Sokolov-Lyon Index (SLI)
Sokolov-Lyon index (SLI) = SV1 (mm) + RV5 (mm) or RV6 (mm).
Normal: up to 48 mm in persons under 40 years of age and up to 38 mm in persons over 40 years of age
To determine this index, it is necessary to add the amplitude (depth) of the SV1 tooth to the amplitude (height) of RV5 or RV6. The resulting figure, expressed in millimeters, will be the index.
Content:
The Sokolow Index is a criterion used to diagnose left ventricular chamber enlargement of the heart based on the measurement of the waves that represent the left ventricle on the electrocardiogram.
The electrocardiogram is printed on a millimeter sheet. From the sum of the small squares that the wave's amplitude occupies, its voltage is obtained. The Sokolov index is the result of the sum of the amplitude of the S wave in precordial vectors V1 plus the R wave in V5 or V6. Thus: S V1 + RV 5 or 6 = Sokolov index.
A result greater than 35 mm indicates that the patient has left ventricular hypertrophy, meaning that their left ventricular heart chamber is thicker than normal.
This type of abnormality is a consequence of diseases such as hypertension, which causes the heart muscle to become overworked due to the high pressure it must overcome to pump blood.
Cornell voltage product (CVP)
Cornell voltage product (CVP) = [RaVL(mm) + SV3 (mm)] × QRS (ms)
Normal: less than 2440 mm/ms.
The Cornell voltage product is calculated a little more complicated: it is necessary to multiply the duration of the QRS complex, expressed in milliseconds, by the sum of R -aVL (mm) + S -V3 (mm). The difficulty is that you have to multiply large numbers and you can’t do it without a calculator. If the obtained value exceeds 2440, then we are talking about LVMH.
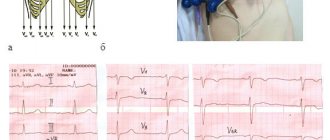
ECG
1: fourth intercostal space to the right of the sternum.
2: fourth intercostal space to the left of the sternum.
3: in the middle of the line connecting V2 to V4.
4: at the junction of the fifth intercostal space with the midclavicular line.
5: parallel to V4, but along the anterior axillary line.
6: parallel to the previous ones, but along the midaxillary line.
In this study, time, expressed in seconds, is measured in the horizontal plane. In this case, the voltage, expressed in volts, is in the vertical plane.
Therefore, on the graph paper on which the electrocardiogram is printed, a square measuring 1 mm in the horizontal plane corresponds to 0.04 seconds and 0.1 millivolts in the vertical plane.
OTHER CRITERIA
RV4 < RV5 > RV6 or RV4 < RV5 < RV6 - shift of the transition zone to the left
Now we will discuss the criterion of LVMH determined by the dynamics of the R wave in the precordial leads. The fact is that in non-hypertrophied myocardium the total excitation vector is directed to the apex, therefore the highest R wave will be recorded in lead V4. In the case of hypertrophy, (but not always) the vector shifts to the left, partly due to thickening of the lateral wall of the left ventricle, and partly due to changes in the boundaries of the heart. Because of this, the maximum R begins to be determined not in V4, as is normal, but in lead V5 or V6.
Many “old school” cardiologists consider this sign to be the most important, however, this is not so. The reason lies in the fact that cardiologists are accustomed to seeing mostly sick people who have hypertrophy in 80%-90%, but if they examine the entire population, then an erroneous conclusion about LVMH will be given to every second patient with such changes on the ECG. So, be careful with this criterion, although it has greater sensitivity than the above indices (ISL and KVP), but its specificity is no more than 60%, while for the above indices it approaches 100%.
ECG diagnosis of LV hypertrophy
Left ventricular hypertrophy
LV hypertrophy occurs in response to an increase in pressure in it, for example, with hypertension or aortic valve stenosis.
On the ECG, this is manifested by an increase in the amplitude of the R wave in the “left” leads (I, aVL and V4-V6) and an increase in the depth of S in the “right” leads (III, aVR, V1-V3).
Thickening of the walls of the LV leads to a prolongation of its depolarization (manifested by an increase in the rise time of the R wave) and to a change in repolarization (changes in the T wave and ST segment in the lateral leads).
SYSTOLIC OVERLOAD OF THE LEFT VENTRICLE
A separate concept in the LVMH section is “systolic overload of the left ventricle.” It must be said that in fact, the ventricle does not experience any special overload either at the time of ECG recording or during any other period of time, except for that which is associated with high blood pressure. There are situations when a person with blood pressure is 150/90 mm Hg. we see “systolic overload”, but in others, even with a pressure of 220/120 mm Hg, there is no hint of such changes. In addition, normalization of blood pressure never led to the disappearance of “overload”.
Systolic overload as an ECG phenomenon occurs in the case of severe hypertrophy, which leads to disruption of the repolarization wave, but we will not go into details, the main thing is that you understand the meaning of this term and do not confuse hemodynamics with electrical activity.
So, how does this “phenomenon” manifest itself? And it manifests itself in the form of disturbances in the repolarization processes of a very specific type (see further on the ECG), occurring in the area of the lateral wall of the left ventricle, always in combination with high R waves or, more often, in combination with positive criteria for LVMH (ISL or CVP).
In conclusion, it is worth noting that in my (and not only my) opinion, in the presence of positive criteria for ISL and CVP, we need to talk about quantitative signs of hypertrophy, while a shift of the transition zone to the left should be called qualitative signs of hypertrophy.
Answers to frequently asked questions
What is the current treatment for left ventricular myocardial hypertrophy?
Treatment of LVH primarily involves addressing the underlying cause. Medical or surgical intervention may be involved, depending on the underlying factor in the development of the disease and the condition of the patient.
Key treatment strategies for LVH based on cause:
- Hypertension is treated with lifestyle changes and medications.
- Aortic valve stenosis is usually treated surgically.
- Hypertrophic cardiomyopathy can be treated with drugs and surgical methods with the implantation of special devices.
- Athletic LV hypertrophy does not require treatment.
Treatment of hypertension that has caused LVH
For this disease, the following principles of therapy are used. 1 . Lifestyle changes:
a . Weight loss – LVH is more common in obese people, regardless of blood pressure level. A study of weight loss in such cases has shown that such a change has a positive effect on the course of LVH. Additionally, blood pressure control is improved. b. Healthy diet - if you have LVH, you need to eat more fruits and vegetables, reduce your intake of refined carbohydrates and foods saturated with fat. c. Limiting salt - you should reduce the amount of salt you consume and should not eat foods containing large amounts of salt (dried fish, sprats, cheeses, sausages). d. Regular physical activity - it is worth doing exercises lasting at least 30 minutes 3-4 times a week. You can try brisk walking for 30 minutes every day. If you have any other heart diseases or shortness of breath occurs during exercise, then you should first consult with your doctor. e. To give up smoking. f. Do not drink alcohol ; in some cases, harm to the body can occur even when using alcoholic beverages in moderation. g. Stress management – Meditation and other relaxation techniques may be helpful.
2. Drug treatment:
a. Thiazide diuretics – These types of medications can promote circulation, further lowering blood pressure. From this pharmacological group, chlorthalidone (Thalitone) and hydrochlorothiazide (Microzide) are often prescribed. They can be used as monotherapy or in combination with other antihypertensive drugs. This is the first option for antihypertensive therapy, but if necessary, the doctor may prescribe other medications. b. Angiotensin-converting enzyme inhibitors (ACE inhibitors)—These drugs dilate blood vessels, resulting in lower blood pressure. When blood pressure is low, the workload on the heart muscle also decreases and blood flow through the heart increases. Examples of medications in this group include captopril, enalapril (Vasotec), and lisinopril (Zestril). Side effects may include an irritating dry cough. c. Angiotensin receptor blockers (ARBs) have a similar effect to ACE inhibitors, but do not cause the development of a persistent cough. Examples from this group of drugs: losartan (Cozaar). ACEIs and BARs are not usually combined because this may increase potassium levels in the body (hyperkalemia). d. Calcium channel blockers (CCBs) - These drugs prevent calcium from entering the heart cells and blood vessel walls, resulting in lower blood pressure. Examples from this group: amlodipine (Norvasc) and diltiazem (Cardizem, Tiazac). e. Beta blockers . Medicines such as atenolol (Tenormin), acebutolol (Sectral) can lower your heart rate, lower your blood pressure, and prevent some of the adverse effects of stress hormones (adrenaline). Beta blockers are not usually prescribed as initial treatment for hypertension. Your doctor may recommend adding a beta blocker if another type of treatment is not effective.
Treatment of aortic valve stenosis that caused left ventricular hypertrophy
With aortic valve stenosis, the aortic opening becomes insufficient for blood to pass through. The left ventricle must work harder to push blood through, which increases the load on the heart. In such cases, surgery is performed to reconstruct the damaged valve or replace it with an artificial or tissue valve.
Treatment of hypertrophic cardiomyopathy, which can also cause LVH
Treatment for left ventricular hypertrophy associated with hypertrophic cardiomyopathy may include medications, surgery, device implantation, and lifestyle changes.
1. Lifestyle changes are the same as for hypertension. However, you need to check with your doctor whether you can exercise or not, which exercises are suitable, for how long and with what intensity they need to be performed.
2. Medicines to relax the heart muscle and slow the heart rate:
a. Beta blockers - metoprolol, propranolol and atenolol b. Calcium channel blockers - verapamil, diltiazem. c . If there are any arrhythmias, then amiodarone or other antiarrhythmic drugs are prescribed. d . Anticoagulants to prevent blood clots - warfarin.
3. Surgical intervention:
a. Removal of part of the thickened septum between the ventricles. b. Implantation of a cardioverter-defibrillator . The device is usually inserted if there is a life-threatening arrhythmia or an increased risk of sudden death due to cardiac arrest. This small device continuously monitors your heartbeat. If a life-threatening arrhythmia occurs, then the electrical shock is automatically blocked, followed by stimulation of the normal heart rhythm.
Left ventricular hypertrophy may also occur with athletic hypertrophy. It does not require specific treatment, but it is still better to reduce the intensity of training for 3-6 months. During this time, the ECG and echocardiogram can be repeated to reassess the thickness of the left ventricle.
Treatment of left ventricular hypertrophy with folk remedies practically does not produce results if the disease is already developing in full swing. Such methods of influence should be used only for the prevention of major diseases such as hypertension and diabetes.
Video: Is it necessary to treat left ventricular hypertrophy?
What diet is best to use for left ventricular myocardial hypertrophy?
The best way to prevent left ventricular hypertrophy is to follow a heart-healthy lifestyle, in which diet plays a significant role. Additionally, as noted above, you need to exercise regularly, maintain a healthy body weight, stop smoking and drinking alcohol, and control your cholesterol, glucose, and blood pressure levels. But a varied and balanced diet low in salt is of particular importance.
Diet plays a dominant role in the prevention of heart and vascular diseases, including left ventricular hypertrophy. It is especially important to consume omega-3 fatty acids, which are deficient in current diets. It has been scientifically proven that omega-3s play an important role in reducing the risk of developing pathologies of the cardiovascular system.
Omega-3 fatty acids are mainly found in marine fish such as salmon, tuna, mackerel or sturgeon, as well as green leafy vegetables, nuts and vegetable oils (such as flaxseed and canola). To ensure that you get the required amount of essential fatty acids, it is recommended to consume fish at least twice a week.
Various clinical trials have shown that omega-3 fatty acid supplements can reduce the incidence of heart disease, reduce the development of atherosclerosis, and prolong the life of patients with left ventricular hypertrophy.
The best recommendations for using diet for LV hypertrophy are as follows:
- The diet should contain low levels of animal fat, with a predominant amount of whole grains, fruits and vegetables.
- You should get into the habit of reading food labels before purchasing food in supermarkets, paying particular attention to the level of saturated fat. In particular, you need to take a closer look at the words “hydrogenated” or “partially hydrogenated”, which are often indicated on labels. You should not eat foods with these ingredients, as they saturate the body with “bad” fats and trans fats.
- It is important to avoid or reduce the amount of saturated fat in your diet (more than 20% of total fat is considered high). Consuming too much saturated fat is one of the key risk factors for heart disease. Foods rich in this type of fat include egg yolks, hard cheeses, whole milk, cream, ice cream, butter and fatty meats, as well as large portions of meat.
- Choose a low-fat protein diet containing soy, fish, lean chicken, lean meats, and low-fat or 1% dairy products.
- It is important to limit the amount of processed and fried foods that many people consume today.
- Avoid eating store-bought baked goods (such as bagels, cookies, and crackers) as they may be high in saturated fat or trans fat.
- It is necessary to use healthy methods of preparing fish, chicken and lean meat - grilling, boiling and baking.
- A diet is considered healthy if it is rich in fiber. In particular, it is recommended to use oats, bran, peas and lentils, legumes (such as beans, black beans, regular white beans), some grains and brown rice.
- The best solution is to avoid going to restaurants and other fast food establishments where healthy options are difficult to find.
DASH diet for left ventricular myocardial hypertrophy
Practicing a low-salt diet (DASH diet) for left ventricular hypertrophy helps reduce blood pressure, and therefore improve the patient’s condition. Beneficial effects on blood pressure in LVH are sometimes observed after several weeks of use.
The DASH diet is rich in important nutrients and fiber. It also includes foods that are rich in potassium, calcium and magnesium. Additionally, there is a lower sodium (salt) content than in a typical diet.
What are the best exercises to do for left ventricular hypertrophy?
Left ventricular hypertrophy, if severe, can eventually impair cardiac function by reducing contractile force. The best measure to prevent LVH is to prevent and adequately control high blood pressure with a low-salt diet, exercise, and appropriate antihypertensive medications.
Maintaining an active lifestyle with moderate levels of aerobic exercise can reduce the chances of developing LVH or moderate the severity of the disease.
Positive changes in well-being are especially noticeable in people who change their habits and begin to lead a more active lifestyle. Regular exercise, such as walking, cycling , for about four hours a week, reduces the risk of developing left ventricular hypertrophy. It has also been proven that physical activity within reasonable limits helps improve the condition of patients with long-term left ventricular hypertrophy. In particular, rehabilitation programs are used based on complex physical exercises, selected taking into account the individual characteristics of the patient.
The exercise program is based on criteria corresponding to the medical and cardiovascular indications of the patient:
- Modality : Continuity of exercise is important for patients with left ventricular hypertrophy. During the workout, various large muscles are used. Swimming, cycling, walking, etc. are best suited for this. With regular exercise, cardiovascular resistance is conditioned.
- Frequency : The minimum duration of training is three weeks, then a week can be taken off and suitable exercises performed again for three weeks.
- Duration: The workout should consist of warm-up and cool-down periods, stretching and flexibility exercises, and cardiovascular exercise for 20 to 40 minutes at a continuous pace or at intervals.
- Intensity: Should be moderate and comfortable, usually with a maximum functional capacity of about 40-85%.
- Gradual Progression : Each program should progress slowly, but with gradual progress in terms of exercise duration and intensity. Such dynamics are extremely necessary for patients with left ventricular hypertrophy.
During exercise, blood pressure may increase. Therefore, it is necessary to reduce exposure to stressors before starting an exercise program.
Limitations of criteria, IMPORTANT! IMPORTANT! IMPORTANT!
1. In the presence of complete or incomplete blockade of the left leg, the criteria do NOT work!
2. In the presence of complete blockade of the right leg, the criteria do NOT work!
3. If there are scar changes, the criteria do NOT work!
4. If the criteria are negative, this does NOT mean that there is no hypertrophy! Low sensitivity.
An attempt to identify left ventricular myocardial hypertrophy by ignoring points 1-3 is a mistake, which, however, is also made by cardiologists!
Well, let's see how it all looks.
Sokolov and Lyon
North American cardiologists Maurice Sokolov and Thomas Lyon based their professional careers on the study of hypertension and its complications.
One of the most common conditions associated with this disease is left ventricular hypertrophy, which is nothing more than a thickening of the muscular wall of the left ventricle of the heart.
These specialists described a way to calculate the state of the heart muscle by measuring the voltage of certain waves on the electrocardiogram. The technique was published in 1949 in a scientific journal. American Heart Journal and it was called "Ventricular complex in left ventricular hypertrophy obtained with unipolar precordial and limb electrodes."
The method is called the Sokolow-Lyon Index, and is one of the criteria currently used to determine left ventricular hypertrophy in patients with heart disease, especially hypertension.
EXAMPLE 1
On this ECG you can see almost all the criteria for left ventricular myocardial hypertrophy (LVMH).
1. Sokolov-Lyon index (ISL) = SV1 (19 mm) + RV5 (22 mm) = 41 mm (norm up to 38 mm)
2. Cornell voltage product (CVP) = [RaVL(13 mm) + SV3 (10 mm)] × QRS (100 ms) = 2300 ms*mm (the norm is up to 2440, this negative criterion was slightly missed)
3. Transition zone offset - RV4 < RV5 < RV6.
4. Systolic overload - we see ST depression in V5 and V6 and biphasic, predominantly negative, T, that is, a violation of repolarization processes.
Diagnostic ECG criteria for LV hypertrophy
There are a lot of diagnostic criteria for LV hypertrophy, but the Sokolov-Lyon index and the Cornish voltage index are most often used.
For a reliable diagnosis of LV hypertrophy, voltage criteria must be supplemented by non-voltage signs.
Voltage criteria in standard leads:
Voltage criteria in chest leads:
Non-voltage signs of LVH:
What else may indicate LVH:
Example 1: LV hypertrophy in a patient with hypertension
This ECG can detect several criteria for LV hypertrophy:
Example 2: LV hypertrophy in a patient with atrial fibrillation
Source
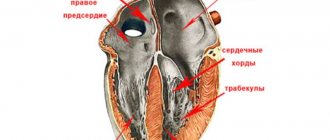
Portrait of hypertrophy
Left ventricular hypertrophy
Before we begin to describe the electrocardiographic signs of hypertrophy (enlargement) of the right and left ventricles, let us dwell on some aspects of pathophysiology and anatomy. We will try to imagine and describe together what a hypertrophied myocardium looks like. Perhaps this will help someone to remember the signs of hypertrophy (enlargement) faster and easier. So, normally the left ventricle (LV) is almost 3 times larger in mass than the right. This fact is explained by the fact that the LV operates under conditions of high resistance. He needs to overcome the vascular resistance that is created in the aorta, the efferent vessel.
The right ventricle (RV) is much easier; it does not encounter such vascular resistance. Therefore, he does not need the same muscle mass as his neighbor. A prerequisite for the formation of remodeling of the right and left ventricle (LV) is an additional increased resistance that one or the other has to overcome. When the pressure in the pulmonary circulation (pulmonary blood flow) increases, the pancreas experiences stress. When the pressure in the aorta increases or when there is an obstacle to the normal functioning of the LV for other reasons, this chamber of the heart experiences increased load.
Right ventricular hypertrophy
In order to cope with the situation and perform its pumping function, as before, the muscle fibers of the right or left ventricle thicken and lengthen. It seemed like these were good compensatory mechanisms. This chamber of the heart will become stronger and will continue to work. But everything has its own margin of safety. And the ventricles are no exception in this situation. For some time, these chambers of the heart operate at their previous level, but then, sooner or later, the compensatory mechanisms become exhausted. The heart muscle begins to lose its pumping function. What new characteristics does the right or left ventricle acquire in the case of established hypertrophy? Muscle fibers lengthen and thicken.
The camera has increased in size and weight. Sclerotic (overgrowth of connective tissue) and dystrophic processes in the myocardium due to depletion of energy reserves in the cell. An increase in the electromotive force of the heart and an increase in the excitation vector of the ventricle. The thicker the myocardium, the more energy the heart needs to expend in order for the electrical impulse to excite the entire thickness of the myocardium. Accordingly, the time of excitation of the ventricle increases. All these points lead to changes in the electrocardiogram, indicating the presence of hypertrophy.
When is surgery necessary?
Approximately 30% of patients with hypertrophic cardiomyopathy already have "left ventricular obstruction", which can be assessed and measured using Doppler ultrasound. A hypertrophied interventricular septum combined with forward displacement of the mitral valve reduces the size of the passageway between the left ventricle and the aorta (the "outlet tract") so that higher pressures are required. It is necessary to force blood from the ventricle into the aorta.
Obstruction may be absent at rest but present during exercise in an additional 30% of patients, and this phenomenon can be assessed using Doppler echocardiography performed during stress testing.
If the obstruction is severe and causing significant symptoms (dizziness and chest pain), relief may be indicated, usually done during cardiac surgery. It should be performed in centers with consolidated experience.
In most cases, hypertrophic cardiomyopathy is a benign heart disease with persistence of symptoms for decades after diagnosis. However, over many years, about 20% of patients may experience worsening symptoms and complications such as atrial and ventricular arrhythmias.
In hypertrophic cardiomyopathy, the walls of the muscle mass of the left ventricle are primarily damaged, which become thicker and larger than usual. In particular, a septum often occurs between the right and left ventricles. When the heart muscle is very thick, it has an increased need for energy and oxygen. Sometimes the coronary arteries cannot respond to the increased demand, so you may experience signs of oxygen deficiency even if you do not have a disease or obesity.
This is a change in the anatomy of the heart muscle with increased thickness, size and shape of the myocardium (heart muscle).
There are reasons for this, from genetic changes, even sports. but the most common cause is hypertension without adequate treatment.
This has consequences such as arrhythmias and cardiac dysfunction, with fatigue, chest pain and limited ability to perform physical and daily activities.
There are several treatments available, but following your cardiologist's recommendations early is fundamental to avoid a flare-up.
Just like an athlete in the gym gains muscle hypertrophy when he does a lot of heavy exercise.
Our heart becomes hypertrophied when it works too hard, i.e. when excessive stress is placed on it, such as hypertension or aortic stenosis. To overcome this increased resistance, the heart muscle (myocardium) must be hypertrophied, which is not good and is understood as an aggravating risk or rather end-organ damage. The good side is reversed most often with proper treatment.
The heart normally pumps blood, but a large, thick wall prevents the ventricle from filling and diastolic heart failure (the heart muscle becomes stiff and less elastic) can occur. The septum in the heart can become so thick that it partially blocks blood flow from the left ventricle and into the aorta.
Thick muscle also increases the risk of rhythm disturbances, both due to the fact that individual muscle fibers are affected, but also due to the high risk of oxygen deficiency, which can cause rhythm disturbances. You can see all kinds of rhythm disturbances in hypertrophic cardiomyopathy. However, there is an increased risk of more dangerous rhythm disturbances (ventricular tachycardia), which originate from the ventricles and can lead to cardiac arrest.
The cause of hypertrophic cardiomyopathy is predominantly hereditary. The condition may be asymptomatic and may be discovered by chance. When the heart muscle becomes thicker, most symptoms appear. Symptoms often worsen when you exercise because the oxygen and energy demands of the heart muscle increase during physical activity. Main symptoms:
- voltage,
- chest pain on exertion,
- heartbeat,
- dizziness from tension.
A cardiogram (ECG) can often raise suspicions that you have hypertrophic cardiomyopathy. The final diagnosis can be made by echocardiography (ultrasound examination of the heart). Once diagnosed, you will be referred to a hospital with specific knowledge about the disease.
Most cases of the disease are hereditary. Therefore, your close relatives will be offered testing to determine if they also have the disease.
If there is angina, arterial narrowing in the coronary arteries will be examined. This may be an X-ray examination of the cardiac coronary artery or myocardial scintigraphy.
The disease is primarily treated with medications. The first choice is a beta blocker. If you cannot take beta blockers, you can try replacing them with a calcium antagonist. If medications are not enough, you may be offered alcohol ablation. Alcohol is injected into the coronary artery, which affects the area of muscle that is too thick. This way, some of the muscle is removed and the symptoms are reduced. Myectomy is the removal of an area of muscle through a surgical procedure. If there is a risk of an abnormal beat, you will be offered a device that can stop the irregular rhythm if it occurs.
Importance and clinical significance
The gold standard for detecting ventricular hypertrophy is an echocardiogram. However, this research is expensive and requires trained personnel to conduct and analyze it.
The importance of the Sokolow index is that it is based on the measurement of the electrocardiogram, which is the basic test of clinical examination, and is also inexpensive, easy to perform, and can be analyzed by any physician.
Based on the electrocardiogram, the doctor diagnoses ventricular hypertrophy, and the patient is referred to a cardiologist for in-depth study.
The role of sport
Regarding fitness for sport in the presence of left ventricular hypertrophy, the benign origin of the disease should first be assessed, distinguishing it from hypertrophic myocardiopathy, which is one of the most common causes of sudden death in young athletes.
The distinction between these two conditions is made by the physician based on various elements collected during the medical history (type of sport, familiarity with the disease) and diagnostic tests.
An athlete's heart can be distinguished from a heart affected by hypertrophic myocardiopathy due to an enlarged ventricular cavity (which may be normal or reduced due to pathology) and a wall thickness of less than 16 mm (which may be greater in the presence of the disease).
In children
In families, the mode of transmission is usually “autosomal dominant”. This means that in most cases the disease is transmitted from parent to child with a 50% probability. However, in some families it is possible that the parent or child does not have an obvious clinical manifestation of the disease, that is, a wall thickness of more than 15 mm. This phenomenon means that the disease does not always manifest itself in all patients who carry the genetic defect. The development of hypertrophy usually occurs during adolescence or adulthood, later in women until the sixth or seventh decade, while in only a minority of patients hypertrophy occurs at birth or at a younger age.
Initially, hypertrophic cardiomyopathy is often asymptomatic, or symptoms may be misinterpreted by the patient. In these cases, the diagnosis is made during checks for other reasons, such as during a sports physical examination. The most common symptoms, when present, are:
- heartbeat,
- dyspnea,
- stress,
- chest pain at rest or stress.
To confirm the diagnostic hypothesis, after a cardiac examination, electrocardiogram and echocardiogram, other studies are performed:
- blood tests,
- dynamic ECG for 48 consecutive hours,
- stress test or cardiorespiratory test,
- magnetic resonance therapy with contrast medium.
These tests assess the severity of heart disease and the potential risk of complications. This data is supplemented by information provided by genetic testing (carried out with the consent of the patient after genetic counseling).
Once diagnosed, first-degree relatives (children's parents and siblings) are invited to undergo basic tests (physical examination, electrocardiogram and echocardiogram) to assess whether even some of them show signs of hypertrophic cardiomyopathy. Once the responsible genetic mutation has been identified in a patient, it is also looked for in first-degree family members.
At the end of this comprehensive evaluation, the specific genetic cause of cardiomyopathy can be identified with reasonable certainty, allowing the patient to be directed to the most appropriate therapy that is aimed at mitigating or eliminating symptoms and reducing the risk of complications. In fact, therapy may vary, based on the specific genetic mutation that causes hypertrophic cardiomyopathy and on the presence or absence of complications, particularly arrhythmias.