The study of the health of a person with cardiovascular diseases needs to determine “reserves” and functional capabilities. Such characteristics are especially important in the selection of treatment tactics for severe cases, cardiogenic and toxic shock, and in preparation for cardiac surgery.
The cardiac index is not measured by any device. It belongs to the group of calculated indicators. This means that to determine it it is necessary to know other quantities.
What indicators need to be measured to calculate the cardiac index?
To determine the cardiac index you need:
- volume of blood circulation in one minute - the volume of blood pushed by both ventricles in 1 minute;
- the total body surface area of the person being studied.
Minute volume of blood circulation or cardiac output is a measured indicator. It is determined using special sensors located at the end of a floating catheter.
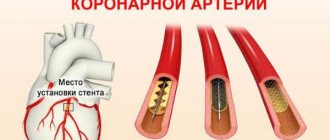
By catheterizing the right subclavian vein, a catheter is inserted into the atrium, then into the ventricle and pulmonary artery
The technique is called "thermodilution". Registration of dilution and “warming” of the injected saline or glucose (5-10 ml required) from room temperature to the core temperature in the bloodstream is used. Computer programs are able to register and quickly calculate the necessary parameters.
The requirements for the method must be strictly followed, since violation leads to inaccurate results:
- inject the solution quickly (within four seconds);
- the moment of administration should coincide with maximum exhalation;
- take 2 measurements and take the average, and the difference should not exceed 10%.
To calculate the total surface area of the human body, use the Du Bois formula, in which body weight and height in meters, corrected by coefficients, measured in kg, are multiplied by a standard coefficient of 0.007184.
General view of the formula for body area (S) in m2: (weight x 0.423) x (height x 0.725) x 0.007184.
Cardiac output, its fractions. Systolic and minute blood volumes. Cardiac index.
The amount of blood ejected by the ventricle of the heart into the arteries per minute is an important indicator of the functional state of the cardiovascular system (CVS) and is called minute blood volume (MBV). It is the same for both ventricles and at rest is 4.5–5 liters.
An important characteristic of the pumping function of the heart is the stroke volume, also called systolic volume or systolic ejection. Stroke volume is the amount of blood ejected by the ventricle of the heart into the arterial system in one systole. (If you divide the IOC by the heart rate per minute, we get the systolic volume (SV) of blood flow.) With a heart contraction of 75 beats per minute, it is 65–70 ml; during work it increases to 125 ml. In athletes at rest it is 100 ml, during work it increases to 180 ml. The determination of MOC and CO is widely used in the clinic.
Ejection fraction (EF) is the percentage ratio of the stroke volume of the heart to the end-diastolic volume of the ventricle. EF at rest in a healthy person is 50-75%, and during physical activity it can reach 80%.
The volume of blood in the ventricular cavity that it occupies before its systole is the end-diastolic volume (120–130 ml).
End-systolic volume (ESV) is the amount of blood remaining in the ventricle immediately after systole. At rest, it is less than 50% of the EDV, or 50-60 ml. Part of this blood volume is reserve volume.
The reserve volume is realized when CO increases under load. Normally, it is 15–20% of the end-diastolic value.
The volume of blood in the cavities of the heart remaining when the reserve volume is fully realized at maximum systole constitutes the residual volume. CO and IOC values are not constant. During muscular activity, IOC increases to 30–38 l due to increased heart rate and increased CO2.
A number of indicators are used to assess the contractility of the heart muscle. These include: ejection fraction, rate of blood expulsion during the rapid filling phase, rate of increase in pressure in the ventricle during the period of stress (measured by probing the ventricle)/
The rate of blood expulsion is changed using Doppler ultrasound of the heart.
The rate of increase in pressure in the cavities of the ventricles is considered one of the most reliable indicators of myocardial contractility. For the left ventricle, the normal value of this indicator is 2000-2500 mmHg/s.
A decrease in the ejection fraction below 50%, a decrease in the rate of blood expulsion, and the rate of pressure increase indicate a decrease in myocardial contractility and the possibility of developing insufficiency of the pumping function of the heart.
The value of the IOC divided by the body surface area in m2 is determined as the cardiac index (l/min/m2).
SI = MOK/S (l/min×m2)
It is an indicator of the pumping function of the heart. Normally, the cardiac index is 3–4 l/min×m2.
IOC, SV and CI are united by the common concept of cardiac output.
If the IOC and blood pressure in the aorta (or pulmonary artery) are known, the external work of the heart can be determined
P = IOC × BP
P is the work of the heart in minutes in kilograms (kg/m).
MOC—minute blood volume (l).
Blood pressure is pressure in meters of water column.
At physical rest, the external work of the heart is 70–110 J; during work it increases to 800 J, for each ventricle separately.
Thus, the work of the heart is determined by 2 factors:
1. The amount of blood flowing to it.
2. Vascular resistance during the expulsion of blood into the arteries (aorta and pulmonary artery). When the heart cannot pump all the blood into the arteries at a given vascular resistance, heart failure occurs.
There are 3 types of heart failure:
1. Insufficiency from overload, when excessive demands are placed on the heart with normal contractility due to defects, hypertension.
2. Heart failure due to myocardial damage: infections, intoxications, vitamin deficiencies, impaired coronary circulation. At the same time, the contractile function of the heart decreases.
3. Mixed form of failure - with rheumatism, dystrophic changes in the myocardium, etc.
The entire complex of manifestations of heart activity is recorded using various physiological techniques - cardiography: ECG, electrokymography, ballistocardiography, dynamocardiography, apical cardiography, ultrasound cardiography, etc.
The diagnostic method for the clinic is the electrical recording of the movement of the contour of the heart shadow on the screen of the X-ray machine. A photocell connected to an oscilloscope is applied to the screen at the edges of the heart contour. As the heart moves, the illumination of the photocell changes. This is recorded by an oscilloscope in the form of a curve of contraction and relaxation of the heart. This technique is called electrokymography.
The apical cardiogram is recorded by any system that detects small local movements. The sensor is fixed in the 5th intercostal space above the site of the cardiac impulse. Characterizes all phases of the cardiac cycle. But it is not always possible to register all phases: the cardiac impulse is projected differently, and part of the force is applied to the ribs. The recording may differ from person to person and from one person to another, depending on the degree of development of the fat layer, etc.
The clinic also uses research methods based on the use of ultrasound - ultrasound cardiography.
Ultrasonic vibrations at a frequency of 500 kHz and higher penetrate deeply through tissues being generated by ultrasound emitters applied to the surface of the chest. Ultrasound is reflected from tissues of various densities - from the outer and inner surface of the heart, from blood vessels, from valves. The time it takes for the reflected ultrasound to reach the capturing device is determined.
If the reflective surface moves, the return time of the ultrasonic vibrations changes. This method can be used to record changes in the configuration of heart structures during its activity in the form of curves recorded from the screen of a cathode ray tube. These techniques are called non-invasive.
Invasive techniques include:
Catheterization of the heart cavities. An elastic catheter probe is inserted into the central end of the opened brachial vein and pushed towards the heart (into its right half). A probe is inserted into the aorta or left ventricle through the brachial artery.
Ultrasound scanning - an ultrasound source is inserted into the heart using a catheter.
Angiography is the study of heart movements in a field of X-rays, etc.
Mechanical and sound manifestations of cardiac activity. Heart sounds, their genesis. Polycardiography. Comparison in time of periods and phases of the cardiac cycle of ECG and FCG and mechanical manifestations of cardiac activity.
Heart beat. During diastole, the heart takes the shape of an ellipsoid. During systole, it takes on the shape of a ball, its longitudinal diameter decreases, and its transverse diameter increases. During systole, the apex rises and presses against the anterior chest wall. A cardiac impulse occurs in the 5th intercostal space, which can be recorded (apical cardiography). The expulsion of blood from the ventricles and its movement through the vessels, due to reactive recoil, causes vibrations of the entire body. The recording of these oscillations is called ballistocardiography. The work of the heart is also accompanied by sound phenomena.
Heart sounds. When listening to the heart, two sounds are detected: the first is systolic, the second is diastolic.
- The systolic tone is low, prolonged (0.12 s). Several overlapping components are involved in its genesis:
1. Mitral valve closure component.
2. Closure of the tricuspid valve.
3. Pulmonary tone of blood expulsion.
4. Aortic tone of blood expulsion.
The characteristic of the first tone is determined by the tension of the leaflet valves, the tension of the tendon threads, papillary muscles, and the walls of the ventricular myocardium.
Components of blood expulsion occur when the walls of the great vessels are tense. The first sound is clearly audible in the 5th left intercostal space. In pathology, the genesis of the first tone involves:
1. Aortic valve opening component.
2. Opening of the pulmonary valve.
3. Tone of pulmonary artery distension.
4. Aortic stretch tone.
Strengthening of the first tone can occur with:
1. Hyperdynamics: physical activity, emotions.
- When there is a violation of the time relationship between the systole of the atria and ventricles.
- With poor filling of the left ventricle (especially with mitral stenosis, when the valves do not open completely). The third option of amplifying the first tone has significant diagnostic value.
Weakening of the first sound is possible with mitral valve insufficiency, when the valves do not close tightly, with myocardial damage, etc.
- II tone - diastolic (high, short 0.08 s). Occurs when the closed semilunar valves are tense. On the sphygmogram its equivalent is incisura. The higher the pressure in the aorta and pulmonary artery, the higher the tone. It can be heard well in the 2nd intercostal space on the right and left of the sternum. It intensifies with sclerosis of the ascending aorta and pulmonary artery. The sound of the 1st and 2nd heart sounds most closely conveys the combination of sounds when pronouncing the phrase “LAB-DAB”.
studfiles.net
Formula and decoding
The cardiac index is determined by the ratio of cardiac output to the total body surface area. Normally it is from 2 to 4 l/min.m2. The indicator makes it possible to level out differences between patients in weight and height and take into account the dependence only on minute blood flow.
Therefore, it increases with increasing emissions in the following cases:
You can also read: Heart hump in children
- hypoxia of myocardial tissue;
- increased carbon dioxide levels in the blood;
- accumulation of liquid part of the blood (hypervolemia);
- tachycardia;
- increased body temperature;
- accelerated metabolism;
- stress state;
- in the initial stage of shock.
A decrease in cardiac index is accompanied by:
- shock state in the 3rd or more stages;
- tachycardia over 150 beats per minute;
- deep anesthesia;
- decrease in body temperature;
- large acute blood loss;
- decrease in the liquid part of the blood (hypovolemia).
In a healthy body, fluctuations in the index are possible due to age and gender.
Cardiac index
Among the constants or indices that individually characterize the state of hemodynamics, the Grollman index deserves some attention. It is the ratio of the cardiac output (in liters) to the body surface (in square meters):
SI=MO/ST,
where: MO—minute volume of the heart, l;
ST—body surface, m2 (PT).
Normally, at rest, according to Grollman, in healthy individuals there is an average of 2.2-2.4 liters of blood per 1 m2 of body surface.
Conducted by N.N. Savitsky (S.O. Vulfovich, A.V. Kukoverov, 1935; V.I. Kuznetsov, M.S. Kushakovsky, 1962) studies showed that the cardiac index lies in the range of 2.00-2.45, which gives the right use its average value - 2.23. The value of the cardiac index depends to a certain extent on age and gender.
Determining the systolic and minute volumes of circulation allows you to calculate the work performed by the heart. But calculating the work of the heart does not allow one to judge the amount of tension that the contractile myocardium develops during its execution and thus does not provide a quantitative idea of the strength of heart contractions. I.P. Pavlov back in 1882-1887. used to assess the force of contractions of the left ventricle a method for determining the second volume of the heart—the rate of blood expulsion into the aorta.
The introduction of mechanocardiography into clinical practice makes it possible to obtain a number of values that, to a certain extent, characterize the strength of heart contractions: volumetric ejection velocity (VEV), linear blood velocity (LBV), power of contractions of the left ventricle (M), energy consumption of heart contractions per 1 liter of minute volume blood circulation (BC).
Determination of these quantities creates the most complete picture of the contractile function of the myocardium.
gemodinamika.ru
Reserve limits of the indicator
In a horizontal position, at rest, the minute volume of a healthy person averages 5–5.5 l/min. Accordingly, under the same conditions, the average cardiac index will be 3–3.5 l/min*m2.
For athletes, the reserve reaches 700%, and the minute volume reaches 40 liters.
With high physical activity, the functionality of the heart muscle increases to 300–400%. 25–30 liters of blood are pumped per minute.
The value of the cardiac index changes in direct proportion.
Cardiac output. Systolic blood volume
Cardiac output refers to the amount of blood ejected by the heart into the vessels per unit time.
In the clinical literature, the concepts used are minute volume of blood circulation (MCV) and systolic, or stroke, blood volume.
Minute volume of blood circulation characterizes the total amount of blood pumped by the right or left side of the heart within one minute in the cardiovascular system.
The measurement of minute volume of blood circulation is l/min or ml/min. In order to level out the influence of individual anthropometric differences on the value of the IOC, it is expressed as a cardiac index.
Cardiac index is the value of minute volume of blood circulation divided by body surface area in m2. The dimension of the cardiac index is l/(min-m2).
In the oxygen transport system, the circulatory apparatus is the limiting link, therefore the ratio of the maximum value of IOC, manifested during maximally intense muscular work, with its value under basal metabolic conditions gives an idea of the functional reserve of the entire cardiovascular system. The same ratio also reflects the functional reserve of the heart itself in terms of its hemodynamic function. The hemodynamic functional reserve of the heart in healthy people is 300-400%. This means that resting IOC can be increased by 3-4 times. In physically trained individuals, the functional reserve is higher - it reaches 500-700%.
For conditions of physical rest and horizontal position of the subject’s body, normal IOC values correspond to the range of 4-6 l/min (values of 5-5.5 l/min are more often given). The average values of the cardiac index range from 2 to 4 l/(min.m2) - values of the order of 3-3.5 l/(min*m2) are more often given.
Since the human blood volume is only 5-6 liters, the complete circulation of the entire blood volume occurs in approximately 1 minute. During periods of heavy work, the IOC in a healthy person can increase to 25-30 l/min, and in athletes - up to 35-40 l/min.
For large animals, a linear relationship has been established between the IOC value and body weight, while the relationship with body surface area is nonlinear. In this regard, in studies in animals, the IOC is calculated in ml per 1 kg of weight.
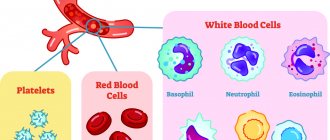
The factors that determine the value of IOC, along with the TPR mentioned above, are systolic blood volume, heart rate and venous return of blood to the heart.
The volume of blood pumped by each ventricle into the main vessel (aorta or pulmonary artery) during one contraction of the heart is designated as systolic, or stroke volume of blood.
At rest, the volume of blood ejected from the ventricle is normally between one-third and one-half of the total amount of blood contained in this chamber of the heart at the end of diastole. The reserve volume of blood remaining in the heart after systole is a kind of depot, providing an increase in cardiac output in situations in which rapid intensification of hemodynamics is required (for example, during physical activity, emotional stress, etc.).
The amount of reserve blood volume is one of the main determinants of the functional reserve of the heart for its specific function - the movement of blood in the system. As the reserve volume increases, the maximum systolic volume that can be ejected from the heart under conditions of intense activity increases accordingly.
During adaptive reactions of the circulatory apparatus, changes in systolic volume are achieved using self-regulation mechanisms under the influence of extracardiac nervous mechanisms. Regulatory influences are realized in changes in systolic volume by influencing the contractile force of the myocardium. As the power of cardiac contraction decreases, systolic volume decreases.
In a person with a horizontal body position under resting conditions, the systolic volume ranges from 70 to 100 ml.
The resting heart rate (pulse) ranges from 60 to 80 beats per minute. Influences that cause changes in heart rate are called chronotropic, while those that cause changes in the strength of heart contractions are called inotropic.
An increase in heart rate is an important adaptive mechanism for increasing the IOC, which quickly adapts its value to the body's requirements. With some extreme effects on the body, the heart rate can increase 3-3.5 times relative to the original one. Changes in heart rate are carried out mainly due to the chronotropic influence of the sympathetic and vagus nerves on the sinoatrial node of the heart, and, under natural conditions, chronotropic changes in cardiac activity are usually accompanied by inotropic effects on the myocardium.
An important indicator of systemic hemodynamics is the work of the heart, which is calculated as the product of the mass of blood ejected into the aorta per unit of time and the mean arterial pressure over the same period. The work calculated in this way characterizes the activity of the left ventricle. It is believed that the work of the right ventricle is 25% of this value.
Contractility, characteristic of all types of muscle tissue, is realized in the myocardium due to three specific properties that are provided by various cellular elements of the heart muscle.
These properties are:
Automaticity is the ability of pacemaker cells to generate impulses without any external influences; conductivity - the ability of the elements of the conductive system to electrotonic transmission of excitation;
Excitability is the ability of cardiomyocytes to be excited in natural conditions under the influence of impulses transmitted along Purkin fibers.
An important feature of the excitability of the heart muscle is also a long refractory period, which guarantees the rhythmic nature of contractions.
doctor-v.ru
Features of the indicator assessment
The cardiac index allows you to choose the right treatment at different stages of shock and obtain more accurate diagnostic information.
It is important to keep in mind that this indicator is never self-assessed. It is included in the group of hemodynamic quantities as equivalent information together with:
- pressure in the arteries, veins, chambers of the heart;
- saturation of blood with oxygen;
- shock indices of the work of each ventricle;
- indicator of peripheral resistance;
- coefficients of oxygen delivery and utilization.
Features of age-related changes
With age, the minute volume of blood changes, on which the cardiac index depends. Due to the slowing of heart contractions, stroke volume increases (per contraction). So in a newborn baby it is at the level of 2.5 ml, at one year of age - 10.2 ml, and by the age of 16 it increases to 60 ml.
In an adult, this figure ranges from 60 to 80 ml.
The indicator is the same for boys and girls. But from the age of 11 it grows faster in boys, and by the age of 16 a slight difference is determined: in boys it is higher than in girls. But since weight and height (and therefore the total surface area of the body) simultaneously increase, the cardiac index does not increase, but even decreases by 40%.
Modern equipment does not require manual calculations, but produces a comprehensive analysis result. The specialist compares it with standard standards, compares it with other analytical data and judges the amount of compensatory possibilities or pathological changes.