Numbness of the fingers is a complete or partial loss of sensation in the entire hand or individual fingers, which can be on one or both hands. The correct name is hypoesthesia. This symptom occurs in many neurological disorders, but also occurs in healthy people.
Each peripheral nerve has a motor and a sensory part. Irritation or damage to sensory fibers of any nature - mechanical, tumor, inflammatory, autoimmune - causes a disorder in the form of numbness, burning, tingling.
At CELT you can get advice from a neurologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
In a healthy person, numbness in the fingers of the hand – most often the right one – occurs due to constant overload of the hand muscles. This happens to pianists, hairdressers, programmers, and sometimes to massage therapists and cosmetologists. Sometimes the hands go numb during sleep, when a person lies on his side for a long time with his hand placed under his body. In all these cases, numbness is caused by a temporary disruption of blood flow in the arm due to mechanical compression of blood vessels and nerve trunks. Numbness is often accompanied by a burning sensation or a crawling sensation, but all this quickly passes after the limb returns to its normal physiological position.
Provoking factors
A completely healthy person rarely experiences numbness; they may indicate a hidden pathology in the form of:
- consequences of injuries;
- various diseases of the spinal column;
- joint inflammation;
- degenerative or destructive diseases of the cartilage and ligaments of the hand;
- nervous and mental disorders;
- persistent decrease in blood pressure;
- diseases of the endocrine glands.
There are currently no clear scales that determine the severity of hand numbness. If the unpleasant sensations bother you from time to time and go away after simple movements or rubbing, then you hardly need to worry. However, in case of frequent repetition of numbness, when it happens several times a week or the discomfort increases, you should consult a doctor as soon as possible, as this may be the beginning of the disease.
Everyday reasons
Numbness of the right hand very often occurs due to impaired blood flow or pinched nerve. In these cases, as a rule, the symptom appears at night. It can be provoked by an uncomfortable body position, which causes stagnation of blood and lymph in the limbs. To remove discomfort, just change your position and stretch your hand. During sleep, a limb may become numb due to the habit of placing your hand under your head. In this case, you need to change the pillow and try to get rid of the habit.
Other reasons:
- Uncomfortable posture while working.
- Carrying uncomfortable bags or suitcases;
- Occupational activity that requires holding the arms in an upright position.
- Hypothermia
- Physical stress for a long time.
Diseases in which numbness of the hands is a symptom
These are conditions such as:
- rheumatic diseases of the joints of the fingers;
- osteochondrosis of the cervical spine, which also causes coordination problems, headaches, and limited movement of some muscles of the shoulder girdle, which is caused by bone growths or osteophytes;
- vertical and horizontal protrusions (hernias) of the intervertebral disc;
- thrombosis of blood vessels of the hand or finger;
- multiple sclerosis, in which the myelin sheath of the nerve is destroyed and the central nervous system is affected;
- carpal tunnel syndrome or another type of tunnel syndrome, when a nerve is compressed in a bone or muscle-ligamentous tunnel;
- metabolic disorders caused by diabetes mellitus;
- anemia or anemia, when tissues lack oxygen;
- inflammation of the brachial nerve plexus;
- various inflammatory processes of hand tissues, aseptic or purulent;
- amyotrophic lateral sclerosis or ALS, when at the onset of the disease some patients interpret increasing weakness in the arm as “numbness”
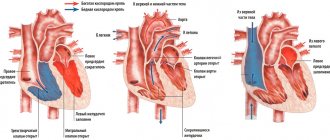
- disturbance of blood flow in the brain - in fairness, it must be said that in this case, movements, vision, speech are also most often impaired, but this is also one of the common reasons why the fingers suddenly go numb;
- Raynaud's syndrome, developing as a result of vibration or genetically determined, when numbness is accompanied by pallor, turning into cyanosis, and then into redness of the skin of the hand
- alcohol intoxication, in which the hands become numb like “gloves”, which is caused by damage to the peripheral nerves;
- diphtheria, which, thanks to universal vaccination, occurs easily and in an erased form; one of the manifestations may be polyneuropathy.
Numbness of the fingers may be the reason for a clinical examination, which will eventually reveal the truth. Modern diagnostic equipment makes it possible to give a preliminary conclusion already during the first day of the examination, or at least significantly narrow the range of the diagnostic search.
Numbness of each finger has its own characteristics. Since the branches of three main nerves are responsible for the innervation of the skin of the hand.
Why does the little finger on my left hand go numb?
Paresthesia on the left requires special attention. They can be a sign of cardiovascular pathologies: angina pectoris, myocardial infarction and stroke. These conditions are accompanied by concomitant symptoms, but there are also isolated cases when only the little finger on the left hand goes numb , and then the clinical picture unfolds.
Etiological factors also include osteochondrosis, local ischemia and other pathologies listed for the corresponding finger on the opposite side.
What can you think about when different fingers are numb?
All fingers on the hand are innervated differently, and by the characteristics of unpleasant sensations one can indirectly judge what caused the disease.
The first or thumb on the palmar surface is innervated by the median nerve, most often irritation is caused by compression or compression. People who constantly load this finger suffer - watchmakers, pianists, jewelers.
In some cases, the cause is a benign tumor that mechanically compresses the nerve. This may be a neurofibroma arising from supporting or glial nerve cells, or a hemangioma, the source of which was capillaries.
People who constantly carry heavy bags or grip handlebars excessively may develop stenotic transverse ligamentosis. This is a condition in which the ligaments lose their natural elasticity, become stiff and stop stretching. The result is the so-called carpal tunnel syndrome with damage to the median nerve.
The index finger and thumb on the dorsal surface are innervated by the radial nerve. Impaired sensitivity in them may be a manifestation of inflammation of the epicondyles of the humerus or epicondylitis, or compression of the radial nerve in the area of the humerus.
You should consult a doctor if numbness lasts longer than 5 - 10 minutes, does not go away after kneading and straightening the hand, and repeats several times during the week.
The middle finger of the hand is partly innervated by the median and partly by the ulnar and radial nerves - its numbness is accompanied by a feeling of “twisting” of the entire palm, similar to calf cramps. Sensory disturbances also appear in this finger when carpal tunnel syndrome occurs, when the transverse ligament presses the nerve too much against the bones of the wrist. Loss of sensitivity is noticeable more often at night, it becomes difficult to hold objects, and shaking the hand stops the discomfort. It seems to a person that the brush has become heavier and thicker. Sometimes swelling does occur.
Often, numbness of the finger occurs in people who are constantly exposed to hypothermia, when they develop inflammation of the inner wall of blood vessels or endarteritis.
The fourth and fifth or ring and little fingers are innervated by the ulnar nerve. The habit of constantly leaning on the elbow, as well as working with trays and daily overload of the wrist contribute to the damage. In men, numbness of these fingers may be the first sign of contracture due to degeneration of the aponeurosis or tendon plate of the palm. Unpleasant sensations in these fingers cannot be ignored, since if the ulnar nerve is damaged, contracture or immobility can form in the joints of the fingers.
Fingertips - it is most difficult to determine why the tips become numb, since the number of reasons is large. This is a violation of the blood supply in the cervical spine, caused by the formation of an atherosclerotic plaque, iron deficiency, the onset of diabetes mellitus, and inflammation of the pancreas. This is inflammation and degeneration of the finger joints, Raynaud's syndrome, venous insufficiency and thrombophlebitis that complicates it. These are chronic stresses and acute traumatic experiences that happen in the life of every person. These are arterial hypertension or vascular hypotension, chronic poisoning, harmful working conditions.
What causes the little fingers on the hands to go numb: reasons
Bilateral, symmetrical damage is possible with:
- degenerative-dystrophic lesions of the spine;
- metabolic and autoimmune diseases: diabetes, scleroderma;
- spasm of microcirculatory vessels;
- anemia;
- alcoholic polyneuropathy;
- infections of the nervous system.
When both little fingers on the hands go numb, the reasons may be inflammatory damage to the cartilage and articular structures. These are osteoarthritis, tendovaginitis, myofascial syndromes that affect the membrane covering the muscles. This list includes rheumatoid arthritis, osteoarthritis, consequences of a fracture of the radius, and tendon sprains.
When the little and ring fingers on the hand go numb , this is a characteristic sign of radiculitis, protrusion or herniated intervertebral disc. The root cause may be cardiac ischemia, but then discomfort appears at night, and the unpleasant sensations spread to the inner side of the forearm. This symptom also occurs with hypothyroidism, a decrease in thyroid function.
The choice of therapy depends on the diagnosis. Treatment comes down to eliminating the underlying disease and local effects: applying ointments, physiotherapeutic procedures. Electrophoresis, amplipulse, laser, and magnetic therapy are recommended. Medicines used include analgesics, anti-inflammatory drugs, and muscle relaxants. Drugs that improve blood microcirculation are indicated.
Our doctors
Pankov Alexander Rostislavovich
Neurologist
40 years of experience
Make an appointment
Novikova Larisa Vaganovna
Neuropathologist, Candidate of Medical Sciences, doctor of the highest category
Experience 39 years
Make an appointment
When should you see a doctor?
Most often, numbness is a transient and quickly passing condition. However, you should be wary if such sensations are repeated too often (for example, your arm goes numb every night or your leg goes numb every time you sit for a long time) or seem inadequate to the situation (there is no mechanical compression, but there is numbness). In the first case, it may be enough to change uncomfortable furniture to more ergonomic and orthopedic furniture, but it is better to seek advice from a neurologist, since numbness may be a symptom of a serious disease of the nervous and cardiovascular systems.
Diagnostics
Conducted individually, the search begins with excluding the most dangerous conditions. According to indications, the following studies may be prescribed:
- Electroneuromyography (ENMG of the upper extremities)
- duplex scanning of arteries and veins of the upper extremities
- X-ray of the cervical spine
- Magnetic resonance imaging of the cervical spine, brain, joints
- blood chemistry;
A specific list of diagnostic procedures is determined by the attending physician based on clinical examination data. Sometimes a diagnostic search leads to the discovery of diseases that a person did not even suspect about.
When is numbness normal?
Typically, numbness includes a number of features:
- complete loss of skin sensitivity of the limb,
- may sometimes be accompanied by painful hypersensitivity,
- feeling of an arm/leg like cotton wool, not belonging to a specific person and not connected with him,
- motor function is preserved, but significantly impaired (it seems to the person that he controls the limb solely by the power of thought),
- loss of muscle tone, such as the inability to put weight on a numb leg,
- the condition goes away after changing position, when normal blood circulation is restored,
- the appearance of “goosebumps” on the skin when blood again begins to flow into the numb area,
- As blood flow is restored, severe pain and burning may occur, which will subside as soon as circulation in the numb area returns to normal.
Treatment with folk remedies
The following recipes help with numb hands:
- as a compress or therapeutic bath, use a mixture of 2 liters of milk, 600 g of salt and 50 g of honey, heated to 60? C;
- apply an infusion of wild rosemary with apple cider vinegar (1:3) 3 times a day;
- infusion of garlic (several cloves) in vodka (400 ml) taken orally, 3-5 drops dissolved in water;
- for 1 liter of vegetable oil - 100 g of ground black pepper, cook for 30–40 minutes, rub the cooled product into the skin of the affected limb.
Ulnar and median nerve neuritis
Neuritis is an inflammation of the nerve resulting from hypothermia, infectious pathologies, injuries, circulatory disorders or lack of vitamins in the body. Diseases such as diabetes mellitus, malfunctions of the thyroid gland, as well as intoxication with various toxic substances can also provoke the appearance of neuritis.
Sensitivity disorder in areas innervated by the nerve is one of the main symptoms of neuritis. When the ulnar or median nerve of the right limb is damaged, the ring finger on the right hand goes numb, and a number of other signs appear.
The inflammatory process in the ulnar nerve can be primary or secondary. Primary neuritis develops independently of other existing diseases, and can occur as a result of traumatic mechanical actions - constant support of the elbow on the edge of a table, work machine and other hard surfaces.
Secondary, or symptomatic, neuritis is a complication that occurs against the background of:
- bursitis of the elbow joint;
- tenosynovitis;
- synovitis;
- deforming osteoarthritis;
- injuries;
- osteoma (benign bone formation).
If the nerve of the left limb is damaged, the patient may feel that the ring finger on the left hand is numb, and there is also no sensitivity in the little finger and half of the middle finger. Weakness bordering on atrophy begins to develop in nearby muscle structures. In certain areas of the ulnar nerve, compression or ischemia such as tunnel syndrome is possible.
We also recommend reading: Tunnel neuropathy of the ulnar nerve
Therapy for ulnar nerve neuritis includes the use of the following:
- antibiotics;
- antiviral drugs;
- vasodilators;
- anti-inflammatory and analgesics;
- decongestants;
- B vitamins;
- anticholyesterase drugs;
- biologically active stimulants to accelerate the regeneration of damaged tissues.
In case of traumatic neuritis, mandatory immobilization of the limb is performed.
Median nerve neuritis cannot be overlooked, since its onset is characterized by sharp and severe pain in the forearm, hand and fingers. Numbness occurs in the ring, thumb, index and middle fingers, as well as parts of the palm in this area.
A characteristic feature of median nerve neuritis is the inability to turn the hand palm down and difficulty bending the hand at the wrist joint. Bending the first three fingers is also impossible. There is a similarity to the “monkey’s paw”, when the thumb is located in the same plane as the other fingers. This occurs due to severe atrophy of the muscles surrounding the thumb of the right or left hand.
The causes of median nerve neuritis are:
- injuries - bruises, wounds, dislocations, fractures;
- inflammatory processes in the elbow or wrist joint (arthritis, arthrosis, bursitis);
- tumors;
- post-traumatic hematomas;
- endocrine disorders (diabetes mellitus, acromegaly, hypothyroidism);
- joint pathologies – gout, rheumatism.
Treatment of median nerve neuropathy begins with eliminating the cause, and may include the following measures:
- drainage of hematoma;
- reduction of dislocation;
- excision of the tumor;
- relief of inflammation in joints;
- correction of endocrine disorders;
- ensuring rest for the injured limb.
Pain and inflammation are relieved with nonsteroidal anti-inflammatory drugs; in severe cases, corticosteroid medications are used, as well as injection blockades.