Most people are accustomed to the fact that a cough is a companion to a cold or allergy. Could a cough be caused by the heart? Yes, because with cardiac pathologies, the synchronous functioning of the ventricles of the heart may be disrupted. The right one actively fills the lung tissue with blood, while the left one pumps it out more slowly. This provokes poor blood circulation and increased pressure in the lungs, which causes hypoxia. The patient constantly wants to cough and inhale more air, and most often the cough is dry. In such cases they talk about cardiac cough.
Causes of cardiac cough
One of the common symptoms of heart pathologies associated with lung function is shortness of breath. It can be felt already in the early stages of the disease. You can often notice that people with shortness of breath during physical or emotional stress begin to cough. This is the so-called “cough from the heart.”
This type of cough owes its origin to functional disorders of the heart muscle. Coughing in heart disease is a fairly common occurrence, because the heart muscle and its main vessels are closely connected to the lungs and bronchi.
Disturbances in blood flow in the pulmonary circulation can manifest themselves to varying degrees: at an early stage they can cause a slight cough, and in an advanced state – pulmonary edema. This is the most severe manifestation of heart failure and is associated with cough. In this case, the patient requires urgent medical attention. Now you have a unique opportunity to undergo a free consultation with a specialist and a set of preparatory examinations when enrolling in a course of enhanced external counterpulsation or shock wave therapy of the heart:
Promotion
Just until the end of autumn, undergo a free consultation and a set of preparatory examinations* when registering for a course of enhanced external counterpulsation or shock wave therapy of the heart.**
Send a request
* Check the details of the Promotion by phone. **Has contraindications; consultation with a doctor is required.
Enhanced external counterpulsation (EECP) Cardiac shock wave therapy (SWTS)
Hurry up to apply, the promotion period is limited.
Factors contributing to the development of ischemic heart disease
The main causes of the development of coronary heart disease can be identified:
- Arterial hypertension (increases the likelihood of developing ischemia by 2-6 times);
- smoking (in tobacco addicts, the risk of developing coronary heart disease is 1.5-6 times higher than in non-smokers);
- disturbance of lipid and lipoprotein metabolism (promotes the development of atherosclerosis and increases the risk of ischemia by 2-5 times);
- physical inactivity and obesity (obese, inactive people get sick at least 3 times more often than thin and athletic people);
- disorders of carbohydrate metabolism, diabetes mellitus (with both types of diabetes, the risk of developing coronary heart disease increases by 2-4 times).
Risk factors also include family history, being of the stronger sex, and old age. When two or more of the listed positions are combined, the risk of developing IHD increases significantly.
1 ECG for cardiac ischemia
2 ABPM in the diagnosis of ischemia
3 ECHO-CG for ischemic heart disease
How does cough occur in heart disease?
Weak functioning of the left ventricle and the pathological processes occurring in it are the main cause of cardiac cough. In this case we talk about left ventricular failure. It leads to deterioration of blood circulation in the pulmonary arteries, sclerosis of small vessels, and increased pressure in the lungs. Their tissues do not have enough oxygen - this is why the patient experiences shortness of breath and suffocates. In turn, problems in the pulmonary circulation aggravate the condition of the heart muscle.
One of the symptoms of cough in heart failure is hemoptysis. This phenomenon also has its own reason: since the volume of blood in the lungs exceeds the normal level, its excess accumulates and comes out of the bronchi when coughing. After all, a cough is a natural reaction of the body when the lungs, bronchi, and alveoli become overfilled with fluid or a foreign body enters them.
A cardiac cough almost always manifests itself at moments when the patient is exposed to physical exertion. However, if the cardiac dysfunction is quite severe, the patient only needs to take a lying position to start choking from coughing. In this case, excess fluid begins to intensively fill the lungs, causing irritation and continuous coughing.
Prevention
Preventing a disease is much easier than curing it. To maintain healthy arteries and blood vessels, it is necessary to eliminate risk factors that negatively affect your health:
- To give up smoking;
- Monitoring blood pressure levels
- Normalization of the level of “bad” cholesterol (low-density lipoproteins)
- Fighting stress and depression
- Minimize alcohol consumption;
- Refusal of smoked, fatty, fried and salty foods.
Spend more time on an active lifestyle: moderate physical activity, therapeutic exercises, morning exercises, walking, swimming, dancing. Physical activity will help strengthen the walls of blood vessels and maintain normal weight, and if necessary, reduce it.
The most important thing in prevention is timely observation by a specialist. In order not to visit medical institutions several times to undergo all the necessary tests and examinations, contact our cardiology center. Federal Research Center FMBA offers patients several programs for comprehensive heart research. You can find them here.
Cough due to heart failure
Heart failure is an extremely common disease associated with blood stagnation due to impaired circulation in large vessels. In most patients, this pathology is accompanied by shortness of breath and cough, which has the origin described above.
The nature of the cough can be different:
- paroxysmal and dry;
- exhausting and loud;
- irritating dry;
- sharp and short.
A cardiac cough can be a persistent problem for people with chronic heart failure . It occurs during times of physical or emotional stress and is usually characterized as dry and jerky.
In acute heart failure, a cough may begin with shortness of breath at night, which turns into suffocation due to the overfilling of the lungs with fluid. When breathing, the lungs begin to make bubbling sounds. The patient may cough producing bloody, frothy sputum due to a rapid increase in sputum volume in the lungs.
When to ask for help
Naturally, in the acute phase you need to seek help immediately. In other situations, if some atypical health problems begin that are embarrassing, you should not try to treat yourself. It is necessary to consult a doctor - a therapist or cardiologist. Moreover, you should not practice folk remedies - you can simply waste time. Those who have people in their family suffering from heart disease should be especially attentive to themselves. After all, hereditary risks in the development of cardiovascular pathologies are quite high.
Symptoms of cardiac cough
Most often, patients in the early stages of developing heart pathologies are alarmed by a dry cough that lasts a long time and is not associated with colds. Pain in the heart when coughing is a clear sign of problems in the functioning of this organ and a signal about the need to start treatment.
Subsequently, coughing attacks begin to overcome the patient even with minimal physical exertion and at night, often accompanied by the release of foamy sputum with traces of blood. This is why many heart patients sleep sitting up.
Other common symptoms include:
- increased heart rate;
- weakness and loss of consciousness;
- lack of air;
- swelling of the veins in the neck;
- bubbling in the lungs audible from a distance.
As already mentioned, a cardiac cough is almost always accompanied by shortness of breath. Unlike bronchitis, a cardiac cough rarely produces sputum. It also differs from a smoker's cough, which has a barking character.
Diagnostics
Diagnosis of coronary artery disease is carried out by cardiologists in several stages. When interviewing the patient, complaints are clarified and symptoms that may be characteristic of the disease are clarified. Examination of the patient helps to note visual changes - swelling and changed skin color (cyanosis); listening to the heart helps to identify murmurs and rhythm disturbances. Next, the patient undergoes laboratory tests for certain indicators in the blood, which may indicate pathology. Standard biochemical analysis is also important, as well as determination of glucose and cholesterol levels. But the most accurate diagnostic method is instrumental:
- ECG;
- Ultrasound of the heart;
- stress tests with physical activity or drug stimulation of the heart;
- Holter ECG monitoring;
- angiography of the coronary arteries (coronary angiography).
Timely examination helps to avoid serious consequences and the development of irreversible pathology. Spend a few hours on your health, because this time will help maintain your quality of life in the future.
Calcium agonists
Calcium agonists - are able to dilate the blood vessels of the heart, increasing the flow of blood to the heart muscle (myocardium), thereby reducing the number of angina attacks
.
They are divided into three main groups with characteristic features. Drugs from the group of dihydropyridine calcium antagonists
(nifedipine) can be prescribed together with beta blockers, or instead of beta blockers (if intolerance or contraindications to the latter).
The first generations (nifedipine) increase the heart rate, so short-acting tablets (nifedipine 10 mg) are prohibited for angina pectoris. There are special prolonged forms (osmo-adalat, corinfar-retard, nifecard) containing from 20 to 60 mg of nifedipine. The third generation of drugs (amlodipine, felodipine) practically does not increase the pulse rate and is taken once a day. Drugs from the verapamil and diltiazem group
reduce the heart rate; combined use with beta blockers is contraindicated due to the risk of bradycardia and other complications. It has been proven that regular use of calcium antagonists can reduce the incidence of strokes.
Antiplatelet agents
Antiaggregates help prevent the formation of blood clots (thrombi), reduce the aggregation (sticking together) of platelets - blood cells that are responsible for the formation of a blood clot. The list of antiplatelet agents includes: aspirin, cardiomagnyl, thienopyridines.
Aspirin (acetylsalicylic acid)
Aspirin (acetylsalicylic acid)
– the main antiplatelet agent, it is prescribed to all patients suffering from angina pectoris (with the exception of those who cannot tolerate it, for example, allergy sufferers with the “aspirin triad”). The dose of aspirin is 75-150 mg daily. Taken once, every 20-30 minutes. after meal. Typically in the afternoon. Pay attention to the low dose! A typical aspirin tablet contains 500 mg, a dose that has been taken as an analgesic and antipyretic for over 100 years! For angina pectoris, no more than 1/4 tablet is recommended. This dose effectively prevents thrombosis and is quite safe for the stomach. When regularly taking higher doses of aspirin (acetylsalicylic acid), there is a risk of developing erosions and stomach ulcers. Since patients with angina pectoris require constant use of aspirin as treatment, special, safer forms for long-term use have been developed.
Cardiomagnyl (aspirin + magnesium hydroxide)
Cardiomagnyl (aspirin + magnesium hydroxide)
75 and 150 mg. Magnesium hydroxide, which is part of the tablet, stimulates the formation of special protective substances in the stomach wall of a patient with angina pectoris that prevent the formation of ulcers and erosions.
Enteric-coated aspirin (AspirinCardio 100 mg, ThromboAss 50 and 100 mg, CardiASK 50 mg, etc.)
. The special coating does not allow the tablet to dissolve in the stomach; absorption of aspirin occurs in the intestines. Important: these tablets must be taken whole, you cannot break them or chew them (otherwise you will damage the shell and the protective effect will disappear)!
Thienopyridines (clopidogrel, prasugrel, ticlopidine)
Thienopyridines (clopidogrel, prasugrel, ticlopidine)
– have a very pronounced antiplatelet effect, hundreds of times stronger than aspirin.
The prescription of these drugs (usually together with aspirin) is necessary in cases where the risk of thrombosis is very high: unstable angina
,
acute coronary syndrome
(“pre-infarction conditions”),
acute myocardial infarction
and cardiac surgery (
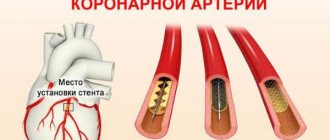
stenting
,
coronary artery bypass grafting
and etc.). Thienopyridines are also prescribed as a treatment for those patients who cannot take aspirin due to intolerance or contraindications.
Important:
Tell your doctor if you have previously had a stomach ulcer, duodenal ulcer (DU) or erosive gastritis, as well as unstable blood pressure with frequent crises, rises above 160-170/100 mm Hg. Art. This information will help your doctor make your antiplatelet treatment safe. It has been proven that regular use of antiplatelet drugs can reduce the incidence of myocardial infarction, strokes and death in patients with angina pectoris by up to 23% (in every 23 people out of 100)! After coronary angioplasty and stenting operations, doctors recommend taking aspirin and clopidogrel together for a certain period of time (from a month to several years).
Statins
Statins – antiatherosclerotic drugs
, reduce the level of “bad” cholesterol in the blood (total cholesterol, LDL, triglycerides), increase the level of “good” cholesterol (HDL). With long-term use of the drug in a dose that allows you to control cholesterol at the target level, they can stop the growth of atherosclerotic plaques and even reduce their size. Target cholesterol levels depend on the prevalence of atherosclerosis in the body and associated diseases (for example, diabetes). Ask your doctor what your target levels should be and monitor the effectiveness of treatment (blood tests for cholesterol and lipids) at least 4 times a year. There is no habituation to statins or development of dependence; treatment with statins should be carried out continuously. If you stop taking it on your own, then within one month after stopping the drug, your blood lipid levels return to baseline.
Statins
can reduce the risk of
myocardial infarction
and stroke by up to 30-40% (in every 30-40 people out of 100), and this effect is more pronounced in diabetics!
The fact that statins save lives became known after several large studies, which involved thousands and tens of thousands of patients with angina pectoris
, diabetes mellitus, and peripheral atherosclerosis.
Today, statins are recommended for treatment not only for patients with angina
, but also for people without coronary artery disease, with several risk factors, for the prevention of atherosclerosis, heart attack and stroke.
Four drugs in this group are registered in Russia: simvastatin (Zocor), rosuvastatin (Crestor), atorvastatin (Liprimar) and fluvastatin (Leskol).
How to take statins
Take statins in the evening (before bedtime). There are medications that can be taken at any time of the day. Nausea and stool disturbances are possible. The use of statins is not recommended for persons with active liver disease or during pregnancy and breastfeeding. A very rare side effect is muscle pain. If you start taking the drug and notice soreness in all the muscles of your body, be sure to tell your doctor to avoid unwanted complications. If you do not tolerate statins well or taking the maximum therapeutic dose does not allow you to control lipid levels, then it is possible to reduce the dose and add a cholesterol absorption inhibitor, ezetimibe. Your doctor may also recommend the use of other lipid-lowering drugs for treatment: fibrates, delayed-release nicotinic acid.
Observation
Duration of treatment
Treatment of coronary artery disease lasts a lifetime and must be carefully planned. During the observation period, it is necessary to strictly adhere to the developed treatment regimen, and if side effects occur or the condition worsens, immediately contact your doctor.
Many medications must be taken for life. These include aspirin (or analogs), blood pressure medications, medications to normalize blood sugar and cholesterol, and in some cases other medications. Sudden withdrawal of medication at will or even a reduction in dose can lead to a sharp deterioration in health and decompensation, and this increases the likelihood of fatal complications (heart attack, cardiac arrest, etc.).
Changes regarding lifestyle and routine must be decisive and unconditional. Often, small mistakes in the diet, such as eating too much herring, can lead to a sharp rise in blood pressure and worsening of the disease.
Doctor visits
Usually the doctor himself sets the date for the next visit. If he didn't, ask him about it. Careful medical supervision and regular checks are a necessary and important component of treatment. If you are unsure or doubt the adequacy of your doctor’s prescriptions, or want to get additional advice, contact a specialized advisory or diagnostic cardiology center.
Preventive hospitalizations
In the former USSR, the phenomenon of hospitalization for prevention was common. In the case of coronary artery disease, such a treatment strategy is not optimal either from the point of view of the quality of disease control or from the point of view of the patient's adherence to treatment, and should be avoided.
Treatment intermittently, from time to time, does not provide the necessary control over risk factors and the course of the disease for ischemic heart disease. Patients begin to be inclined to think that they will be “treated”, after which they will go back to their previous lives, and everything will be as before. This is a big misconception, which leads to refusal to take medications on a regular basis, large fluctuations in blood counts and pressure, and lack of control over the disease.
In one or two weeks spent in hospital every six months, it is impossible to achieve any real change in the course of the disease, other than some symptomatic improvement. Many patients perceive this improvement as a small victory over the disease and continue to live their previous lives. However, this is not at all true: coronary artery disease continues to progress without lifestyle changes and maintenance medications, ending in sudden death or heart attack. You can reduce your risk and prolong your life only with long-term, and not periodic, therapeutic effects.