What is akinesia?
The term akinesia refers to the inability to perform clinically perceptible movements. The disease can manifest itself as a delayed reaction, stopping of movement or even complete cessation of movement. Akinesia occurs when movement is not felt, either because the range of movement is small or because the time required to initiate a response is significantly increased. The former is often a consequence of severe bradykinesia, which is often mistakenly called akinesia. This makes it difficult to distinguish between them. With akinesia, sufficient force does not quickly accumulate to initiate movement.
Akinetic states are associated with numerous etiological causes, which depend on the age of the patient. In adults, akinesia can occur on its own or as a consequence of neurodegenerative disorders. Akinesia detected in the antenatal or neonatal period is associated with fetal akinetic syndrome.
Causes
The causes of akinesia can be classified depending on the age group.
1. In adults, akinesia is associated with the following two reasons:
- Pure isolated akinesia (without any accompanying conditions).
- Late stages of basal ganglia or frontal lobe diseases: Progressive supranuclear palsy (PSP or also known as Steele-Richardson-Olszewski syndrome);
- Parkinson's disease (PD);
- Multiple system atrophy (MSA);
- Normal pressure hydrocephalus (NPH).
2. Fetal akinetic syndrome (arthrogryposis fetalis or Pena-Choqueir syndrome type 1) is a cause of intrauterine fetal death or, in rare cases, live birth associated with diffuse contractures throughout the body (arthrogryposis) of the fetus and, consequently, with decreased mobility, which further leads to intrauterine growth retardation, short umbilical cord and pulmonary hypoplasia.
Symptoms
An infarction of the anterior wall of the heart (as well as another localization) is accompanied by the appearance of characteristic clinical signs that allow one to immediately suspect the disease.
Typical signs
When talking with patients suffering from hypertension or other heart diseases, I always pay attention to signs that may indicate the onset of acute infarction of the anterior wall of the left ventricle:
- Burning, pressing pain in the region of the heart. Many of my patients have described the symptom as “being squeezed in a vice” or “an elephant stepping on the chest.” A feature of a heart attack is the irradiation (spread) of pain to the left arm, neck, jaw or under the shoulder blade.
- The duration of the attack may exceed 30 minutes.
- Ineffectiveness of the tablets used. My patients always keep antihypertensive medications at home, Nitroglycerin and Validol. In case of a heart attack, these drugs will not bring relief.
Most of my patients can clearly indicate the moment of pain. The attack is often associated with a stressful situation or excessive physical activity. However, in my practice there have often been patients in whom a heart attack developed in the absence of any provoking factors.
Atypical manifestations
The clinical picture described above remains classic. It is characteristic mainly of anterior infarction. However, plaque rupture with thrombosis can also occur in arteries that supply blood to other parts of the heart.
In case of myocardial infarction of the inferior wall of the left ventricle, the following atypical signs come to the fore:
- Nausea, vomiting. One patient told me how he ate a heavy meal and his abdominal discomfort suddenly began to increase. Before seeking help, he took 4 tablets of drugs to improve digestion. The ambulance team diagnosed an inferior infarction.
- Isolated shortness of breath with a tendency to increase the intensity of the symptom. In this case we are talking about a disease.
- Weakness with episodes of dizziness. Patients lose consciousness extremely rarely.
- Painless form of ischemia. A relatively rare variant of the development of the disease. The patient may only notice weakness and a desire to rest.
I always tell my patients that if at least one of the symptoms described above occurs, they should consult a specialist. It is quite easy to miss a heart attack that develops in the lower wall of the left ventricle. However, it is not easy to treat it after losing precious time.
Epidemiology
Akinesia in clinically observed parkinsonism has been found to be more often associated with the motor variant of frontotemporal dementia (FTD) than with frontal degeneration associated with Parkinson's disease (PD). About 30% of patients with clinically confirmed FTD had signs of parkinsonism, such as rigidity or akinesia. Acute akinesia is a relatively rare phenomenon and occurs in 0.3% of patients with PD secondary to infectious pathology or other stress factors.
In pediatrics, akinesia is often associated with fetal akinetic syndrome. This is associated with high intrauterine mortality. However, the incidence of live births is 1 in 3000 cases, with more than 320 genes involved. The condition is more common among Asian, European and African populations.
Pathophysiology
The pathogenesis of akinesia in adults in general appears to be related to pallidonigral degeneration, which mainly results in stiffening. However, the specific pathology depends on the type of akinesia. In cases of pure akinesia with freezing of gait without any other symptoms or diagnosis of PD, it is most likely due to progressive supranuclear palsy (PSP). In PSP, degeneration of the subthalamic nuclei, globus pallidus, and substantia nigra is observed.
In patients with Parkinson's disease, the main cause of akinesia appears to be dysfunction of the phasic and tonic release of dopamine. This contrasts with resting tremor, which is caused primarily by dysfunctional tonic phase dopamine release. Another theory suggests that akinesia in patients with Parkinson's disease is associated with bilateral frontal lesions and is also accompanied by worsening mental status.
Fetal akinesia is associated with approximately 320 genetic variations that may be present in this syndrome. From a pathological point of view, pathology occurs at all levels, including the brain, spinal cord, motor neuron, neuromuscular junction, and muscles.
Causes, risk factors and development mechanism
To begin with, I will try to briefly outline the essence of the problem.
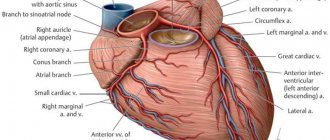
Acute myocardial infarction is one of the variants of coronary heart disease (CHD). The basis of the pathology remains a critical discrepancy between the needs of the heart muscle for oxygen and nutrients. Simply put, certain areas of the myocardium are simply not supplied with blood, which leads to the death of first isolated cells (cardiomyocytes), and then entire areas of muscle tissue. My patients often ask me what can happen to cause the vessel that supplies the heart with blood to close. In 70-80% of cases, the basis of the problem is atherosclerosis. The disease is accompanied by the deposition of fat on the surface of the vascular wall and inflammation of the cells of its inner layer. Over time, these elements form a tubercle, after which the lumen of the artery narrows. The result may be plaque rupture with the formation of a blood clot and complete blockage of the vessel. Acute myocardial infarction of the anterior wall of the left ventricle occurs in my practice more often than other forms. This is due to the anatomical features of the blood supply to the heart.
According to modern views of cardiologists on the causes of myocardial infarction, it is worth highlighting the following key factors contributing to the progression of the pathology:
- Poor nutrition. I mean excessive consumption of foods rich in fast carbohydrates and fats (fast food, various sweets, energy drinks, alcohol).
- Obesity. Excess body weight indicates an active process of fat deposition in the wall of blood vessels. You can determine your body mass index by clicking on the link.
- Smoking. Nicotine promotes additional spasm of the coronary arteries.
- Physical inactivity. The less you move, the higher the chance of developing obesity with further progression of atherosclerosis.
- High blood pressure (BP). The chance of developing anterior, lateral or inferior myocardial infarction in hypertensive patients is higher than in patients with normal blood pressure.
- Stress. Emotional stress leads to vasospasm, which, given the presence of plaques, increases the risk of their rupture with the development of acute thrombosis and artery blockage.
- Age, gender Men over 50 occupy a leading place among patients with heart attacks of various locations.
Genetic predisposition also plays a role in the development of the disease. If you have close relatives who have suffered or died from a heart attack, you should be more attentive to risk factors and visit the doctor more often.
Diagnostics
— History and physics.
In Parkinson's disease (PD), evaluation of a patient with akinesia reveals freezing mid-movement, festination of both gait and speech, and repetitive movements of the upper extremities. This stiffening is usually associated with increased symptoms when passing through narrow spaces such as doorways. The condition is usually not treatable with antiparkinsonian drugs.
In akinetic patients secondary to PSP, the stiffness is primarily axial rather than appendicular. The earliest manifestation is intermittent falls due to severe rigidity, but atypical manifestations such as nonspecific dizziness, generalized motor slowing, and personality changes may also be present. Slowing of vertical saccades is the most common manifestation of eye movements, along with difficulty in looking down.
During the prenatal period, a patient carrying a fetus with possible fetal akinesia may experience decreased fetal motility. In later stages of pregnancy, the patient develops polyhydramnios, as evidenced by an abnormally increased height of the uterine fundus.
When a baby is born alive with fetal akinesia syndrome due to lack of fetal movement, the following sequence is often observed:
- fetal joint contractures;
- pulmonary hypoplasia;
- polyhydramnios;
- micrognathia.
— Analyzes and visualization.
The definition of akinesia in a patient is primarily clinical and is characterized by a delay or inability to respond or execute a motor command. Reaction time analysis is used to assess the degree of akinesia. Typically the study shows delayed simple reaction time but normal choice reaction time.
Neuroimaging studies used to evaluate akinesia include:
- magnetic resonance imaging (MRI);
- functional MRI;
- single photon emission computed tomography;
- positron emission tomography.
Treatment
Treatment of akinesia in adults comes down to monitoring the development of the underlying disease. Treatment of akinesia is symptomatic rather than curative.
- Drug therapy: In patients with Parkinson's disease (PD), it mainly aims to modify/supplement the impaired dopamine release.
- Surgical therapy: The most studied surgical procedure to treat akinesia is deep brain stimulation, commonly used to improve dopamine secretion and improve symptoms of tremor, akinesia, and rigidity.
- Other procedures performed in severe cases include thalamotomy, pallidotomy, nerve grafts, and electrical stimulation.
Treatment of fetal akinesia is supportive, mainly due to the dismal prognosis for live birth. Initially, resuscitation measures are used to combat pulmonary hypoplasia. First, drugs such as sildenafil and iloprost are used to control high pressure in the lungs. Antimicrobials may be required. These patients often require prolonged feeding due to intestinal malrotation, short bowel syndrome, and dysphagia. Central nervous system abnormalities such as epilepsy and endocrine disorders such as hypothyroidism require treatment with anticonvulsants and thyroid hormone replacement therapy.
Clinical case
A 49-year-old man was admitted to our clinic with severe pressing pain behind the sternum, which radiated to the left arm.
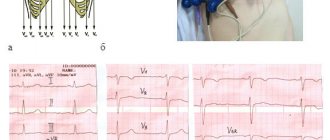
The patient attributes the symptoms to stress due to a quarrel with his wife. It took 2 hours from the moment the symptom appeared to seeking help. On the cardiogram, ST segment elevation in V1-V4 and the formation of a pathological Q wave in I, aVL, V1-V4. During bedside echo-CG, no zones of hypokinesia were identified. The troponin test is positive. Blood pressure – 130/90 mm Hg. Art. The patient was sent for urgent coronary angiography. Total occlusion of the anterior descending branch of the left coronary artery was discovered. Stenting was performed with the placement of a metal stent. As a result, a diagnosis was made: anteroseptal myocardial infarction. On the third day after stenting and taking appropriate drug therapy, the patient notes an almost complete normalization of his condition.
Forecast
There is no curative therapy for adult akinesia, but symptomatic treatment can significantly reverse the damage to quality of life in these patients. Although mild akinesia may not directly lead to death, severe akinetic crises can cause dysphagia, autonomic dysfunction, and aspiration, which can be fatal.
Fetal akinesia syndrome has been found to be fatal in the womb, with 30% of fetuses being stillborn. The final prognosis depends on the underlying cause. Most live-born babies usually die within the first month of life. This may provide a basis for proposing late termination of pregnancy in countries where this is permitted.
Complications
Fetal akinesia is often fatal within the first month of life. This is due to the many complications associated with this condition.
- Pulmonary complications: pulmonary hypoplasia, pulmonary hypertension, aspiration pneumonia.
- Oropharyngeal dysfunction: This leads to aspiration and subsequent pneumonia.
- Neurological complications: epilepsy and hypothalamic dysfunction.
- Gastrointestinal complications: short bowel syndrome and intestinal malrotation.
- Endocrine dysfunction: hypothyroidism resulting from hypothalamic dysfunction.
Akinesia in adults can often manifest as a critical situation, known as an akinetic crisis. Parkinsonian hyperpyrexia, neuroleptic malignant syndrome, and acute akinesia of parkinsonism are other terms used to describe these akinetic crises. The spectrum of this variant can range from complete akinesia with dysphagia, hyperthermia, dysautonomia, increased muscle enzymes, and mental status changes to inability or difficulty initiating movement.
Consequences and possible complications
The prognosis for a patient with a heart attack always depends on timely consultation with a doctor. When providing qualified assistance to the patient within the first 2 hours after the onset of the attack, it is likely to prevent the development of necrosis of the heart muscle. A similar prognosis is possible thanks to rapid thrombolysis and stenting. However, people often endure pain and hope that it will “go away on its own,” thereby wasting precious minutes and increasing the affected area.
The most common complications of the disease that I often encounter:
- Deterioration of the contractile function of the heart with the development of failure.
- Various types of rhythm and conduction disorders.
- Chronic cardiac aneurysm. Due to the thinning of the affected myocardium, a protrusion forms in the wall, in which blood clots can form.
The most severe consequence of a heart attack is death. However, with adequate therapy and a successful combination of circumstances, patients can live well for decades even after suffering a heart attack. You can read about what medications and for how long to take after discharge from the hospital.