In order to identify existing acquired or congenital pathological processes in the heart, the ultrasound method is often used. This diagnostic method has many advantages. Firstly, this manipulation is very informative and can reveal even minor changes in the structure of the heart and its blood flow. Secondly, it is not painful and does not cause moral or physical discomfort. For this reason, this procedure is available to everyone, regardless of age and gender.
In what cases is cardiac ultrasound prescribed?
Cardiologists usually prescribe this procedure if the patient has the following complaints:
- Irregular heart rhythm, fast, slow or uneven pulse;
- Pain in the chest area;
- The occurrence of shortness of breath even with minor physical exertion;
- Dizziness or loss of consciousness;
- Blue or pale skin, especially the nasolabial triangle;
- Suspicion of stroke or heart attack;
- Heart murmurs detected by the doctor;
- Diseases of the vascular system;
- Severe swelling of the limbs;
- Ever diagnosed tachycardia, arrhythmia, heart disease and dysfunction.
Ultrasound of the heart can be performed not only according to indications, but also for preventive purposes. Typically, examinations without obvious complaints are prescribed to professional athletes or people engaged in heavy physical labor. The study is also carried out before surgery on the heart or blood vessels.
Reasons for deviations
The heart is a muscle that works like a pump. Its main task is to pump blood. The weight of the heart depends on the volume of blood distilled. A child has a small heart - the capacity of the vascular bed is small, so there is little work for the heart. An adult, large man has a larger heart than a fragile girl, the reason for this is a different volume of blood. A weightlifter and an office worker have hearts of different masses. A weightlifter needs a big heart because his muscles consume more oxygen.
The weight of a healthy person’s heart depends on several factors and ranges from 270–380 grams in men and 203–302 in women.
Demographic factors for the development of cardiac hypertrophy include race, age, gender, physical activity, and a tendency toward obesity and alcoholism.
Deviation from these indicators is an alarm signal. The reason may be:
- hypertension;
- ischemic disease;
- congenital or acquired heart defects;
- obesity;
- great physical activity;
- bad habits.
An increase in the mass of the heart muscle also occurs in healthy people - professional athletes. As athletes age, they may be at risk for developing cardiovascular disease. Their coronary arteries cease to supply the hypertrophied muscle with a sufficient volume of blood, and against this background coronary disease will occur.
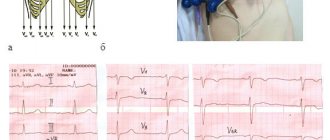
Hypertrophy can be assumed based on clinical data: shortness of breath, fatigue. Electrocardiography reveals characteristic changes. It is possible to diagnose the pathology and give an accurate quantitative assessment of the detected changes in myocardial hypertrophy using echocardiography and ultrasound examination.
Preparing for the study
Preparation measures may be different - it depends on how exactly the echocardiography will be performed. If you are undergoing a standard ultrasound examination procedure through the chest, then no special preparation is required - you just need to observe moderation in nutrition and fluid intake and relax. Experts do not recommend taking sedative medications before the study. Another method is transesophageal cardiac examination. In this case, more serious preparation is required. It is recommended to have dinner no later than 20:00 the day before, while in the morning before the examination you should not eat or drink. If the examination is scheduled for the evening, you are allowed to drink water in the morning.
Another effective way to identify pathological processes is a “stress echocardiogram”. This technique involves physical exercise to monitor the work of the heart under load. If you are having this test, you should not eat or drink three hours before the test.
How is an ultrasound of the heart performed?
First, let's look at the classic method of diagnosis through the skin in the area of the chest. First of all, it is important to dim the lights in the office so that the patient can calm down and relax. The person is asked to undress to the waist and remove jewelry from his neck, and then lie on his back on a flat couch. The specialist applies a small amount of silicone gel to the chest and begins the examination. If necessary, the doctor may ask you to change your body position, for example, lie on your side. The study usually takes 15-20 minutes. The doctor needs some more time to decipher and draw up the conclusion.
Modern medical centers also conduct other types of studies: stress echocardiography and transesophageal cardiography.
A transesophageal ECG is prescribed when the patient has an artificial heart valve. Also, indications for transesophageal examination are a recent stroke or the presence of atrial fibrillation. In this case, a thin “cord” with a camera at the end is inserted through the patient’s nose or mouth, after pre-treating the area with an anesthetic.
Stress echocardiography is performed while the patient is performing physical activity. At the time of the study, a person exercises on special exercise equipment or on a treadmill.
Ultrasound of the heart: what will the interpretation of the results show?
The diagnosis is carried out by an ultrasound doctor, who usually interprets the result.
During the examination, it is possible to diagnose the following ailments:
- Mitral valve prolapse;
- Presence of valve pathology;
- Deviations in the functioning of the heart muscle;
- Underdevelopment of the left ventricular myocardium;
- The exact dimensions and structure of the heart.
After issuing the results, the doctor must tell the patient about the existing diagnosis and further treatment tactics, if necessary.
Principle of determining mass
The determination of myocardial mass is calculated using numbers obtained during echocardiography. For accuracy and objectivity of measurement assessments, they are carried out in a combination of modes, comparing two- and three-dimensional images. The data is supplemented by the results of Doppler studies and indicators of ultrasound scanners, which are capable of displaying a projection of the heart in natural size on the monitor screen.
Calculation of myocardial mass can be done in several ways. Preference is given to two formulas ASE and PC, which use the following indicators:
- the thickness of the muscular septum separating the cardiac ventricles;
- directly the thickness of the posterior wall of the left chamber in a calm state, until the moment of its contraction;
- full size of the relaxed left ventricle.
The interpretation of values obtained from echocardiography should be considered by an experienced specialist in functional diagnostics. When evaluating the results, he will note that the ASE formula represents the left ventricle along with the endocardium (the cardiac membrane lining the chambers). This may cause distortion in the measurement of its thickness.
Normal ultrasound of the heart
If pathologies and abnormalities are not identified, the results should vary within the following limits:
- LV myocardial mass (left ventricle): men/women – 137–172 g/95–141 g, respectively;
- LV myocardial mass index: male – from 71 to 94 g/m2, female – from 71 to 89 g/m2;
- end diastolic size (EDS)/ESR (end systolic size): 46–57.1 mm/ 31–43 mm, respectively;
- LV wall thickness in relaxation (diastole) – up to 1.1 cm;
- blood ejection during contraction (FB) – 55–60%;
- the amount of blood pushed into the vessels - from 60 ml to 1/10 liter;
- Pancreas size index – from 0.75 to 1.25 cm/m2;
- pancreatic wall thickness – up to 0.5 cm;
- ECD of the pancreas: 0.95 cm–2.05 cm.
If the results of the study reveal any deviation in you, there is no need to worry at all. Not all changes threaten the patient’s quality of life. But even in the presence of diagnoses that pose a threat to life and health, qualified treatment will prevent the negative consequences of diseases and lead a rich and interesting life.
Electronic scientific journal Modern problems of science and education ISSN 2070-7428
1 Zadorozhnaya M.P.
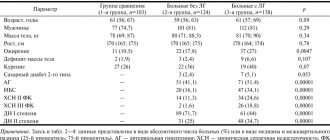
1Razumov V.V. 1 1 GBOU DPO NSIUV Ministry of Health of Russia The article highlights methodological and methodological problems when using the most common echocardiographic methods for calculating the mass of the left ventricular myocardium by linear dimensions in people with arterial hypertension, as well as various options for its indexing for the diagnosis of left ventricular myocardial hypertrophy, followed by there are numerous factors affecting the weight of the myocardium in different age groups. The article presents multiple criteria for hypertrophy of the left ventricular myocardium, even within the same indexing, which complicate the interpretation of the results obtained. A possible method for finding the optimal formula for calculating the mass of the left ventricular myocardium and its standardization is to study the relationships between the structural parameters of the left ventricle with its systolic, diastolic function and numerous indicators of structural functional restructuring of the vascular system in arterial hypertension. The arguments for using the Penn Convention method with standardization to body surface area are given. left ventricular myocardial mass index of left ventricular myocardial mass 1. Belenkov Yu.N., Ternovoy S.K., Sinitsyn V.E. Magnetic resonance imaging of the heart and blood vessels // Moscow, Vidar, 1997. 2. Prevention, diagnosis and treatment of primary arterial hypertension in the Russian Federation. The first Report of experts from the scientific society for the study of arterial hypertension of the All-Russian Scientific Society of Cardiologists and the Interdepartmental Council on Cardiovascular Diseases (DAG-I). Clinical Pharmacology and Therapy 2000; 3:5-30. 3. Rafikov A.Yu., Galyavich A.S. Comparative analysis of echocardiography (ECHO-CG) and multislice computed tomography (MSCT) data in assessing the functional parameters of the left ventricle in patients with hypertension. Kazan Medical Journal, 2012.-N 6.-P.855-858. 4. Recommendations for the treatment of arterial hypertension ESH/ESC 2013. Russian Journal of Cardiology. 2014; 1: 7-94. 5. Schmidt-Nielsen K. Animal sizes: why are they so important?: Per. from English – M.: Mir, 1987. – 259 p. 6. Abergel E., Tase M., Bohlader J. What definition for echocardiographic left ventricular hypertrophy? Am J Cardiol 1995;75:489-503. 7. Antoniucci D., Seccareccia F., Menotti A. et al. Prevalence and correlates of echocardiographic determined left ventricular hypertrophy in 2318 asymptomatic middle-aged men: the ECCIS project. Epidemiolgia e Clinica della Cardiopatia Ischemica Silente // J. Ital. Cardiology. – 1997. – Vol. 27, No. 4. – P. 363-369. 8. Burke GL, Arcilla RA, Culpepper WS, Wehber LS, Chiang YK, Berenson GS. Blood pressure and echocardiographic measures in children: the Bogalusa. Heart Study. Circulation 1987;75:10%14. 9. Casale PN, Devereux RB, Milner M. et al. Value of echocardiographic measurement of left ventriculsr mass in predicting cardiovascular morbid events in hypertensive men. Ann. Intern. Med. 1986; 105: 173-178. 10. Daniels SD, Meyer RA, Loggie LMH. Determinants of cardiac involvement in children and adolescents with essential hypertension. Circulation 1990;82:1243-8. 11. De Simone G, Devereux RB, Daniels SR, Koren MJ, Alderman MH, Laragh JH. Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and of their capacity to predict cardiovascular risk. J Am Coll Cardiol. 1995;25:1056-1062. 12. De Simone G, Devereux RB, Roman MJ, et al. Gender-differences in left ventricular anatomy, blood viscosity and volume regulatory hormones in normal adults. Am J Cardiol 1991;68:1704-8. 13. De Simone G., Devereux RB, Roman MJ et al. Relation of obesity and gender to left ventricular hypertrophy in normotensive and hypertensive adults // Hypertension. – 1994. – Vol. 23. – P. 600-606. 14. De Simone G1, Devereux RB, Kimball TR, Mureddu GF, Roman MJ, Contaldo F, Daniels SR. Interaction between body size and cardiac workload: influence on left ventricular mass during body growth and adulthood. Hypertension. 1998 May;31(5):1077-82. 15. De Simone G1, Verdecchia P, Pede S, Gorini M, Maggioni AP. Prognosis of inappropriate left ventricular mass in hypertension: the MAVI Study. Hypertension. 2002 Oct;40(4):470-6. 16. Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man: Anatomic validation of the method. Circulation 1977; 55: 613-618. 17. Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986. 57:450-458. 18. Gardin JM, Lauer MS. Left ventricular hypertrophy: the next treatable, silent killer? JAMA.2004;292:2396-2398. 19. Ghali JK, Liao Y, Simmons B et al. The prognostic role of left ventricular hypertrophy in patients with or without coronary artery disease // Ann. Intern. Med. – 1992. – Vol. 117. – P. 831-836. 20. Gidding SS. Controversies in the assessment of left ventricular mass. Hypertension. 2010 Jul;56(1):26-8. 21. Gosse P., Jullien V., Jarnier P. et al. Echocardiographic definition of left ventricular hypertrophy in the hypertensive: which method of indexation of left ventricular mass? // J. Hum. Hypertension. – 1999. – Vol. 13, No. 8. – P. 505-509. 22. Hammond IW, Devereux RB, Alderman MH et al. The prevalence and correlates of echocardiographic left ventricular hypertrophy among employed patients with uncomplicated hypertension // J. Amer. Coll. Cardiology. – 1986. – Vol. 7. – P. 639-650. 23. Hurst's heart / Eds. V. Fuster, R. W. Alexander, R. A. O'Rourke et al. – 10th ed. – 2001. – Vol. 1. – 1488 p. 24. Ilercil A, O'Grady MJ, Roman MJ, Paranicas M, Lee ET, Welty TK, et al. Reference values for echocardiographic measurements in urban and rural populations of differing ethnicity: the Strong Heart Study. J Am Soc Echocardiogr 2001; 14:601-11. 25. Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991 Mar 1;114(5):345-52. doi:10.7326/0003-4819-114-5-345. 26. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al. Recommendations for chamber quantification: A report from the American Society of echocardiography's Guidelines and Standards committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of echocardiography, a branch of the European Society of cardiology. J Am Soc Echocardiogr 2005;18:1440-63. 27. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA at al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006 Mar;7(2):79-108. 28. Levy D, Garrison RJ, Savage DD et al. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study // New Engl. J. Med. – 1990. – Vol. 322. – P. 1561-1566. 29. Levy D., Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP Echocardiographic criteria for left ventricular hypertrophy: the Framingham Heart Study. Am J Cardiol. 1987 Apr 15;59(9):956-60. 30. Liao Y., Cooper RS, Durazo-Arvizu R. et al. Prediction of mortality risk by different methods of indexation for left ventricular mass // J. Amer. Coll. Cardiology. – 1997. – Vol. 29, No. 3. – P. 641-647. 31. Linzbach AJ. Hypertrophy, hyperplasia and structural dilation of the human heart. Adv Cardiol 1976;18:1-14. 32. Mahn JJ, Dubey E., Brody A., Welch R., Zalenski R., Flack JM, Ference B., Levy PD Test characteristics of electrocardiography for detection of left ventricular hypertrophy in asymptomatic emergency department patients with hypertension. Acad Emerg Med. 2014 Sep;21(9):996-1002. doi: 10.1111/acem.12462. 33. Mahoney LT, Schieken RM, Clarke WR, Lauer RM. Left ventricular mass and exercise responses predict future bkmd pressure. Hypertension 1988112:206-13. 34. Mureddu GF, Pasanisi F, Palmieri V, Celentano A, Contaldo F, de Simone G. Appropriate or inappropriate left ventricular mass in the presence or absence of prognostically adverse left ventricular hypertrophy. J Hypertens. 2001; 19: 1113-1119. 35. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents.Pediatrics.2004;114:555-576. 36. Schiller NB, Shah PM, Crawford M. et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography committee on standards, subcommittee on quantitation of two-dimensional echocardiograms // J. Amer. Soc. Echocardiography. – 1989. -Vol. 2. – P. 358-367. 37. Troy BL, Pombo J., Rackley CEMeasurement of left ventricular wall thickness and mass by echocardiography // Circulation. 1972. Vol. 45. P. 602-611. 38. Verhaaren HA, Schieken RM, Mosteller M, Hewitt JK, Eaves LJ, Nanee WE. Bivariate genetic analysis of left ventricular mass and weight in pubertal twins (the Medical College of Virginia Twin study). Am J Cardiol 199l;68:661-8.11-14.
Left ventricular myocardial hypertrophy (LVH), as an element of its structural restructuring, is considered a sign of morphological deviation from the norm, a clear predictor of an unfavorable prognosis of the disease that caused it , as well as a criterion determining the choice of active treatment tactics [28]. Over the past twenty years, clinical studies have been conducted that have proven the independent contribution of drug-induced reduction in LV myocardial mass (LVMM) in patients with arterial hypertension (AH), which makes it necessary to determine and control LVMM [18]. Based on these ideas, recent recommendations for the diagnosis and treatment of hypertension include the measurement of LVMM in the algorithm of antihypertensive management of patients in order to determine the presence of LVH [4, 35].
But still, there is no unambiguous idea about the pathogenicity of LVH, which is associated with interrelated problems of both methodological and methodological nature: The first concerns the reliability of methods for determining LVH, the second concerns the assessment of the results obtained in terms of the presence or absence of LVH. In addition, there are many instrumental approaches to determining LVMM.
When measuring LVMM, researchers are faced with multifactorial factors that do not influence it. This is the dependence of LVMM on body size, and the possibility of only an adaptive increase in LVMM, for example, during physical activity. There is also a difference in the sensitivity of instrumental methods for determining LVMM: some authors are inclined towards greater sensitivity of MRI measurements [1, 3].
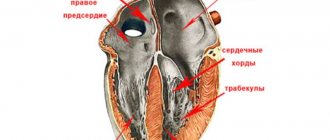
All echocardiographic calculations of LVMM, based on determining the difference in LV volumes between the epicardium and endocardium, multiplied by myocardial density, face the problems of determining tissue interfaces and assessing the shape of the left ventricle.
Moreover, many methods are based on linear measurements in M-mode under B-mode control, or directly in a two-dimensional image [24].
The previously existing problem of identifying tissue interfaces, such as “pericardium-epicardium” and “blood-endocardium”, has generally been resolved in recent years, but requires a critical attitude to the studies of past years and does not relieve researchers from the need to use all the technical capabilities of ultrasound -scanners.
Individual differences in LV geometry prevent the creation of a universal mathematical model, even in the absence of local disturbances in the structure of the LV and the approximation of its shape to an ellipse, which has generated a large number of formulas, and, consequently, criteria for determining LVH, resulting in different conclusions about the presence of hypertrophy in one and the same person. the same patient.
In addition, several calculation formulas for determining LVMM are currently used.
The formulas recommended by the American Society of Echocardiography (ASE) and the Penn Convention (PC) are more often used, using three measured parameters: the thickness of the myocardium of the interventricular septum (IVS), the posterior wall of the LV (PLV) at the end of diastole and its end-diastolic size (EDD) with including (ASE formula) or not including endocardial thickness (PC formula) in left ventricular diameter, depending on the formula used. But the results obtained when applying these formulas are not always comparable, therefore, to interpret the data obtained, it is necessary to clarify the method used for calculating the parameters of the left ventricle, which in practice is not always available or is neglected. The reason for the discrepancy lies in the following. The cubic formula, originally recommended by ASE, was proposed by BL Troy et al in 1972 (LVMM, gr = [(EDV+LVAD+LVAD)3-EDV3]×1.05) [37] and then modified using the regression equation RB Devereux and Reichek in 1977 (Penn Convention formula) by analyzing the relationship between echocardiographic LVMM and postmortem anatomical LV mass in 34 adults (r = 0.96, p
Source: https://science-education.ru/ru/article/view?id=23603