Heart failure, like all diseases of the cardiovascular system, is one of the most dangerous, i.e. those that lead to particularly severe consequences (disability, death). For the development of any pathology in the myocardium, there is a reason, and one of them is systolic disorders - a decrease in the ability of the heart to eject blood into the aorta (this leads to the development of left ventricular failure and pulmonary hypertension). As a result, such operational problems reduce the overall level of release and delivery of oxygen and nutrients through the blood to vital organs.
Diastolic myocardial dysfunction - what does it mean?
Dysfunction is a malfunction of the organ, translated from Latin as “difficulty in action”, diastolic dysfunction of the myocardium, respectively, this is a disruption of the process of the heart muscle and a decrease in the filling of the left ventricle with blood during diastole (its relaxation). With this pathological process, the ability of the left chamber of the myocardium to pump blood into its cavity from the pulmonary artery decreases, thus reducing its filling during relaxation.
Diastolic dysfunction of the left ventricular myocardium is manifested by an increase in the ratio of final ventricular pressure and final volume during diastole. The development of this pathology is accompanied by a decrease in the compliance of the walls of the left chamber of the heart.
Fact! In 40% of patients with heart failure, there is no systolic dysfunction of the left chamber, and acute heart failure is progressive diastolic dysfunction of the left ventricle.
I want to know the cost of treatment
As the left ventricle fills, there are three main stages of the process.
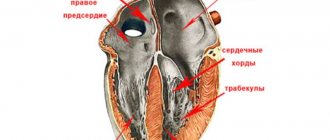
- Relaxation. This is a period of relaxation of the heart muscle, during which the active removal of calcium ions from filamentous muscle fibers (actin, myosin) occurs. During this, the contracted muscle cells of the myocardium relax and their length increases.
- Passive filling. This stage occurs immediately after relaxation; the process directly depends on the compliance of the walls of the ventricle.
- Filling, which is carried out due to contraction of the atria.
Interesting! Despite the fact that cardiovascular diseases more often affect males, this dysfunction, on the contrary, “prefers” women a little more. Age category – from 60 years.
How is functional impairment treated?
As already noted, left ventricular diastolic dysfunction, the treatment of which depends on the type of disease, primarily affects hemodynamic processes. Therefore, the treatment plan is based on correcting disturbances in this process. In particular, regular monitoring of blood pressure, heart rate and water-salt metabolism is carried out, followed by their correction, as well as remodeling of myocardial geometry (reducing thickening and returning the walls of its chambers to normal).
Among the drugs that are used to treat functional disorders of diastole in this part of the heart, the following groups are distinguished:
- adrenergic blockers;
- drugs to improve the elasticity of the heart muscle, reduce pressure, reduce preload and promote myocardial remodeling (sartans and ACE inhibitors);
- diuretics (diuretics);
- drugs that reduce calcium levels in heart cells.
Varieties of this pathology
Today, this pathology is usually divided into the following types:
- diastolic myocardial dysfunction type 1. This stage is characterized by disturbances (slowdowns) in the process of relaxation of the left ventricle of the heart in diastole. The required amount of blood at this stage arrives during atrial contractions;
- diastolic myocardial dysfunction type 2 is characterized by an increase in pressure in the left atrium, due to which filling of the lower chamber is possible only due to the action of a pressure gradient (this type is called “pseudonormal”);
- diastolic myocardial dysfunction type 3. This stage is associated with an increase in atrial pressure, a decrease in the elasticity of the ventricular walls and an increase in rigidity.
Sign up for a consultation
Depending on the severity of the pathology, an additional division has been adopted into:
- mild (type I disease);
- moderate (type II disease);
- severe reversible and irreversible (type III disease).
Materials and methods
The study included 365 people (198 men) aged from 30 to 85 years (mean age 64.6±8.0 years) who underwent echocardiographic examination in an ultrasound diagnostic room. The study included persons without pathologies of the cardiovascular system and respiratory organs (group 1, or comparison group, n
=103), patients with respiratory pathology without signs of PH (group 2,
n
=124) and patients with echocardiographic signs of PH (group 3,
n
=138).
The criterion for the presence of PH was considered to be a mean pulmonary artery pressure (MPAP) above 25 mm Hg. Participants in group 1 were recruited from persons without complaints and a history of diseases of the cardiovascular system and lungs. These patients underwent a preventive examination in the ultrasound room to exclude pathologies of the abdominal organs, urinary system or reproductive organs; they additionally underwent echocardiography (EchoCG) and electrocardiography after obtaining consent. Groups 2 and 3 included patients with various chronic diseases of the bronchopulmonary system: chronic obstructive pulmonary disease - COPD ( n
= 76), chronic dust bronchitis (
n
= 143), anthracosilicosis (
n
= 25), other pneumoconiosis (
n
=11).
In 21 people from group 3, PH developed against the background of pathology of the cardiovascular system: pulmonary embolism - PA ( n
= 1), coronary heart disease - IHD (
n
= 7), hypertension (
n
= 3), a combination of IHD and hypertension (
n
=12). The groups are comparable in age and gender composition (Table 1). The study did not include patients with decompensation of the underlying or concomitant disease, hemodynamically significant heart defects, renal and liver failure, type 1 diabetes mellitus, thyrotoxicosis, or cancer.
Table 1. Characteristics of the studied groups Note.
Here is the table. 2-4: Data are presented as the absolute number of patients (%) or as the median and interquartile range (25th percentile; 75th percentile). AG - arterial hypertension; CHF - chronic heart failure; FC - functional class; DN—respiratory failure. Patients were assessed for their clinical condition, electrocardiogram and spirometry parameters were recorded. EchoCG was performed using MedisonSonace 8000 and VividS5 ultrasound systems; structural parameters were assessed: the length and area of the RV in diastole and systole in a four-chamber section from the apical approach, the end-diastolic length and the diameter of the right atrium (RA). Tricuspid annular systolic excursion (TAPSE) was determined in M-mode in a four-chamber section. RV ejection fraction (EF) was determined using the Kaul method (RVEF=3.2·TAPSE) [11]. In Doppler mode, we studied the parameters of transtricuspid blood flow: peak velocity of early diastolic flow (Et), atrial systole flow (At), their ratio (Et/At), and deceleration time of early diastolic flow (B3Et).
Patients underwent pulsed wave tissue Doppler, during which the velocities of systolic (s't), early (e't) and late diastolic motion of the pancreatic wall in the area of the tricuspid valve annulus were measured. The e't/a't ratio in the indicated segment was also measured. Using pulsed wave tissue Doppler, the Thea index was determined as the ratio of the sums of isovolumetric relaxation time and isometric filling time of the pancreas to the time of pancreatic ejection [2].
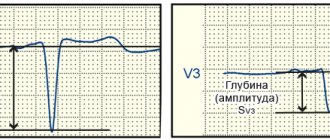
SRTP was measured in combined color M-mode. In this study, the M-line was installed in the area of opening of the cusps of the mitral and tricuspid valves, and at least 5 cycles were recorded in color M-mode. The velocity of propagation of atrioventricular flow was determined by measuring the slope of the early diastolic wave of the color Doppler spectrum. LBP was measured using the Kitabataki method: the ratio of acceleration time to ejection time in the outflow tract of the pancreas was assessed. In the presence of tricuspid regurgitation, the pressure gradient between the RV and the right atrium (RVRA) was measured, on the basis of which the systolic pressure in the PA (SPAP) was calculated.
The work was carried out in accordance with the Declaration of Helsinki, the study protocol was approved by the local ethics committee, all patients signed voluntary informed consent to participate in it.
Statistical data processing was carried out using the standard software package Statistica 6.0. Normality of distribution was determined using the Shapiro-Wilk test. For most quantitative variables, the distribution differed from normal; they are presented as median and interquartile range. Comparisons were made using the Kruskal-Wallace test and subsequent identification of between-group differences using the Mann-Whitney test with Bonferroni correction. The relationship between diastolic function parameters and echocardiographic signs of PH was assessed using the Spearman correlation coefficient. The association of possible factors with a decrease in CPTP less than 32 cm/s was assessed in a multiple logistic regression model. Variables for which the criterion for statistical significance in univariate analysis was less than 0.1 were included in the multivariate analysis. Multivariate analysis was performed stepwise by exclusion method. Initially, the sign most closely associated with a decrease in SRTP was identified. Subsequent variables were included in the logistic regression model when the contribution was significant at the α≤0.1 level. Level of statistical significance ( p
) is taken equal to 0.05.
The main symptoms of external manifestations of dysfunction
Diastolic myocardial dysfunction quite often occurs asymptomatically, without revealing its presence for years. If pathology manifests itself, then you should pay attention to the appearance of:
- heart rhythm disturbances;
- shortness of breath, which was not there before, then it began to appear during physical activity, and over time - at rest;
- weakness, drowsiness, increased fatigue;
- cough (which becomes stronger when lying down);
- severe sleep apnea (appears a couple of hours after falling asleep).
Factors provoking the development of pathology
First of all, it should be noted that the development of diastolic myocardial dysfunction is facilitated by its hypertrophy, i.e. thickening of the walls of the ventricles and interventricular septum.
The main cause of cardiac muscle hypertrophy is hypertension. In addition, the danger of its development is associated with excessive physical stress on the body (for example, intense sports, heavy physical labor).
How to arrive for treatment
Factors contributing to the development of the main cause – hypertrophy – are separately identified and these are:
- arterial hypertension;
- heart disease;
- diabetes;
- obesity;
- snoring (its effect is caused by involuntary cessation of breathing for a few seconds during sleep).
results
The groups were homogeneous in age, gender composition, height and body weight, number of smokers, and the number of people with underweight. Obese patients were more common in groups 2 and 3. In group 1 there were no patients with coronary artery disease, hypertension, type 2 diabetes mellitus, or signs of heart and respiratory failure.
Spirometry data in the groups of patients with lung pathology did not differ significantly from each other, but were naturally reduced compared to those in the comparison group (Table 2). When comparing the structural parameters of echocardiography, a statistically significant increase in the diameter of the pulmonary artery was revealed in the PH group compared with group 1 ( p
<0.0001).
Diameter P.P. in patients without signs of PH was 6% more than in group 1 ( p
= 0.00023), and in the PH group it was 21% more than in healthy people, and 12% more than in patients without signs of PH (
p
< 0.0001 in both cases).
In the PH group, there was an increase in the EDR of the pancreas by 14 and 3% compared with that of groups 1 and 2 ( p
<0.0001 and
p
= 0.001, respectively).
TAPSE in the PH group was 15% lower than in the comparison group, and 5% lower than in the group of patients without signs of PH ( p
<0.0001 in both cases).
In the same group, there was a decrease in RV EF to 51%, which is 9 and 6% lower than in the first two groups ( p
<0.0001 in both cases).
There was an increase in pancreatic wall thickness compared to that in group 1 by 11% in patients without signs of PH and by 33% in patients with PH ( p
<0.0001 in both cases).
Table 2. Spirometry data, structural parameters of the right heart and pulmonary arterial pressure in the examined groups Note.
Here and in the table. 3: the differences in indicators are significant (p<0.05) when comparing * with the 1st group, ** with the 2nd group. EDV - end diastolic size; RVd - thickness of the wall of the pancreas in diastole. When assessing the diastolic function of the RV (Table 3), patients in the PH group showed a decrease in the rate of early diastolic flow Et by 8% compared to that in group 1 ( p
=0.46).
The Et/At ratio also did not differ significantly between the groups. There were virtually no differences between groups in the atrial systole velocity At and the time of deceleration of early tricuspid flow. In the group of patients with lung pathology without PH, compared with group 1, there was a significant decrease in CPTP by 6% ( p
<0.0001).
In patients with PH, compared with groups 1 and 2, there was a decrease in CPTP by 19 and 14% ( p
<0.0001 and
p
= 0.021, respectively).
The Et/CPTP ratio in the PH group was 19% higher than in group 1 ( p
= 0.00023), but did not differ significantly from that in the group of patients without PH (
p
= 0.18).
Table 3. Indicators of RV diastolic function in the examined groups Note.
Et/SRTP is the ratio of the speed of early diastolic transtricuspid flow to the speed of its propagation. When analyzing the indicators of spectral tissue Doppler annulus of the tricuspid valve (Table 4), there was a tendency towards a decrease in the speed of its early diastolic movement e't in the PH group compared with group 1 ( p
=0.19).
In the same group, compared with the 1st group, there was a tendency towards a decrease in the speed of late diastolic movement of the tricuspid ring a't ( p
= 0.07).
The e't/a't ratios did not differ between groups. There were also no intergroup differences in the speed of systolic movement of the tricuspid valve ring (s't) and the Et/e't ratio. In group 2, compared to group 1, there was a non-significant increase in the Thea index by 14% ( p
= 0.54).
In the PH group, this indicator was significantly higher by 43% than in group 1 ( p
= 0.00078), and there was a tendency to increase by 25% compared to group 2 (
p
= 0.07).
Table 4. Indicators of spectral tissue Doppler in the groups examined Note.
e't, a't, e't/a't, - speeds of early and late diastolic movements of the tricuspid valve ring and their ratio; s't is the speed of systolic movement of the distal part of the pancreatic wall; Et/e't is the ratio of the flow velocity of early RV filling to the velocity of early diastolic movement of the tricuspid valve annulus. Correlation analysis revealed a statistically significant relationship between SRTP and LADsr values ( r
=–0.51;
p
<0.0001) with a gradient of tricuspid regurgitation - GTR (
r
=–0.41;
p
<0.0001), SPAP (
r
=–0.44;
p
<0.0001).
In univariate logistic regression analysis, the probability of SRTP below 32 cm/s (Table 5) increased with increasing age, in the presence of COPD, respiratory failure stage II, coronary artery disease, CHF III F.K. The likelihood of detecting a reduced SRTP also increased the increase in GTR above 20 mm Hg, LBP above 25 mm Hg. Art. and MPAP above 30 mm Hg.
Table 5. Analysis of factors influencing SRTP less than 32 cm/s in logistic regression analysis Note. OR—odds ratio; CI—confidence interval.
When constructing a multiple linear regression model, which included such features as age, the presence of COPD, stage II DN, ischemic heart disease, an increase in LBP above 25 mm Hg, an increase in GAD above 20 mm Hg. Art., and MPAP is above 30 mm Hg. Art., it was revealed that only two factors had an independent effect on the decrease in SRTP: the presence of II degree DN (the risk of detection increased by 2.1 times) and an increase in LBP above 25 mm Hg. (the risk of detection increased by 2 times).
Methods for detecting pathology
Diagnosis of the development of a pathology such as diastolic dysfunction in the myocardium includes the following types of examinations:
- echocardiography in combination with Dopplerography (the study makes it possible to obtain an accurate image of the myocardium and assess functionality in a given period of time);
- electrocardiogram;
- ventriculography (in this case, radioactive albumin is also used to determine the contractile function of the heart);
- X-ray examination of the lungs;
- laboratory blood tests.