Are clinical manifestations of impaired contractility possible?
Changes in myocardial contractility are not isolated, and, as a rule, are accompanied by one or another myocardial pathology. Therefore, among the patient’s clinical symptoms, those that are characteristic of a specific pathology are noted. Thus, with acute myocardial infarction, intense pain in the heart region is observed, with myocarditis and cardiosclerosis - shortness of breath, and with increasing systolic dysfunction of the LV - edema. Heart rhythm disturbances (usually atrial fibrillation and ventricular extrasystole) are common, as well as syncope (fainting) conditions caused by low cardiac output and, as a consequence, low blood flow to the brain.
Myocardial contractility according to ECG
The contractility of the heart muscle can be assessed already by performing an electrocardiogram (ECG), since this research method allows you to record the electrical activity of the myocardium. With normal contractility, the heart rhythm on the cardiogram is sinus and regular, and the complexes reflecting contractions of the atria and ventricles (PQRST) have the correct appearance, without changes in individual teeth. The nature of the PQRST complexes in different leads (standard or chest) is also assessed, and with changes in different leads, one can judge the impairment of contractility of the corresponding sections of the left ventricle (lower wall, high-lateral sections, anterior, septal, apical-lateral walls of the LV). Due to its high information content and ease of use, an ECG is a routine research method that allows timely identification of certain disorders in the contractility of the heart muscle.
Do contractility disorders need to be treated?
Treatment of impaired contractility of the heart muscle is mandatory. However, when diagnosing such a condition, it is necessary to establish the cause that led to impaired contractility and treat this disease. Against the background of timely, adequate treatment of the causative disease, myocardial contractility returns to normal levels. For example, in the treatment of acute myocardial infarction, areas subject to akinesia or hypokinesia begin to normally perform their contractile function 4-6 weeks after the onset of the infarction.
How to determine reduced myocardial contractility
In order to be able to obtain maximum information about the state of your health, you need to undergo a full examination. Typically, reduced or satisfactory myocardial contractility is detected after ECG and echocardiography. If the results of the electrocardiogram make you think and do not allow you to immediately make an accurate diagnosis, the person is recommended to undergo Holter monitoring. It consists of continuously recording heart performance using a portable electrocardiograph attached to clothing. This way you can get a more accurate picture of your health status and make a final conclusion.
Phase structure of the cardiac cycle
This direction of shift depends on an increase in the phase of isometric contraction (the phase of increasing intraventricular pressure), while the phase of asynchronous contraction (transformation) does not change significantly with age. This is especially clearly seen from the calculation of the intrasystolic indicator of the phase of isometric contraction.
The ejection period in people aged 60 years is most often shortened, which should be made dependent on the decrease in cardiac output usually observed at this age. This reveals an increase in the phase of rapid expulsion of blood and a shortening of the phase of slow expulsion.
This redistribution in the phase structure—an extension of the rapid ejection phase—can be associated with a decrease in myocardial contractility in the presence of increased peripheral vascular resistance. The lengthening of the fast ejection phase and the shortening of the slow phase are also confirmed when recording a rheogram and electrokymogram from the ascending aorta and its arch.
Calculation of the ratio of the ejection period to the tension period (Blumberger coefficient) indicates that the work expended directly on the ejection of blood from the left ventricle during systole requires greater myocardial tension and is performed over a longer period of time.
It should be considered that prolongation of both electrical and mechanical systole of the heart is the most beneficial restructuring of cardiac activity, which ensures hemodynamics in specific conditions.
The diastolic period of the cardiac cycle also undergoes age-related restructuring—the period of isometric relaxation and the rapid filling phase are lengthened with a relative shortening of the overall filling period.
Myocardial contractility
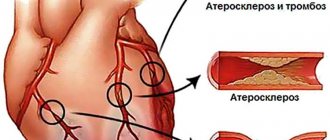
Progressive myocardial sclerosis, focal atrophy of muscle fibers with symptoms of protein-lipoid degeneration, nested hypertrophy of muscle fibers, dilatation of the heart are the main morphological signs of the senile heart.
One of the main reasons for the development of dystrophic and atrophic changes in the myocardium during aging is disruption of energy processes and the development of hypoxia.
With aging, the intensity of tissue respiration of the myocardium decreases, the coupling of oxidation and phosphorylation changes, the number of mitochondria decreases, their degradation occurs, the activity of individual parts of the respiratory chain changes unevenly, the glycogen content decreases, the concentration of lactic acid increases, the intensity of glycolysis is activated, the amount of ATP and CP decreases. creatine phosphokinase (CPK) activity
.
It is known that myocardial contractility is controlled by many mechanisms, the most important of which are the Frank-Starling mechanism and direct inotropism, which is closely related to the adrenergic effect on the heart. At the same time, it has been shown that the Frank-Starling mechanism suffers significantly with age.
This is due to a decrease in the elasticity of muscle fibrils as such, an increase in low-elastic connective tissue, the appearance of atrophic changes and hypertrophy of individual muscle fibers, as well as changes within the actomyosin complex itself.
It should also be noted that there is a violation of the properties of myocardial contractile proteins and a change in the actomyosin complex. Bing (1965) believes that the aging heart gradually loses the ability to convert the energy received during its formation into mechanical work.
The author has established a decrease in the contractile ability of actomyosin filaments in old people. In addition, it was noted that the amount of myofibrillar proteins decreases with age. Undoubtedly, all these changes can be the cause of functional failure of the myocardium.
Dock (1956) sees disturbances in mineral metabolism, in particular excessive accumulation of Na+ ions, as one of the reasons for impaired myocardial contractility in old age. According to Burger (Burger, 1960), with age, the content of water, K+ and Ca2+ ions in the heart muscle decreases. Michel (1964) points out that changes in the chemical environment (transmineralization, reduction in energy-rich phosphates) occur in parallel with a limitation of myocardial contractility and its compensatory ability.
It has been shown that with age, the content of intracellular Na+ ion increases, and the content of K+ ion decreases. The AP repolarization phase is lengthened. It is known that the depolarization wave, propagating along the outer membrane of the muscle cell, also captures the T-tubular system and penetrates the elements of the sarcoplasmic reticulum (SRR)
, which causes the release of calcium from the SPR tanks.
The calcium “volley” leads to an increase in the concentration of the Ca2+ ion in the sarcoplasm, as a result of which the Ca2+ ion enters the myofibrils and binds there with the Ca2+ reactive protein troponin. Due to the elimination of tropomyosin repression, the interaction of actin and myosin occurs, i.e., contraction.
The onset of subsequent relaxation is determined by the rate of reverse transport of the Ca2+ ion into the SPR, which is carried out by the Ga-Mg-dependent ATPase transport system and requires a certain energy expenditure. Changes in the K+/Na+ ratio can affect the state of the potassium-sodium pump.
It can be assumed that the resulting changes in the K+/Na+ ratio and disturbances in the calcium pump can significantly impair myocardial contractility and diastolic relaxation of the heart in old age.
In addition, in old animals, changes were also revealed in the SPR - thickening and compaction of the T-carpal system, a decrease in their specific gravity in the cell, an increase in contacts between the sarcolemma and the vesicles of the SPR, which, as is known, provide the optimal rate of exit and entry of the Ca2+ ion into SPR. Under these conditions, the optimal possibilities for systole and diastole are disrupted, especially with functional stress.
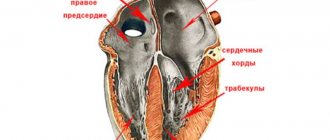
As is known, synchronization of the activity of individual muscle cells is essential in ensuring the contractility of the heart. It is largely determined by the state of the intercalary discs, i.e., the place of contact of individual myocardial cells. At the same time, in an experiment on old animals (Frolkis et al., 1977b), when a load was applied, a distinct widening of these discs was found, with a 3-4-fold increase in the distance between them.
Bioelectrical basis of myocardial contractility
heart contraction cycle
The contractility of the entire myocardium depends on the biochemical characteristics in each individual muscle fiber. The cardiomyocyte, like any cell, has a membrane and internal structures, mainly consisting of contractile proteins. These proteins (actin and myosin) can contract, but only if calcium ions enter the cell through the membrane. This is followed by a cascade of biochemical reactions, and as a result, the protein molecules in the cell contract like springs, causing contraction of the cardiomyocyte itself. In turn, the entry of calcium into the cell through special ion channels is possible only in the case of repolarization and depolarization processes, that is, sodium and potassium ion currents through the membrane.
With each incoming electrical impulse, the cardiomyocyte membrane is excited, and the flow of ions into and out of the cell is activated. Such bioelectric processes in the myocardium do not occur simultaneously in all parts of the heart, but one by one - first the atria are excited and contracted, then the ventricles themselves and the interventricular septum. The result of all processes is a synchronous, regular contraction of the heart with the ejection of a certain volume of blood into the aorta and further throughout the body. Thus, the myocardium performs its contractile function.
Video: more about the biochemistry of myocardial contractility
How is reduced contractility treated?
First of all, the patient is limited in emotional and physical stress. They provoke an increase in the heart's need for oxygen and nutrients, but if the global contractility of the left ventricular myocardium is impaired, the heart will not be able to perform its function, and the risk of complications will increase. It is imperative to prescribe drug therapy, which consists of vitamin preparations and agents that improve metabolic processes in the heart muscle and support the performance of the heart. The following medications will help cope with satisfactory contractility of the left ventricular myocardium:
- phosphocreatine;
- riboxin;
- panangin or asparkam;
- iron supplements;
- royal jelly.
Note! If the patient cannot independently protect himself from stressful situations, he will be prescribed sedatives. The simplest ones are tincture of valerian and motherwort.
If the cause of the disorders is a heart or vascular disease, it will be treated first. Only then, after repeated diagnostics and electrocardiography, will a conclusion be made about the success of therapy.
What is normokinesis of myocardial contractility?
When a doctor examines a patient’s heart, he necessarily compares the proper performance indicators (normokinesis) and the data obtained after diagnosis. If you are interested in the question of determining normokinesis of myocardial contractility, only a doctor can explain what it is. We are not talking about a constant figure, which is considered the norm, but about the relationship between the patient’s condition (physical, emotional) and the indicators of the contractility of the heart muscle at the moment.
After identifying the disorders, the task will be to identify the cause of their occurrence, after which we can talk about successful treatment that can bring the working parameters of the heart back to normal.