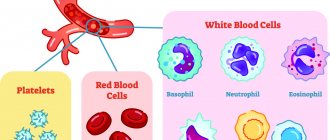
Among the laboratory techniques designed to assess the characteristics of red blood cells (erythrocytes - Er), not the least role belongs to the coloring of the smear and its morphological examination. Although, before the drug comes under the microscope lens, a person or machine (automatic hematology analyzer) will count red blood cells and determine the level of red blood pigment - hemoglobin (Hb). Having noticed some discrepancy, namely, a decrease in the level of hemoglobin in the blood with a normal content of red blood cells, the doctor, based on the data obtained, can calculate the color index (CI) and in case of its reduced value (below 0.8), without waiting for viewing the smear, give an unambiguous answer – hypochromia
. Of course, to establish a diagnosis, this answer cannot be final, but it will become an additional guideline for microscopic examination.
Hypochromia in a general blood test (CBC) indicates the development of hypochromic (mainly microcytic) anemia.
However, if the development of anemic syndrome is suspected, not only quantitative, but also qualitative (morphological) changes in the red blood must be taken into account.
Before morphological examination
The color index (CI), which characterizes the general condition of red blood cells, can be calculated using a simple and reliable formula:
CP = (Hb, g/l • 3) / first three values of total erythrocyte content
Possible results and their interpretation:
- CP is in the range of 0.85-1.05 - the norm for red blood cells containing a sufficient amount of hemoglobin.
- CP less than 0.8 – hypochromic anemia (hypochromasia), when the number of red blood cells is normal, but hemoglobin is insufficient.
- CP above 1.1 – hyperchromasia (hyperchromasia), above 1.4 – there is a deficiency of folic acid (vitamin B12), or pernicious anemia.
The color index is the ratio of hemoglobin to red blood cells, expressed in numbers. Hemoglobin deficiency and a low level of color index are a sign of iron deficiency or sideroachrestic anemia, which occurs due to impaired hemoglobin synthesis in erythroblasts. These conditions belong to the class of hypochromic anemias.
The correct calculation of the color index depends on the accuracy of determining the Hb level and counting the number of red blood cells. These criteria determine the presence or absence of anemic syndrome.
Primary sources of increasing values
Changes of physiological nature are provoked by:
- severe emotional stress;
- severe dehydration;
- long-term sports activities;
- living in high mountain areas.
The pathological form of erythrocytosis is associated with:
- with erythremia - tumor damage to the hematopoietic organs;
- heart defects - when arterial and venous blood is mixed, there is an insufficient supply of oxygen to the tissues; to compensate for the deviation, the bone marrow begins to produce a larger number of red blood cells;
- neoplasms in the kidneys, pituitary gland, adrenal glands or liver - the organs are responsible for the disposal of old elements in the blood, the formation of the disease leads to the cessation of this function, the tests indicate a predominance of mature forms;
- diseases of the respiratory tract and heart, infectious pathologies - a large number of young or reticular types of elements are observed;
- primary pulmonary hypertension;
- Pickwick's syndrome caused by obesity, pulmonary insufficiency, high blood pressure.
Less dangerous sources of development of an increased number of red blood cells include:
- lack of digestive enzymes;
- dehydration due to heat or prolonged physical activity;
- low-quality water: with chlorine, contaminated, highly carbonated;
- vitamin deficiency or deficiency due to liver dysfunction;
- smoking.
Against the backdrop of a large number of reasons causing changes in tests, only a doctor can correctly determine the original source of the deviation.
Qualitative and quantitative analysis
Counting the number of red blood cells performed using a hematology analyzer is not very informative. To obtain complete information, morphological or qualitative analysis is used.
What this research allows you to do:
- Examine the smear;
- Determine the size of red blood cells;
- Visually see the degree of saturation of red blood cells with hemoglobin.
Morphological signs of hypochromic anemia:
- Hypochromia;
- Hypochromia and microcytosis;
- The appearance of schizocytes (fragments of red blood cells) and normoblasts (young cells);
- Polychromatophilia is a condition when the smear contains red blood cells that can be stained with acidic and alkaline dyes;
- Fluctuations or lack of response from the white blood.
Cell size as an important indicator
If the CP values deviate from the norm, the hematologist analyzes the size of the red blood cells:
- Normal-sized red blood cells (normocytes), measuring 7-8 microns, can be present in some types of anemia;
- Macrocytes (erythrocytes with a diameter of more than 8 mm) – a sign of anisocytosis with a predominance of macrocytes;
- Microcytes (red blood cells with a diameter of less than 8 mm) are a sign of microcytic anemia.
If deviations from the norm appear, the hematologist studies the material using the Price-Jones curve.
Red blood cell staining intensity
An important criterion for assessing red blood cells is the intensity of their staining:
- Normochromia (normochromasia), when red blood cells saturated with Hb look like normal cells with a small bright spot in the middle of the cell, the CP is in the range of 0.85-1.0. This condition does not always correspond to the norm; it can be observed with normochromic anemia.
- Hyperchromia (hyperchromasia), when the median clearing does not differ from the rest of the erythrocyte due to excessive saturation with pigments. The CPU is more than 1.1.
- Hypochromia (hypochromasia), when the median clearing is excessively large, and the rim of the cell is very narrow due to poor saturation with red pigment. The condition is characterized by poor performance of erythrocytes’ functions.
The doctor, having assessed the characteristics of red blood cells during a morphological study, will identify anemia and reflect the diagnosis by drawing up a conclusion.
...their coloring
{banner_banstat3}
Meanwhile, in addition to the size of red blood cells, there is another, no less important criterion that gives a visual assessment - the intensity of staining of red blood cells:
- Red blood cells, fully (but not excessively!) saturated with hemoglobin, are visible under a microscope as normocytes with a small clearing in the middle of the cell - this is normochromia or normochromasia
, corresponding to a color index in the range of 0.85 - 1.0. And again, normochromia does not mean the absence of pathology; a proportional decrease in red cells and blood pigment is also designated as normochromia, but in fact normochromic anemia occurs; - Excessive saturation of erythrocytes with red blood pigment gives an excessively intense color, erasing the median clearing (CP - more than 1.1) - hyperchromia or hyperchromasia
; - A large median clearing and a narrow rim (ring) outlining the cell indicate hypochromia of erythrocytes or hypochromasia
(the greater the clearing, the greater the degree of anemia). This means that red blood cells (they are called anulocytes) are poorly saturated with red blood pigment, therefore, they will perform their main functional duties (delivering oxygen to tissues and organs) poorly.
A laboratory diagnostic doctor, having conducted a morphological study of red blood cells and seen changes in red blood cells (and this will certainly happen if most of the cells for some reason have changed their characteristics - size and color), will suspect the development of an anemic condition, which will be reflected in his conclusion. However, the topic of this work is hypochromia, so let’s return to it...
Degrees of hypochromia
Gradation of hypochromic anemia:
- 1st degree - the rim of the cells is colored, the clearing area is larger than usual;
- 2nd degree - the central clearing is wider than usual, approaching the membrane, the colored area is clear;
- 3rd degree - only the area near the membrane is colored, the red blood cell visually looks like a pale ring. It manifests itself in severe anemia, in very advanced stages.
Very often, hypochromia is accompanied by microcytosis; these symptoms are signs of hypochromic anemia. They become even more important if it is necessary to distinguish microcytic anemias from each other or differentiate them from other blood pathologies.
A reliable sign of hypochromic anemia
There are the following forms of anemic conditions included in the group of hypochromic anemias:
- Iron-deficiency anemia.
The most common form of hypochromic anemia.
Characteristic features:
- Microcytosis in combination with hypochromia;
- The color index is below normal;
- Reduced serum iron levels;
- Positive dynamics of treatment.
- Iron-saturated anemia (sideroachrestic).
The Hb level in this pathology steadily decreases due to ineffective absorption of iron to the site of hemoglobin synthesis. Occurs due to intoxication with industrial poisons, chemicals, side effects of medications that affect the formation of red blood cells.
Characteristic features:
- Low Hb;
- Hypochromia;
- Normal iron levels;
- Lack of effect from using drugs with high iron content.
- Iron redistribution anemia.
The etiology of this form of anemia is based on excessive hemolysis of red blood cells, tuberculosis, purulent processes, and cardiac pathologies. Refers to hypochromic microcytic anemia.
Characteristic features:
- Low Hb Level;
- Hypochromia;
- Serum iron levels are normal;
- Lack of effect from iron therapy.
When signs of different types are combined, a mixed form of hemochromatosis is diagnosed.
Classification Features
There are two types of erythrocytosis:
- Primary hereditary – refers to genetic pathologies, is rare. The source of the development of the disease is the low susceptibility of oxygen receptors in the kidneys and increased levels of erythropoietin. A sign of the disease is a pronounced loss of strength, attacks of dizziness, a change in the standard shade of the skin and mucous membranes into purple shades, and reduced blood clotting.
- Secondary or acquired - provoked by oxygen starvation of cells, occurs against the background of neoplasms in the liver, kidneys, and respiratory organs.
If the primary form of pathology is ignored, there is a risk of vascular complications, including thrombus formation. The problem is related to changes in the rate of blood clotting.
Causes of hypochromia
The etiology of hypochromia is based on hypochromic anemia.
Risk factors contributing to the development of hypochromia and anemia:
- Long-term or chronic blood loss (gastrointestinal tract, uterus);
- Chronic inflammatory processes (enteritis, organ resection), leading to impaired absorption of iron in the gastrointestinal tract;
- Malignant tumors of the gastrointestinal tract (stomach cancer);
- Increased need for iron, vitamins and microelements during pregnancy, lactation, increased growth of children and adolescents;
- Lack of iron and vitamins that help absorb it due to a sharp decrease in the intake of food into the body (during vegetarianism or following a diet).
Clinical signs of anemia depending on the severity and hemoglobin level:
- 1st degree (mild) – Hb level is below normal, but does not fall below 90 g/l;
- 2 degree (moderate) - Hb level in the range of 70-90 g/l, CP below 0.8, visual assessment of the smear shows moderate hypochromia;
- Grade 3 (severe) - Hb level is below 70 g/l, CP is reduced, visual assessment of the smear shows severe hypochromia.
The lower the degree of anemia, the less pronounced its manifestations.
Iron deficiency anemia in children
Why are iron supplements necessary for IDA? What are the advantages of the latest generation drugs? Why should iron supplements be taken for a long time?
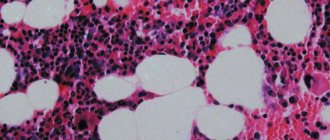
| Blood picture in chronic iron deficiency anemia. Severe hypochromia of erythrocytes, anisocytosis, poikilositosis, schizocils, the presence of polychromatophils |
Anemia is a pathological condition characterized by a decrease in red blood cell mass, often in combination with a decrease in the number of red blood cells per unit volume of blood.
There are many causes of anemia; For children, iron deficiency anemia (IDA) is most typical. IDA is characterized by the presence of small hypochromic red blood cells and depletion of iron stores in the body. The prevalence of iron deficiency in children at an early age, according to WHO, ranges from 17.5 to 30%.
The following reasons for the development of iron deficiency in children can be identified.
- Insufficient iron stores at birth. Premature babies, as well as children from mothers who suffered from anemia during pregnancy, are at risk for developing IDA. The condition of the placenta is also of great importance, since the positive balance of iron in the fetus is due to the perfect transport mechanisms of the placenta.
- Insufficient intake of iron from food and impaired absorption in the gastrointestinal tract. What matters is not so much the iron content in the product, but the efficiency of its absorption and assimilation. Iron is absorbed in the duodenum and jejunum, therefore, with various diseases of the digestive tract (chronic enteritis, malabsorption syndrome), iron deficiency can also develop due to impaired absorption.
- Increased need for iron due to growth, intensive processes of tissue differentiation, maturation of various organs and systems, and an increase in circulating blood volume. The need for iron is especially high during traction, puberty and during the formation of menstrual function in teenage girls.
- Excessive loss of iron by the body. This is primarily blood loss: bleeding of various locations (for diseases of the digestive tract - ulcerative processes, polyps, vascular anomalies, nasal), helminthic infestation, menstruation in teenage girls. Excessive loss of iron can occur with severe allergic manifestations on the skin due to the loss of a microelement with exfoliating epithelium, with frequent acute respiratory viral infections in children, since viruses and bacteria use the child’s iron for their metabolic processes.
It is important to note that in young children the causes of iron deficiency are, as a rule, insufficient iron stores and poor nutrition, and in older children - blood loss and sudden traction.
Pathophysiological aspects
Since iron absorption is limited, most people's dietary intake barely meets the body's current needs; iron deficiency can easily develop as a result of illness or poor nutrition. This process consists of several stages.
Stage 1. Iron loss exceeds iron intake. Against the background of a negative iron balance, its reserves in the bone marrow are gradually depleted. Although serum iron and hemoglobin levels remain normal, serum ferritin levels decrease (below 20 ng/mL). As iron stores are depleted, a compensatory increase in transferrin concentration occurs (as evidenced by an increase in iron-binding capacity).
Stage 2: Depleted iron stores no longer provide erythropoietic function to the bone marrow. While plasma transferrin levels rise, serum iron levels decrease, resulting in an increasing deficiency in red blood cell production. Erythropoiesis is impaired when iron levels are below 50 mcg% and transferrin saturation is below 16%. The concentration of ferritin receptors in the serum increases (more than 8.5 mg/l).
Stage 3. Anemia with apparently normal red blood cells and red blood cell indices.
Stage 4. Development of microcytosis and then hypochromia.
Stage 5: Iron deficiency is accompanied by symptoms of tissue disorders.
Clinical manifestations
The idea of the clinical status of a patient with anemia depends on the underlying disease and the form of anemia (acute or chronic). IDA is a chronic condition. The manifestation of anemia per se is explained using pathophysiological mechanisms. Most symptoms of IDA are a reflection of cardiovascular and gas exchange changes that compensate for the decrease in red blood cell mass. The severity of symptoms depends on the speed of development of anemia (with the slow development of anemia, characteristic of iron deficiency conditions, there is enough time for the full development of compensatory mechanisms) and its duration. Even moderate anemia is often asymptomatic. The child may complain of fatigue, shortness of breath and palpitations, especially after physical activity. In severe anemia, symptoms persist even at rest, and the patient cannot tolerate physical activity. If the hemoglobin level is less than 75 g/L, resting cardiac output increases markedly as both heart rate and stroke volume increase. Symptoms of heart failure develop when myocardial reserve is depleted. Consequently, the severity of the patient’s condition is determined primarily by the severity of cardiovascular disorders.
Symptoms of moderate to severe anemia extend to other organ systems. The patient often complains of dizziness and headaches, tinnitus, and even fainting is possible. The person becomes irritable, sleep is disturbed, and concentration decreases. Because blood flow to the skin is reduced, hypersensitivity to cold may develop. Symptoms also arise from the gastrointestinal tract - a sharp decrease in appetite, dyspeptic disorders (nausea, changes in the nature and frequency of stool), primarily due to the shunting of blood bypassing the vascular bed of the internal organs. In teenage girls, the menstrual cycle is disrupted, which manifests itself in the form of amenorrhea or heavy bleeding.
The main sign of anemia is pale skin. However, its information content is limited by other factors that determine skin color.
Therefore, the most informative sign of anemia is the pallor of visible mucous membranes - the mucous membrane of the oral cavity, the nail bed and the conjunctiva of the eyelids. The color of the skin on the folds of the palmar surface is also considered informative - if they do not differ in color from the surrounding skin, then the patient’s hemoglobin level is usually less than 80 g/l.
The development of pallor of the skin during anemia is explained by two factors: the first is, undoubtedly, a decrease in the level of hemoglobin in the blood, the second is the shunting of blood bypassing the vessels of the skin and other peripheral tissues, which promotes increased blood supply to vital organs. Redistribution of blood flow is one of the important mechanisms for compensating for anemia.
Other clinical symptoms of anemia include the already mentioned tachycardia, significant fluctuations in pulse pressure, systolic ejection murmur over the atria, decreased mental and physical activity, children become irritable, quickly get tired, their sleep is restless, and their appetite is reduced.
With IDA, the usual symptoms of anemia are accompanied by signs specific to iron deficiency. With prolonged iron deficiency, perverted appetite (eating chalk, dirt, paints) and sense of smell appear (like the strong smells of gasoline, paints, varnishes, eating ice (pagophagia), glossitis, cheilitis, koilonychia (thinned, striated, brittle nails) develop. With deficiency iron, the activity of the immune system decreases due to a decrease in the synthesis of IL-2 and T-killers; children are more likely to get ARVI, which, in turn, aggravates the existing iron deficiency.
The diagnosis is confirmed by laboratory data. The criterion for diagnosing IDA is microcytic, hypochromic, normoregenerative anemia. IDA is characterized by anisocytosis, thrombocytosis, decreased serum iron levels (less than 13 mmol/l), total iron-binding capacity of serum is unchanged or increased, serum ferritin level is less than 15 ng/ml, transferrin saturation is less than 16%, erythrocyte protoporphyrin level is increased, Hb level A2 is reduced, irritation of the red line is noted in the bone marrow (erythrocytes: granulocytes = 1:1 - 1:2), a typical lack of iron reserves and ring-shaped sideroblasts in the bone marrow.
The differential diagnostic search includes thalassemia, lead poisoning, anemia in chronic diseases, congenital disorders of iron metabolism (transferrin deficiency, impaired iron utilization, impaired iron reutilization), hemosiderosis, including Goodpasture's syndrome, copper deficiency.
Principles of treatment of IDA in children
- Elimination of the causes underlying the development of iron deficiency.
- Therapy for IDA should be carried out with iron supplements, since it is impossible to compensate for iron deficiency in this condition with diet therapy alone; true iron deficiency is not accompanied by a deficiency of vitamins B12, B6, and folic acid.
- The goal of therapy with iron supplements is to eliminate iron deficiency in the body, and not just to normalize hemoglobin levels, so the treatment period is long (at least 3 months).
- IDA therapy is carried out mainly with oral iron supplements.
- Blood transfusions for IDA are carried out only for health reasons.
Diet therapy for IDA in children
It is now generally accepted that it is impossible to eliminate iron deficiency in the body through diet therapy alone. This is due to the fact that the absorption of iron from food is limited - 1.8-2 mg (no more than 2.5 mg) of iron per day - even with a balanced diet appropriate for age and consumption of sufficient amounts of foods high in iron. (For comparison: a healthy child, depending on age, loses from 0.15 to 0.6 mg of iron per day, a girl during menstruation - 15-50 mg) When taking modern iron supplements, it is absorbed 20 times better. Diet therapy should be one of the components of IDA therapy in children.
On the other hand, it is very important to focus not on the iron content in food, but on its form. It is the form of iron that determines the percentage of its absorption and assimilation and, consequently, the effectiveness of therapy. Of the various forms of iron, the easiest to absorb is heme iron, a complex organic compound in which iron is found in hemoglobin; inorganic compounds - iron salts - are absorbed by the body much worse. Iron in heme is actively captured by the cells of the intestinal mucosa and absorbed unchanged. The processes of heme absorption in the intestine do not depend on the acidity of the environment and the activity of food enzymes. Iron from cereals, vegetables, and fruits is absorbed much less well due to the presence of ferroabsorption inhibitors in them, such as oxalates, phosphates, tannin and others. Compare: the absorption coefficient of iron from beef (heme iron) is 17-22%, from fruit - no more than 3%. The degree of absorption of iron from animal products also depends on the form of iron-containing compounds. Thus, from the liver, where iron compounds are presented in the form of ferritin and transferrin, iron is absorbed in significantly smaller quantities than from meat products, although the total iron content in the liver is 3 times higher than in meat. Therefore, including liver in the diet to eliminate iron deficiency or for preventive purposes does not make any sense. Thus, the diet should be as rich as possible in foods that contain iron in the form of heme (beef tongue, rabbit meat, beef).
It should also be noted that meat, liver and fish improve the absorption of iron from fruits and vegetables when consumed simultaneously.
The absorption of iron from cereals, legumes, tubers, vegetables, and fruits is much lower, since they contain iron in non-heme form, and largely depends on the content in the diet of substances that inhibit or potentiate the absorption of iron. Ascorbic acid, meat, poultry, fish products, as well as substances that reduce the acidity of food (for example, lactic acid) enhance the absorption of non-heme iron. Soy protein and polyphenols found in tea, coffee, nuts and legumes reduce the absorption of non-heme iron. Despite the high iron content in some products of plant origin, they cannot meet the high iron requirement characteristic of a growing organism, since iron from them is absorbed much less well than from animal products. Recommendations to consume large quantities of fruit juices, apples, pomegranates, buckwheat and other products in order to replenish iron depots in IDA also cannot be considered justified. A diet balanced in terms of the main ingredients allows you to “cover” only the physiological need of the child’s body for iron, but does not eliminate iron deficiency in any way and should be used in combination with iron supplements in the treatment of IDA. However, a complete and balanced diet plays an important role in preventing the development of iron deficiency in a child’s body during all periods of childhood.
Drug therapy for IDA
The main goal of IDA therapy is to eliminate iron deficiency in the child’s body. This is achieved by taking iron-containing medications. The main requirements for iron preparations are a sufficient content of elemental iron and the absence of side effects and complications. Currently, there is a sufficient selection of iron preparations on the Russian pharmaceutical market, which expands the physician’s capabilities and allows taking into account the individual characteristics of patients when prescribing treatment (Table 1). In particular, convenient forms for young children have appeared - drops and syrup (ferrum lek, maltofer, actiferrin, hemofer).
All drugs are registered and approved for use in the Russian Federation.
Modern iron supplements are divided into two groups:
- ionic iron-containing preparations (salts, polysaccharide iron compounds);
- non-ionic compounds, i.e. preparations represented by the hydroxide-polymaltose complex of ferric iron (ferrum lek, maltofer).
The absorption of iron from a medicinal product depends on the content of elemental (active) iron in it. The largest amount of elemental iron is contained in preparations in which iron is presented in the form of fumarate (ferretab, ferronate) or ferrous sulfate (actiferrin, ferro-foil, hemofer prolangatum, ferro-gradumet). Currently, a new generation of iron preparations has appeared, which include drugs represented by the hydroxide-polymaltose complex of ferric iron (maltofer, ferrum lek). The peculiarity of these drugs is that the entry of iron from the intestine into the blood occurs through active absorption, in contrast to iron salt compounds, the absorption of which occurs along a concentration gradient. This is important because it eliminates the possibility of an overdose of iron preparations containing ferric iron hydroxide-polymaltose complex.
Iron salt preparations in the intestinal lumen interact with food components and other medications, which complicates the absorption of iron. Therefore, this group of iron supplements is prescribed one hour before meals. However, against the background of pronounced free radical stress that occurs when iron interacts with the intestinal mucosa during its diffusion, the damaging effect of iron compounds on the intestinal mucosa increases, which is manifested by dyspeptic disorders, including necrosis of the mucosa. If iron salt preparations are poorly tolerated, they can be taken with food, which will reduce side effects, but iron absorption, in turn, will worsen. Iron salt preparations should not be taken with tea, milk or combined with certain medications (tetracyclines, chloramphenicol, calcium supplements, antacids, penicillamine), since this reduces the absorption of iron.
Nonionic iron preparations, as studies have shown, do not interact with food components and medications, which allows the use of these preparations without disturbing the diet of children (the preparations can be added to food, juices) and treatment regimens for concomitant pathologies (if there is a need for such treatment ).
The daily therapeutic dose of iron preparations should be sufficient to normalize hemoglobin levels and replenish iron reserves in the bone marrow, which for iron salt preparations is 3-6 mg/kg/day of elemental iron in two or three doses. Iron hydroxide-polymaltose complex (ferrum lek) is prescribed at a dose of 3-6 mg/kg/day in one or more (at the patient’s request) doses.
Adverse reactions when taking iron supplements
The most common side effects observed during treatment with ferrodrugs (Table 2): metallic taste in the mouth, darkening of tooth enamel, allergic skin rashes, dyspeptic disorders as a result of irritation to the mucous membrane of the digestive tract, especially the intestines (loose stools, nausea, vomiting ). Therefore, the initial doses of drugs should be 1/2-1/3 of the therapeutic dose, followed by increasing them to the full dose over several days in order to avoid the occurrence of severe side effects. If you are intolerant to the salt preparation, it can be replaced with an iron hydroxide-polymaltose complex, the use of which does not result in the above-described effects. Iron hydroxide-polymaltose complex can be used immediately in full dose. Non-ionic iron preparations do not cause the side effects listed above, and a feeling of stomach fullness is also rare.
Parenteral administration of iron supplements
Parenteral administration of iron supplements is carried out only under strict indications due to the development of pronounced local and systemic side effects. Indications are as follows: pathology of the digestive tract (impaired intestinal absorption syndrome, ulcerative colitis, chronic enterocolitis, gastrointestinal bleeding) and intolerance to iron-containing drugs when taken orally.
Contraindications to the prescription of iron supplements are anemia not caused by iron deficiency (hemolytic, aplastic), hemosiderosis, hemochromatosis.
Duration of treatment
The clinical and therapeutic effects of oral ferrotherapy develop gradually. After some time, clinical improvement appears: weakness decreases, dizziness disappears, the child becomes more active, appetite increases, and the skin and visible mucous membranes gradually turn pink. On the 8-10th day of therapy, a reticulocyte crisis is observed - up to 5%, which confirms the effectiveness of treatment. Later, an increase in hemoglobin levels is observed; most often, normalization of hemoglobin occurs in the 3-6th week from the start of therapy and depends on the severity of anemia. On average, Hb levels increase by 10 g/l in 10 days. However, normalization of hemoglobin levels is not a sign of elimination of iron deficiency. To completely replenish the iron depot in the body, the course of ferrotherapy should be at least 3 months.
Reasons for the ineffectiveness of ferrotherapy
The ineffectiveness of therapy while taking iron supplements, if they are well tolerated, may be due to the following factors:
- wrong diagnosis,
- ongoing blood loss
- intercurrent diseases (ARVI, exacerbation of chronic foci of infection).
IDA is a disease that, with proper treatment, can lead to complete recovery!