Main advantages and features of the method
The Holter device is a portable recorder that is attached to the patient's body using a belt. The recorder is connected by wires to electrodes installed at certain points in the chest. This technique has been used for a relatively long time. Here are its main advantages:
- Non-invasive. Wearing a halter does not cause pain or discomfort;
- Safety. Holter does not have a negative effect on the human body;
- Simplicity and accessibility. Holter studies are carried out in both public and private medical institutions;
- Information content. This type of research allows you to identify deviations even at an early stage.
Another advantage is the fact that you do not need to remain in a hospital setting to conduct the study. The patient can go home and lead his daily life, and a day later go to the doctor to remove the device.
How is the research conducted?
- The person must remove all clothing above the waist.
- The skin in the chest area is degreased to securely fix the electrodes.
- Special disposable sensors are attached to the body and connected to a recorder.
- The recorder is placed in a special small bag, which secures the device for the patient’s convenience.
- The patient can then go home. After 24 hours, you should return to the doctor to have the recorder removed. After this, the device is connected to a computer and the data obtained is analyzed.
Kinds
The following types of Holter monitoring have been developed:
- Full-scale monitoring , in which the procedure lasts 1-3 days. The device transmits the received data to a specialist for the purpose of quickly deciphering the results.
- Fragmentary method , when recording is made only at moments when a person feels pain or feels symptoms of arrhythmia. If health deteriorates, the patient himself presses the start button of the device.
When is Holter prescribed?
In cardiology, there are a huge number of indications for which daily ECG monitoring can be prescribed. Moreover, a holter can be prescribed not only if there are any deviations, but also for preventive purposes.
A doctor may prescribe this study in the following cases:
- Sudden fainting, loss of consciousness for no apparent reason;
- Frequent dizziness;
- The pulse is too high, or, conversely, low;
- Complaints about heart failure;
- Evaluation of the effectiveness of antiarrhythmic therapy;
- Assessment of heart rhythm after installation of a pacemaker;
- Complaints of shortness of breath or chest pain;
- Idiopathic hypertrophic cardiomyopathy;
- The presence of various types of arrhythmia, including atrial fibrillation;
- Feeling of “missed heartbeats”;
- Suspicion of angina pectoris;
- Unsatisfactory electrocardiogram readings;
- Chronic heart failure;
- Preventive examination of athletes, endurance testing;
- Determining the degree of compliance of a person’s physical capabilities with the requirements of the profession
Holter monitoring has no contraindications, except for acute inflammatory processes on the skin in the chest area (where the sensors are attached). The Holter test method can be performed on people of all ages, including pregnant women. There are no restrictions on the number of studies or intervals between them. In order to monitor the progress of treatment, the study is carried out repeatedly.
List of indications for a Holter study:
- The absence of pathological changes on a traditional ECG when the patient complains of burning chest pain, shortness of breath, that is, symptoms indicating cardiac ischemia.
- Symptoms indicating arrhythmia: dizziness, fainting, rapid heartbeat, interruptions in heart function.
- Analysis of the effectiveness of treatment of coronary heart disease and arrhythmias.
- Monitoring the functions of the pacemaker.
- Dynamic monitoring of people at risk for arrhythmias and coronary heart disease.
- Arterial hypertension in combination with cardiovascular failure.
- Preparation for surgery in people with myocardial pathology.
Important! Holter monitoring to assess the condition of the heart muscle is recommended for persons who have undergone chemotherapy or radiotherapy for cancer.
How to behave during monitoring
A few recommendations for monitoring:
- During the examination, the patient should lead a normal lifestyle without reducing physical activity to a minimum;
- The recorder and sensors on the body cannot be wet, that is, while wearing the device, it is necessary to completely avoid water procedures;
- Avoid mechanical and thermal damage to the halter;
- It is not advisable to travel, fly on an airplane or go on attractions during the examination;
- Typically, other electrical devices do not affect the operation of the Holter monitor, but it is still best to keep it away from microwave ovens, magnets, metal detectors, etc.
In addition, the patient must keep a special diary and record all actions performed during the day, indicating the time.
For example, the following actions should be noted in the diary:
- Time of administration and name of all medications taken during the day;
- Meal times, stressful situations;
- Time of going to bed, number of awakenings at night, time of getting up;
Climbing stairs is recommended as physical activity. For example, this can be done in your own entrance, going up to the 5th-10th floor. You need to indicate in your diary the start time of the climb and the end time. If you feel any discomfort while wearing the halter, this should also be noted in the diary.
Decoding the results
The received data is processed by a computer program - a decoder. After studying the results, the doctor gives a conclusion that includes information about the heart rate, the presence of extrasystoles and arrhythmias, changes in the blood supply to the myocardium, the reaction of the heart muscle to stress and other parameters. All identified pathologies are confirmed by ECG printouts for the monitoring period.
If you are worried about dizziness, aching pain in the heart, shortness of breath of unknown origin, contact a cardiologist at the Caring Doctor clinic, who will prescribe a heart study using Holter monitoring. This modern technique will allow the doctor to detect heart disease in the early stages, prescribe the correct treatment and prevent serious complications such as heart attacks and strokes.
What the study will show
After the holter is removed, the doctor deciphers the data using a computer program. A graph is created on the monitor with cardio indicators, which are studied by a specialist. Typically, a 24-hour ECG provides a comprehensive report of cardiac activity. Typically the decryption procedure takes about 2 hours. You can wait for the results or get them the next day.
Using Holter monitoring, you can record various heart rhythm disturbances, tachycardia, arrhythmia, extrasystoles, etc. Please note that the conclusion of a Holter study is not an official diagnosis. To make a diagnosis, you will need to consult your doctor, and possibly additional diagnostic methods.
You can obtain more detailed information about a 24-hour Holter study during an in-person consultation with a doctor. Be healthy!
Difference between ECG and Holter monitoring
A conventional electrocardiograph (ECG) records and evaluates the work of the heart in a short period of time. An ECG reveals only persistent changes in the myocardium, which are not affected by general health, physical activity, or emotional background (stress, anxiety). Even if the day before a person had an attack of pain or heart rhythm disturbances, the cardiograph may not show any pathological changes.
With Holter monitoring, the electrical activity of the heart is recorded for 1–3 days, which makes it possible to see changes in the functioning of the heart while the patient is active, as well as during periods of rest and sleep. The Holter study is more informative and detects the slightest deviations from the norm that occur spontaneously and irregularly.
The latest models of the device are equipped with additional devices for recording daily blood pressure.
Complications
As such, no health complications were recorded after this study; rather, there were some inconveniences associated with wearing the device.
Firstly, the recorder has weight and size, although small (from several tens of grams to 500), but sleeping or performing any active actions with it is not very comfortable.
Secondly, a person entangled in wires is nowadays associated with a terrorist. As a result, misunderstandings may arise, even leading to serious police proceedings. Therefore, you must always have a medical certificate with you with a photograph of the device, which is issued by the medical center. institution simultaneously with the installation of the device.
How is a daily ECG taken?
The procedure for Holter ECG monitoring from the patient's point of view is simple and does not imply any serious restrictions or complex preparation.
Some inconvenience will be that after installing the sensors you will have to avoid taking a shower (bath) for 24 hours. Therefore, the person being examined needs to take a shower in the morning before Holter diagnostics.
A male patient (if necessary) may be asked to remove chest hair.
The female patient will have to stop wearing a bra for the duration of the study.
The installation of the monitor and electrodes itself takes no more than 10 minutes. The portable recorder, about half the size of a 1980s cassette player, is usually clipped to your belt. Wires with adhesive electrodes go from it to the heart area.
Detailed instructions follow. In particular, the patient is asked to keep a diary of conditions: to record the time of meals, sleep, moments of physical activity (walking, running, etc.) or stress. They will be asked to pay special attention to recording in time complaints of weakness, pain, dizziness, uneven heartbeat, etc.
After this, the person is allowed to live a normal life for 24 hours. (Of course, patients examined in a hospital setting receive other recommendations).
A day later the monitor is removed. The specialist begins to analyze the collected information.
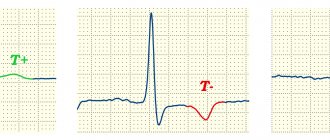
ECG waves and waves
I suggest sticking to a simple rule: the teeth are sharp and the waves are smooth. What kind of waves and waves can be detected on an ECG?
As you can see, there are only eight of them (I do not count the possible splitting R).
The P wave reflects atrial contraction.
The delta wave is not normally observed and is pathognomonic for WPW.
QRST - waves of the ventricular complex, are very variable. R can split into 2 teeth, for example, with blockade of the right bundle branch in V1-V2.
The epsilon wave is commonly seen in arrhythmogenic right ventricular cardiomyopathy.
The U wave is an intermittent manifestation of ventricular repolarization, most often detected in V5.
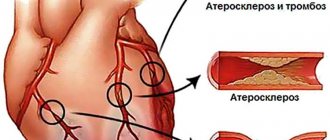
Ankle-brachial pressure index - ABI
The ankle-brachial index is a parameter that allows you to assess the adequacy of blood circulation in the lower extremities.
For this purpose, blood pressure is measured in the shoulder and ankle area. After this, these indicators are compared, as a result of which the doctor receives the ankle-brachial index. Typically, the pressure in the shoulder and ankle areas is the same. However, if the pressure in the ankle area is lower than in the shoulder area, this means that the arteries in the lower extremities may be narrowed. To determine the ankle-brachial index, the doctor uses a conventional blood pressure measuring device or an ultrasound machine. However, this parameter does not allow determining the location of arterial blockage. The ankle-brachial pressure index reflects the degree of stenosis or occlusion of the arteries of the lower extremities due to atherosclerotic obliteration. ABI <0.9 in both legs is considered positive for the diagnosis of peripheral atherosclerosis.