment are carried out.
We will call you back
Message sent!
expect a call, we will contact you shortly
Drug treatment
After identifying the cause of uterine bleeding, the Medica24 international clinic prescribes drug treatment according to indications, which may include:
- Hemostatic drugs.
- Hormonal medications (to normalize the menstrual cycle)
- Gland preparations (for the treatment of anemia).
- Vitamin and mineral complexes.
- Oxytocin (for uterine contractions).
- Non-steroidal anti-inflammatory drugs (NSAIDs).
- Antifibrinolytics.
- Antibiotics.
The patient's condition is under constant supervision by a doctor who monitors the dynamics of treatment.
This makes it possible to timely adjust the course, if necessary, cancel, replace or add certain drugs.
Surgery
If tumors are found during diagnosis, they are removed. Surgical treatment at the international clinic Medica24 is carried out primarily using minimally invasive, hysteroscopic methods.
Minimally invasive operations do not require a wide incision and its healing, and do not leave external marks. Recovery after such surgical interventions is much faster.
Hysteroscopic polypectomy, myomectomy
Removal of polyps and uterine fibroids is performed using a miniature device that is inserted into the uterus through the vagina.
The hysteroscope is equipped with a high-resolution video camera, the image from which is sent to a computer monitor. Thanks to this, the surgeon controls his actions with high precision when removing polyps, fibroids, purulent foci, endometrial remnants or other formations.
Endometrial ablation
One of the effective treatment methods is the destruction of the surface layer of the endometrium using radiofrequency radiation, laser or other means.
Endometrial ablation is used for menopausal bleeding because its side effect is infertility.
Hysterectomy
If histological examination shows the malignant nature of the tumor, complex treatment is carried out, which includes surgery, chemotherapy and other methods (targeted, immune, radiation therapy).
In the most serious cases, a decision is made to surgically remove the uterus - hysterectomy with preservation or removal of the uterine appendages.
The material was prepared by a gynecologist, oncologist at the international clinic Medica24, candidate of medical sciences Alimardonov Murad Bekmurotovich.
First aid
You should call an ambulance immediately. During pregnancy, a woman's condition worsens sharply because blood loss is profuse. Every minute counts. If it is not possible to contact a medical team, you should take the woman to the hospital yourself. The reaction must be quick; with uterine bleeding there is a serious threat to life. In case of dysfunctional bleeding, do not apply any warm heating pads to the abdomen, do not use medications, douching, or taking a bath.
Before the ambulance arrives, a woman can be helped independently by the following actions:
1. We put the woman to bed. In a horizontal position, it is advisable to raise your legs above your head. Prop up a pillow or roll up a blanket. In case of significant bleeding, this will help the patient not to lose consciousness.
2. Apply cold to your stomach. If you don’t have a heating pad or ice, replace it with any item from the refrigerator, after wrapping it in cloth. A plastic bottle with cold water will do. You can achieve vasoconstriction and reduce bleeding using cold in no more than 15 minutes. You should take 5 minute breaks.
3. The woman is given plenty of fluids. This will replace the IV at home. Make sweet tea or water.
4. Take medications seriously when carrying a child. If it is not possible to consult a doctor, you need to read the package insert and find out the minimum dose. Be sure to read the side effects. Upon arrival of medical workers, provide the name of the drug that the woman took and its dosage.
How to feel about “grandmothers’ recipes”?
In preparing this article, we conducted a survey and found out that, without exaggeration, a huge number of women are trying to cope with the situation of uterine bleeding on their own - using traditional medicine recipes. Naturally, in this case we are talking about moderate or scanty bleeding. The reasons for this state of affairs most likely lie in the absence of a certain culture of treatment and constant monitoring of one’s health. On the other hand, many books and brochures with various folk recipes can now be bought at any bookstore. It is also not difficult to find such information on the Internet. Recipes based on nettle, yarrow, St. John's wort, and viburnum are presented there as safe, effective, affordable, and, moreover, tested by several generations of women.
Without criticizing traditional medicine and recognizing its merits, we would like to focus your attention, first of all, on the inadmissibility of self-medication in case of uterine bleeding. As noted above, the causes of bleeding can be different. Bleeding is only a consequence, a symptom of the disease. You need to treat what caused it: tumor, dysfunction, uterine fibroids, endometriosis, etc. Therefore, it is extremely important to consult a doctor in a timely manner and correctly diagnose the causes of bleeding. And only then, in the treatment regimen, in some cases folk remedies can be used.
Diagnostics
At the first signs of uterine bleeding, contact your gynecologist immediately. Women should keep a calendar recording the nature, symptoms, well-being and duration of the menstrual cycle. This will help the gynecologist prescribe the correct treatment and complete the course of therapy faster. Performing ultrasound diagnostics, taking smears of the cervix to check for cancer. Blood tests are performed to determine hormone levels. A biopsy is performed to examine the endometrium under a microscope. Correct diagnosis is the key to optimal rehabilitation.
Symptoms
At the very beginning, the symptoms are vague, which makes this condition similar to various diseases. Doctors say that there are general symptoms that are characteristic of each type of blood fluid loss, while there are also certain signs that indicate a specific problem.
General symptoms of blood loss
Common signs of internal bleeding are:
- Dizziness.
- Nausea.
- Vomit.
- Fainting.
- Weakness.
- Cold sweating.
- The skin and whites of the eyes become pale.
- Apathy, I want to sleep, it is impossible to concentrate.
- Coma.
- Clouding of consciousness, a person reacts inadequately to everything that happens around him. This condition occurs in very severe cases.
You can recognize which vessel was injured:
- Capillaries – weak abundance of blood fluid.
- Capillaries from a parenchymal organ - profuse, prolonged bleeding.
- Artery - blood has a bright, red color, and the process itself is jerky.
- Vein - blood flows out smoothly, evenly, it has a dark color.
In addition, general symptoms in a child and an adult may depend on the severity of the loss of blood fluid:
- Minor – pulse increases slightly, blood pressure decreases.
- Medium – there is a drop in systolic pressure to 80 mm. rt. Art., increased heart rate, cold extremities, sometimes there is a slow reaction.
- Severe case - systolic pressure is less than 80 mm. rt. st, the respiratory rhythm is disturbed, sticky sweating appears, trembling in the hands, darkening in the eyes, thirst, apathy.
- Massive blood loss - blood pressure decreases greatly, the pulse quickens, consciousness becomes confused, delirium appears, the eyes become sunken.
- Fatal hemorrhage - coma ensues.
Signs of hemothorax
The manifestation of hemothorax is influenced by the degree of blood loss, compression of the lung tissue, as well as shift of the mediastinal organs. Small hemothorax is characterized by minimal or no symptoms. Doctors include moderate shortness of breath and pain in the sternum, which intensifies during coughing, as the main complaints. As for medium and large hemothorax, in such conditions respiratory and cardiovascular disorders are observed; during breathing and coughing, pain from the chest moves to the back and shoulder. The patient also feels weak, his blood pressure decreases, and tachypnea occurs. Severe hemothorax is characterized by fainting, pale skin, weakness, dizziness, and cold sweat.
According to medical statistics, 3-12% of patients develop a coagulated hemothorax. In this case, blood clots and fibrin layers form in the pleural cavity, which interferes with the respiratory function of the lung, this in turn gives impetus to the onset of sclerotic processes that affect the lung tissue. The clinical picture of such hemothorax is manifested by shortness of breath, heaviness and pain in the chest.
Signs of uterine bleeding
Distinctive symptoms of bleeding from the uterus in women are the release of blood fluid from the vagina, the appearance of a large volume of blood clots during menstruation, prolonged menstruation up to 7-8 days, and blood is observed after sexual intercourse. Otherwise, uterine bleeding may have signs that are common to internal blood loss of any kind.
Signs of hemorrhage in the urinary and digestive organs
Many people are interested in how to determine internal bleeding of the esophagus and urination. The following may indicate this condition:
- The stool takes on the color of tar and has a foul odor - the intestines and digestive organs are damaged.
- Vomiting has bloody clots or becomes like a coffee mass - the stomach or duodenum is affected, respectively.
- Bright blood from the anus - the hemorrhoids were damaged.
- Blood in the urine - the kidney area and urinary tract are affected.