- From the moment of pregnancy, a complex of changes occurs in a woman’s body, which covers the functions of all organs and systems, is observed throughout pregnancy and is within the physiological boundaries characteristic only of the state of pregnancy.
The set of changes includes:
- cessation of menstruation (changes occur in the mucous membrane of the uterine cavity caused by changes in the functional state of the ovary);
- prolonged low-grade fever (the influence of progesterone, an ovarian hormone, on the thermoregulation center in the brain);
- formation of the placenta - a new endocrine gland;
- change in a woman’s appearance;
- the emergence of a pregnancy dominant in the cerebral cortex, which ensures clear coordination of the functions of all organs and systems in the interests of the developing fetus;
- changes in the function of the endocrine glands;
- changes in the uterus (the greatest changes compared to other organs);
- changes in metabolism;
- changes in hematological (blood) and hemodynamic (blood movement) parameters;
- change in circulating blood volume;
- changes in the blood coagulation system;
- changes in the functioning of the cardiovascular system.
That is, with the onset of pregnancy, your body begins to completely restructure its functioning. He is preparing to bear the fruit, give birth and feed the child. Therefore, such a restructuring is a normal state for a pregnant woman.
| A healthy person has the same indicators (the numbers you see on the analysis form are normal), for example, blood indicators, urine indicators, etc. |
| For a sick person , there are indicators; they vary depending on the patient’s condition and his disease. |
| A pregnant woman is her own story. Her laboratory values may vary depending on the physiological course of pregnancy. Moreover, in different trimesters of pregnancy, each indicator has its own norm, and these norms for a pregnant woman do not coincide with the norms for a healthy person. |
Moreover, sometimes what is normal for a pregnant woman is considered pathological in a non-pregnant woman. But for a man it’s generally fatal; you can’t live with something like that.
Dear men, loving husbands!
Remember that your pregnant wife is an “unusual” person the entire time she is carrying your child. That is why a loving husband should not allow his wife to overwork herself with housework. A pregnant woman needs to create favorable conditions so that she can safely bear and give birth to a child, i.e. so that her body can qualitatively adapt to changing conditions as the pregnancy progresses (the baby grows, develops, eats, “breathes,” etc. - conditions are constantly changing).
If a pregnant woman’s body cannot adapt normally, then she will experience various unfavorable conditions, primarily for the child. For a woman, these are also unfavorable conditions. In especially severe cases, pregnancy is sacrificed to save the woman, because... terminating a pregnancy in this condition immediately leads to recovery (conditionally to recovery), but your child will no longer be born.
Always take care of women! And especially during pregnancy!
Treatment
The feasibility of treating tachycardia is assessed based on the results of an examination of the pregnant woman. If palpitations are physiological and transient, the doctor may recommend lifestyle changes and eliminate psycho-emotional stress. According to indications, sedatives approved for use during pregnancy may be prescribed. If tachycardia is associated with cardiac or endocrine pathology, drug treatment is selected by the appropriate specialist.
Draw your attention to! This article is not a call for self-medication. It is written and published to improve the reader's knowledge about his own health and understanding of the treatment regimen prescribed by the doctor. If you experience similar symptoms, be sure to seek help from a doctor. Remember: self-medication can harm you.
The fetoplacental system is like a new endocrine gland
After implantation of the zygote in the uterine cavity, a new endocrine gland begins to form in the woman’s body - the placenta (baby place).
The placenta has two parts: fetal and maternal, the blood circulation of which never mixes. These parts of the placenta are as close as possible, which allows for the exchange of substances between the body of the mother and the fetus, i.e., in essence, allows the child to “eat, write and breathe,” and, therefore, grow and develop.
Metabolism between the mother and fetus is the main factor for its development. The exchange is carried out due to the permeability of the placenta, which is disrupted in most acute and chronic complications during pregnancy. Violation of the integrity of parts of the placenta and deterioration of its permeability leads to fetal death and termination of pregnancy.
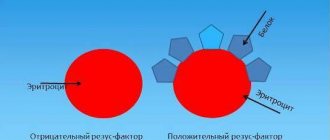
The death of the fetus and termination of pregnancy is also possible for another reason, when the mother’s body suddenly decides that the fetus is a foreign protein for it. But this is actually true. However, nature has provided a protective mechanism that does not allow the mother's immune system to recognize antigens of paternal origin embedded in the child.
This protective mechanism consists of certain factors that block the mother’s immune system and provide local immunological comfort. With spontaneous abortions, blocking factors in the mother's blood are reduced or absent.
The placenta produces a wide range of hormones and specific proteins that enter the mother's blood and amniotic fluid. They regulate the normal course of pregnancy and fetal development by changing the function of other endocrine glands and life support organs in general.
By the level of hormones and specific proteins of the placenta, determined in the mother’s blood, in the fetal blood or in the amniotic fluid, the condition of the fetus and the function of the placenta can be assessed, which is what obstetric endocrinology deals with. Thus, studying the endocrine function of the fetoplacental complex can significantly improve the diagnosis of the fetal condition at different stages of pregnancy.
The appearance of a new endocrine gland leads to other changes in the female body.
The appearance of a woman changes. Appears:
- pigmentation of the skin (forehead, cheeks, chin, upper lip, white line of the abdomen, nipples and parapapillary zones), which is associated with significant stimulation of pigment formation by skin cells. The formation of pigment depends on the melanoform hormone of the adrenal gland, increased production of which occurs during pregnancy;
- low-grade body temperature is noted , which can last up to 16-20 weeks of pregnancy and is associated with hormonal fluctuations.
From the moment the placenta begins to produce progesterone, the temperature decreases and returns to normal.
- There is engorgement and soreness of the mammary gland due to an increase in its volume as a result of the proliferation of glandular tissue, enlargement of the nipples and protrusion of the areolar glands. In the second half of pregnancy, colostrum may be released;
- violation of facial proportions (enlargement of the nose, lips, chin, thyroid gland, especially in the second half of pregnancy), some enlargement of the limbs;
- stretching of the tissues of the anterior abdominal wall , mammary gland, thighs and the appearance of striae (“pregnant stripes”) in these areas (stria gravidarum). Their occurrence is associated with excessive stretching of the abdominal wall; this is more often observed in persons with a large abdominal volume (large fetus, polyhydramnios, multiple pregnancy) or with some lack of elastic fibers in the skin;
- varicose veins worsen or appear for the first time , especially in the lower extremities;
- The “proud posture and gait” of a pregnant woman is caused by a shift in the center of gravity of the body , increased mobility of the pelvic joints and limited mobility of the hip joints.
- Progressive increase in body weight , which is caused both by the growth of the fetus and uterus, and by the characteristics of metabolic processes and fluid retention in tissues. The average weight gain during pregnancy is 10-12 kg, of which 5-6 kg is due to the fertilized egg (fetus, placenta, amniotic fluid), 1.5-2 kg for enlarged uterus and mammary glands, 3-3.5 kg - to directly increase a woman’s body weight.
Before childbirth (3-4 days), a pregnant woman’s body weight drops by 1.0-1.5 kg, due to the peculiarities of metabolic processes.
40th week of pregnancy: how is the baby developing?
40 weeks – full-term pregnancy. The weight of a child born at this period ranges from 2,600 g to 4,400 g, and his body length is 48-53 cm. These indicators are very arbitrary, since at 40 weeks miniature babies weighing 2,600 g and real heroes are born, whose body weight approaches 5,000 g. The body length of newborns can also vary from 45 to 55 cm.
Most women give birth at 40 weeks. At this stage, the baby is completely ready for birth; it meets all the parameters of a full-term baby. Before birth, the baby presses its arms and legs closely to the body, bends its head as much as possible and presses against the exit of the uterus. This position makes it possible to pass the birth canal with the narrowest part of the skull. During labor, with each contraction, the child gradually moves downward; he does not move in a straight line, but makes helical-translational movements, as if screwing into the mother’s birth canal. As the newborn moves forward and his head descends completely, the cervix opens completely. This is followed by pushing, that is, contractions of the uterus that move the baby along the birth canal. The baby's head gradually appears, followed by his body. Childbirth is a complex mechanism that is aimed not only at the safe passage of the birth canal by the child, protecting him from accidental injuries due to increased pressure, but also at preventing ruptures of the woman’s soft tissues.
The structure of the external (and internal) genital organs changes
- The external genitalia become swollen and hyperemic. Cyanosis of the mucous membranes of the vaginal part of the cervix, vagina and its vestibule occurs, which indicates vasodilatation and blood stasis, facilitating serous permeation of the tissues necessary for the deposition of nutrients at the site of attachment of the fertilized egg to the uterine wall.
- The vagina expands and lengthens somewhat during pregnancy. The walls of the vagina are swollen and thickened. The discharge becomes more abundant, mucous in nature, milky white or yellowish in color with an acidic reaction. In a healthy pregnant woman, the vagina has I-II degrees of cleanliness.
The uterus changes the most during pregnancy compared to other organs.
Its size increases during pregnancy in all respects:
- weight - from 50-100 g to 1-2 kg!!!
- length - from 7-9 cm to 50 cm,
- volume - 500 times, reaching 2-3,000 cm3 (liters) or more.
Accordingly, changes occur in all tissues, blood supply and innervation of the uterus:
- The shape and position of the uterus changes during pregnancy. As the uterus grows, it emerges from the pelvis into the abdominal cavity, rising in the 9th month of pregnancy to the xiphoid process. The shape of the uterus is asymmetrical due to the bulging of the part where the placenta is attached.
- Thin arteries and veins of the uterus turn into powerful trunks, which become corkscrew-shaped, tortuous, which allows maintaining normal blood supply during pronounced changes in the uterus during pregnancy and during contraction of its muscles during childbirth.
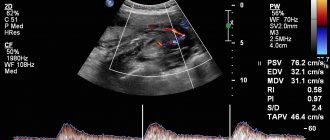
- The volume of blood circulation in the uterus during pregnancy increases tens of times, providing uteroplacental blood flow, which is carried out according to the principle of blood supply to vital organs and remains relatively optimal even under various stresses (blood loss, anemia). This ensures the survival of the fetus in extreme situations.
- The receptor system of the uterus changes: during pregnancy, the sensitivity of the uterus to stimulating factors decreases, before childbirth, the excitability of the uterus increases, some of the nervous structures are lost in order to reduce pain information from the uterus during childbirth.
With the appearance of the placenta, a pregnancy dominant arises in the cerebral cortex, which ensures clear coordination of the functions of all organs and systems in the interests of the developing fetus.
Women note a decrease in performance, increased drowsiness, or vice versa, they are irritated, they have nausea, drooling, periodic vomiting, which is classified as mild and the occurrence of which corresponds to the phase of functional changes in the nervous system.
Pregnant women have increased suggestibility and self-hypnosis, which is taken into account when conducting psychoprophylactic preparation for childbirth.
Phenomena of paresthesia, neuralgic pain, spasms of muscle groups, numbness of the fingers and other disorders may occur. Increased excitability of peripheral nerves is also manifested by increased knee reflexes.
With all this, sexual excitability decreases , and you, dear husbands, must be prepared for this. No need, under no circumstances!!! (remember about increased suggestibility and self-hypnosis) do not show your grievances that your wife is cold and inattentive to you, which means she has stopped loving you. She still loves you, she is already carrying your child and she has a dominant in her cerebral cortex - to endure pregnancy at all costs. And there is no escape from this.
- In a pregnant woman, the functions of some analyzers change - hearing, vision, smell!!! A pregnant woman's sense of smell can become so strong that the woman will react to the lightest (hardly perceptible) odors.
Please keep in mind, dear men, when a woman feels bad, feels sick, and the world is generally in shades of grey, for some reason unhappy thoughts come into her head, which can lead to a deterioration in her condition and, as a consequence, to termination of pregnancy.
During pregnancy, changes affect other organs as well.
The adrenal glands increase in size during pregnancy due to cortical hyperplasia, and the glucocorticoid and mineralocorticoid function of the adrenal glands increases accordingly.
Strengthening the function of the adrenal cortex during pregnancy is aimed at increasing protective and adaptive mechanisms, including during childbirth.
The thyroid gland increases in volume and function increases. Goiter in pregnant women is observed, especially in areas endemic for goiter (little iodine in soil and water) and hyperthyroidism without thyrotoxicosis. Strengthening the function of the thyroid gland is associated with the influence of placental hormones on it. Clinical thyrotoxicosis does not develop due to increased binding of free hormones by plasma proteins. The protein-bound form of the hormone is subsequently utilized by the fetus and the mother’s body, since the need for it increases with the development of pregnancy, before the onset of fetal thyroid function.
The parathyroid glands (calcium metabolism) undergo hypertrophy, their functional activity increases due to the increased need for calcium, which is a plastic material for the formation of the musculoskeletal system of the fetus. If there is insufficient intake or impaired absorption, the fetus receives calcium from the tissues of the mother’s body (bones, teeth), which can manifest itself as osteoporosis, fragility and dental caries. During pregnancy, the concentration of calcium in the blood increases. The content of phosphorus compounds, iron and a number of microelements (cobalt, iodine, manganese, copper) also decreases in the blood plasma. The deficiency of these substances is due to the needs of the fetus and increased metabolic reactions, the enzyme systems of which include some of the micro- and macroelements.
Pancreas – strengthening the function of the insulin-producing apparatus. As a result, carbohydrates are absorbed very well and are deposited in the mother’s liver and in the tissues of the fetus. Women with diabetes always give birth to large children due to the utilization of excess carbohydrates by the fetus. Some pregnant women experience glucosuria (sugar in the urine), which is not pathological and manifests itself with normal or even low carbohydrate levels in the blood.
The pituitary gland in pregnant women increases in volume and is difficult to fit in the sella turcica; hyperproduction of growth hormone (GH) is observed, which, penetrating the placenta, stimulates the growth of the embryo. This hormone also affects the lactogenic function of the mammary gland, causing in some cases an enlargement of the nose, lips, and fingers.
Management of pregnancy in women with heart disease
Patients with a significant cardiovascular history should take a responsible approach to planning pregnancy. Even in the absence of any complaints, examination by a cardiologist is recommended. It is this doctor who decides the issue of prolonging pregnancy, choosing management tactics and method of delivery.
Preparing for pregnancy
The expectant mother should undergo examination to identify possible diseases. You should not be afraid of visiting a doctor and assume that pregnancy is a condition that cures all diseases, and the very fact of its occurrence automatically recognizes the woman as healthy. To assess the risk you must go through:
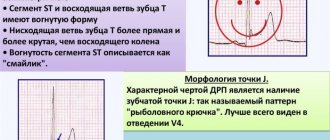
- ECG;
- EchoCS;
- stress tests to assess heart function;
- MRI for aortic lesions.
If you suspect hereditary diseases, you should contact a medical geneticist. A full examination will show whether it is possible to plan a pregnancy.
Pregnancy due to CVD
If pregnancy occurs in a woman with damage to the heart or blood vessels, the cardiologist conducts an ongoing examination to decide whether it can be saved. Thus, indications for interruption are conditions with severe circulatory disorders and an active rheumatic process:
- atrial fibrillation due to heart disease;
- aortic valve insufficiency;
- aortic valve stenosis with an increase in heart size and impaired myocardial function;
- mitral valve insufficiency with the development of circulatory failure, arrhythmia, active rheumatic process;
- previous heart surgery (individual);
- exacerbation of rheumatism with severe manifestations;
- severe cardiomyopathy;
- severe congenital defects (patent ductus arteriosus, pulmonary stenosis, ventricular septal defect).
If a council of specialists allows a woman to bear a child, she is subject to joint supervision by an obstetrician-gynecologist, a therapist and a cardiologist. During pregnancy, it is necessary to regularly evaluate the condition of the heart, and if the condition worsens, prescribe drug therapy. Treatment is carried out on an outpatient basis or in a hospital setting. Cardiologists recommend a minimum of 3 planned hospitalizations:
- in the 1st trimester to decide whether to continue the pregnancy;
- at a period of 228-32 weeks for preventive treatment;
- at 36 weeks to choose the method of delivery.
Effect of pregnancy on kidney function
Renal blood flow increases and glomerular filtration increases (maximum in mid-pregnancy) - associated with the excretion of metabolic products of the woman and the fetus.
The permeability of the kidneys to protein and carbohydrates increases: proteinuria (protein in the urine), glucosuria. The excretion of 140 mg/day of glucose in the urine is considered the upper limit of the physiological norm. Peak glucose secretion was detected at 9 months of pregnancy.
The peristaltic function of the ureters is sharply suppressed, as a result of which they expand and urine is retained in them. Atony of the ureters leads to impaired drainage of urine from the pelvis, which creates favorable conditions for the development of pyelonephritis in pregnant women. In the postpartum period, these phenomena soon disappear.
How long does CTG last?
The procedure lasts from 30 to 60 minutes depending on the baby’s activity. After 32 weeks, the fetus is characterized by periods of sleep and wakefulness. The active state lasts 50-60 minutes, while the calm state lasts 20-30 minutes. When assessing cardiotocography, the leading period is the period of fetal wakefulness. Therefore, the duration of the study may vary.
Effect of pregnancy on liver function
The liver during pregnancy is in a state of high functional tension. However, in healthy women during the physiological course of pregnancy, the functioning of the liver is not impaired.
Noted:
- slight increase in liver size in the absence of pronounced histological changes;
- there is a decrease in the antitoxic function of the liver;
- the level of protein in the blood serum decreases, by the time of childbirth it can reach 60 g/l;
- the result of changes in the composition of serum proteins is an increase in ESR;
- blood clotting and fibrinolysis changes. These changes help increase blood clotting ability.
In what cases should you sound the alarm?
You should consult a doctor if changes in pulse are accompanied by:
- frequent dizziness;
- constant nausea;
- general weakness, apathy;
- breathing problems;
- fainting.
These symptoms are cause for alarm and all require medical attention. It is possible that the woman has encountered these problems before, and pregnancy provoked their aggravation. In any case, if alarming symptoms appear, the expectant mother is recommended to visit not only a gynecologist, but also a neurologist, cardiologist and endocrinologist.
Function of the gastrointestinal tract
There are changes in the function of the gastrointestinal tract. A number of women experience a perversion of taste sensations such as aversion to certain types of food (meat, fats), the appearance of taste whims (the desire to eat even clay, chalk), an increase in appetite, and in some cases its decrease. Due to a decrease in gastric secretion, the evacuation ability of the stomach slows down. Intestinal function in pregnant women is characterized by decreased tone and decreased intestinal motility, which determines the tendency to bloating, constipation, and hemorrhoids.
Metabolism
Characterized by an increase in metabolic processes.
- Basal metabolism and oxygen consumption increase, especially in the second half of pregnancy and childbirth.
- Changes in water-electrolyte metabolism are characterized by fluids.
- Carbohydrate metabolism is characterized by an increase in glucose in the blood, and when the body is overloaded with carbohydrates, it appears in the urine (glucosuria). During pregnancy, latent forms of diabetes mellitus appear.
- The content of fats and cholesterol in the blood increases, but no pathological manifestation of this condition is observed. There is increased fat deposition with a characteristic distribution in the subcutaneous tissue, mammary glands, lower abdomen, thighs, and buttocks. Fats are used to build the tissues of the body of the mother and fetus, and are also energy material.
- During pregnancy, there is an increased need for vitamins (A, B, D, C, E, K, PP).
- In some women, due to pregnancy, sweating increases and the discharge of liquid salts from the vagina, which are a mixture of mucus and transudate of the vasculature of the genital organs, increases.
The variety of external and internal changes in a woman’s body increases with increasing pregnancy, are characteristic only of the state of pregnancy and are aimed at creating optimal conditions for the development of the fetus and the course of labor.
That is why the norms characteristic of non-pregnant women cannot be transferred to pregnant women.
The norm of pregnancy is considered to be the average statistical indicators of functional tests characteristic of uncomplicated development of pregnancy.
Each trimester of pregnancy has its own norms. Knowledge of the norms allows you to avoid unreasonable actions that can cause a violation of the physiological balance established between the fetus and the mother’s body.
What to do?
Regardless of whether the expectant mother’s heart rate is high or low, if she does not complain of feeling unwell, this does not mean that nothing needs to be done. You can normalize your heart rate using the following simple recommendations.
Tips for tachycardia:
- Maintaining a daily routine. Pay special attention to daytime rest and a good night's sleep. Read more about how to sleep during pregnancy to feel great →
- Proper nutrition. Avoid overeating and tonic drinks - strong tea and coffee.
- Lack of strong physical activity.
- With the permission of a doctor, take sedatives of natural origin, for example, motherwort.
Tips for bradycardia:
- Correction of the daily routine, observing alternating periods of activity and rest. Avoiding overwork.
- Balanced diet, avoiding heavy foods.
- Carrying out gymnastics for expectant mothers to activate cardiac activity.
- Daily walks in the air.
Women are interested in pulse not only in the context of their health. Sometimes they ask how to determine pregnancy by the pulse? This is not difficult to do, but the reliability of the result is questionable: you need to place your hand 7-8 cm below your navel and listen to your feelings. It is believed that if there is pregnancy, this place will pulsate.
During pregnancy, changes in heartbeat are indeed possible. Most often this is not dangerous and is a physiological norm.
In any case, during each scheduled visit to the antenatal clinic, the doctor must monitor the pressure and pulse of pregnant women, so it is almost impossible to miss the occurrence of a problem. If there are any deviations, the specialist will prescribe an additional examination to prevent pregnancy complications.
Author: Olga Rogozhkina, obstetrician-gynecologist, especially for Mama66.ru