What is angina
Angina pectoris is a specific pain syndrome characteristic of myocardial ischemia. There are stable and unstable angina, as well as exertional and resting angina.
Stable angina is one that occurs in an unchanged form. We can say that this is a “habitual” symptomatology for a person. However, this situation cannot be considered the norm: serious treatment is required, often surgical.
Unstable angina is either angina that has arisen for the first time, or one where the nature of the pain syndrome and sensations differs significantly from the usual state. This is an extremely dangerous condition, fraught with a high risk of developing a heart attack, and requiring an immediate call to the ambulance.
Angina pectoris is one of the manifestations of atherosclerosis and coronary heart disease, which is manifested by severe chest pain during physical activity and stress. However, chest pain is not always a manifestation of angina.
It is important to note symptoms such as:
- squeezing, pressing or burning nature of the attack;
- impact under the left shoulder blade or in the arm, neck, lower jaw;
- lack of oxygen and dizziness;
- obvious interruptions in the functioning of the heart: fluctuations in heart rate and blood pressure.
Most often, pain with angina pectoris manifests itself during walking, climbing stairs, physical effort, and stress. The attack lasts from 1 to 15-20 minutes and is facilitated by taking nitroglycerin. Symptoms may appear all at once or separately.
Angina at rest, unlike the previous type, is characterized by a sudden and prolonged attack, which is activated without external provoking factors, sometimes during sleep. In this case, we can add to the main symptoms: an uncontrollable panic attack, a pronounced feeling of suffocation, a violation of the autonomic functions of the body. We will write more about this type of angina in the following articles.
In addition to extremely unpleasant symptoms, such manifestations indicate a high risk of myocardial infarction, as well as the development of heart failure.
Cardiovascular diseases claim half of human lives - exactly the same as all other causes combined.
Angina pectoris
Angina pectoris is translated from Latin as “compression of the heart,” an outdated synonym for the name “angina pectoris.” Angina pectoris is manifested by severe pain or discomfort in the chest area. An attack occurs due to a temporary lack of oxygen to the working heart muscle.
The sensations of patients with angina pectoris can be described as follows: squeezing or pressing pain behind the sternum, often radiating to the shoulder, arm, neck or jaw. As a rule, the pain lasts no more than 10-15 minutes and goes away after taking nitroglycerin under the tongue or resting. At the same time, various patients experienced angina attacks that lasted both 30 seconds and 30 minutes.
Angina pectoris is the leading symptom of coronary heart disease (CHD), which develops as a result of narrowing or blockage of the blood vessels of the heart. The most dangerous manifestation of coronary heart disease is myocardial infarction. In some patients, it is preceded by frequent attacks of angina pectoris for 10–15 days. In other patients, a heart attack develops without warning - suddenly.
Unlike angina, a heart attack causes irreversible changes in the heart tissue due to the complete cessation of blood supply to this area. Chest pain during a heart attack is more pronounced, lasts longer and does not go away after rest or taking nitroglycerin under the tongue. During a heart attack, nausea, severe weakness and sweating are also observed.
It should be remembered that in cases where angina episodes become longer, occur more often and occur even during rest, the risk of developing a heart attack increases. To avoid heart disaster, you need to prevent angina attacks. This process is quite complex, requires patience and painstaking execution and covers all areas of life: from work and rest to taking medications.
Work and rest schedule
The heart does not like heavy physical activity and overwork. Therefore, plan in advance everything you will do tomorrow. This will allow you to evenly distribute the load throughout the day.
Don't go to bed late, preferably at 10-11 p.m., and don't sleep long, get up at 7-9 a.m.
Try to be outside every day so that your heart receives oxygen, and walk at a moderate pace (when walking, contractions of the veins in your legs help your heart pump blood, reducing the load on it).
Constantly lying on the bed is as harmful as intense physical activity. So don't lie around.
When working at the dacha, do not carry out heavy work: do not carry logs and full buckets, do not stand bent over for a long time, do not work in the beds without breaks. Remember that a dacha is a place of relaxation, not hard labor. The excessive effort invested may no longer be necessary.
Nutrition
Patients with coronary heart disease must follow a diet that limits fluids, table salt, carbohydrates, spicy foods, coffee and alcohol.
Don't drink a lot and often, it's better to eat some fruit. Remember, water is found not only in tea, but also in soups and other foods.
Try to count your urine output: the amount of fluid consumed should not exceed the amount of urine excreted per day.
Limit your salt intake because... it retains water in the body and puts even more strain on the heart. Prepare food without salt, add salt immediately before eating, in small quantities. Do not eat various homemade pickles and salted fish. This often provokes high blood pressure and angina attacks.
Limit your carbohydrate intake: sugar, white bread and pastries, pasta. Eliminate fatty meat and fish, limit butter. Eat low-fat dairy products, vegetables, fruits. Baked potatoes, dried apricots, raisins and other dried fruits are very healthy.
Try not to eat spicy foods, smoked meats, sausages, or foods fried in oil. Boiled meat dishes are much healthier.
You should completely forget about alcohol and coffee. These are direct conductors to a heart attack.
Smoking
If you smoke, try to get rid of this habit as soon as possible. Statistics show that 50% of people quit smoking after the first heart attack, another 30% after the second, and 99% do not smoke after the third heart attack. Why wait for him? Quit now! If you are still unable to do this, then reduce the number of cigarettes you smoke to a minimum. It is not difficult!
Blood pressure control
Due to the fact that the vast majority of patients with coronary heart disease suffer from hypertension, you need to monitor your blood pressure daily. If you don’t yet have a device to measure it, then buy one. Life is worth more than its cost! It is necessary to measure blood pressure 2 times a day: in the morning and in the evening, before taking medications, and also in cases of poor health: headaches, chest pain, palpitations.
Taking medications
All patients suffering from coronary artery disease must daily, meticulously take medications prescribed by the local therapist and other specialists. If they have not yet been prescribed to you, do not hesitate to contact the clinic!
The medications must be taken daily, not occasionally (!), and as many times as prescribed by your doctor. You cannot stop or prescribe medications on your own. To cancel or replace them, consult your doctor, not your neighbor. Try to keep the intervals between taking medications even, a properly organized daily routine will help. Take blood pressure-lowering medications only after measuring your blood pressure: if it is below your working pressure, reduce the dose, if it is higher, increase it.
Try not to swallow handfuls of tablets, but spread them out throughout the day.
Before going outside or exercising, take a long-acting nitrate as prescribed by your doctor.
Causes of angina
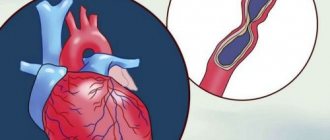
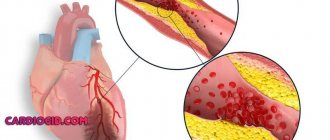
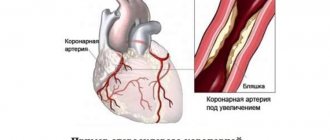
The cause of angina is the partial blocking of the lumen of the arteries by atherosclerotic plaques, resulting in severe oxygen starvation of the heart cells, which causes pain. An additional role is played by vasospasm, which can be provoked, for example, by nervous strain or sudden exposure to cold.
It is the presence of atherosclerotic plaques that is the leading factor in the development of angina pectoris. The development of coronary heart disease is a complex and multicomponent process, which is provoked and accelerated due to risk factors:
- arterial hypertension,
- smoking, obesity,
- cholesterol metabolism disorder,
- diabetes,
- low physical activity and poor nutrition.
In the case of atherosclerosis, angina begins to manifest itself when an atherosclerotic plaque fills the artery by more than 50% - preventing the normal passage of blood through the heart and, accordingly, the saturation of the heart muscle with oxygen. This leads to the development of an imbalance in the functioning of the heart.
With physical and psycho-emotional stress, the situation worsens. The heart begins to work more actively - it contracts more often and stronger. In this state, it requires more oxygen and nutrients. However, due to vasoconstriction, this need is not satisfied, which leads to oxygen starvation and, as a result, pain.
We feel pain thanks to the instinct of self-preservation. She is a kind of alarm signal. Therefore, any pain attack is a rational reason to consult a doctor.
Risk factors and their control
Angina pectoris and the disease that causes it require not only the fastest possible treatment, but also control of risk factors. These include:
- Hyperlipidemia - imbalance in cholesterol metabolism. It is characterized by an increased concentration of low-density lipoproteins and fatty acids - triglycerides. And also by lowering the level of high-density lipoproteins - “good” cholesterol.
It is observed in most patients with angina pectoris. Reducing cholesterol levels in the body helps reduce the number of attacks.
- Obesity - characterized by a body mass index of more than 26 and, often, occurs due to constant poor nutrition: consumption of high-calorie foods high in animal fats, cholesterol and “fast” carbohydrates, such as sugar and flour. And, on the contrary, a lack of vegetables, fruits, whole grains, legumes, and herbs in the diet.
In addition, large body weight increases the load on the heart, increasing the risk of an attack. To control this factor, it is necessary to adhere to the principles of rational or therapeutic nutrition: limit the consumption of cholesterol, animal fats, processed foods and salt. Increase your consumption of vegetables, fruits and other whole plant foods containing fiber, natural antioxidants, polyphenols, and flavonoids.
Excess body weight is usually just the “tip of the iceberg”. This is a manifestation of serious imbalances in the functioning of the body.
- Physical inactivity - insufficient physical activity, combined with poor nutrition, contributes to the risk of obesity and cholesterol accumulation. Together, these factors contribute to the development and frequency of angina pectoris.
- Arterial hypertension - is a frequent companion to coronary heart disease, which, in itself, implies oxygen deficiency of the myocardium. When blood pressure rises, myocardial tension occurs, causing the heart to have an even greater need for oxygen. This provokes an attack of angina pectoris.
Controlling blood pressure will help keep the heart and blood vessels relatively calm - reducing the frequency and power of attacks.
- Anemia is not a risk factor, but a condition that aggravates the course and makes it difficult to control IHD. It is characterized by a decreased level of hemoglobin and a general weakening of the body. This results in the impossibility of sufficiently supplying the heart with oxygen. Controlling the normal level of hemoglobin in the blood helps alleviate the course of the disease: for women the norm is 120-150 g/l, for men - 135-165 g/l.
- Tobacco addiction - smoking increases several risk factors at once: it causes oxygen starvation, increases blood pressure and causes spasms of the arteries. The habit harms a healthy body, and in the presence of atherosclerosis it leads to early manifestations of angina pectoris and significantly increases the risk of acute myocardial infarction.
- Diabetes mellitus type 2. This disease seriously worsens the course and prognosis of IHD. We will devote a separate article to this condition, but for now we draw attention to it as a serious risk factor.
The combination of 2 or more items from the list, even weakly expressed ones, increases oxygen starvation of the heart, and, accordingly, the risk of developing and the severity of symptoms of angina pectoris. The presence of risk factors should be taken into account when determining treatment tactics and secondary prevention of angina pectoris.
Coronary heart disease, angina pectoris and rules of life
Coronary heart disease, angina pectoris and rules of lifeUsually a well-functioning heart is practically undisturbed, but there may come a time when the heart suddenly makes itself felt.
Most often this is associated with the development of a serious disease – coronary heart disease.
What is coronary heart disease?
IHD - coronary heart disease (angina pectoris, unstable angina, myocardial infarction) - is a consequence of narrowing and blockage of the main arteries of the heart with atherosclerotic plaques. Over time, there are more and more of them, and when the lumen of the vessel is blocked by 50% or more, difficulty in blood flow occurs. As a result, the delivery of oxygen and nutrients to the heart muscle decreases, oxygen starvation (hypoxia) develops, which leads to myocardial ischemia. The larger the size of the atherosclerotic plaque, the smaller the lumen of the vessel and the less blood flows through it, the more pronounced the myocardial hypoxia, which means the more pronounced ischemia (angina).
If, due to physical activity or emotional stress, you experience pain or a feeling of pressure or heaviness behind the sternum, you have a high probability of having angina pectoris (formerly called angina pectoris).
It is strongly recommended that you be examined by a cardiologist or physician.
Know that an attack of angina can be triggered by exercise, emotional stress, cold air and smoking.
Under the influence of these external influences, the pulse (heart rate) increases and blood pressure (BP) increases, which entails an increase in the myocardial oxygen demand against the background of a decrease in its delivery to the heart cells, thus developing myocardial ischemia, which the patient feels as angina pectoris.
How to diagnose angina?
The diagnosis of coronary artery disease and angina is made on the basis of a thorough survey and complaints.
To confirm the diagnosis and clarify the severity of the disease, additional methods are needed:
— taking an electrocardiogram (ECG) at rest and at the height of an attack
— carrying out stress tests (treadle test or test on a bicycle ergometer)
— according to indications (in case of high pulse, abnormal heart rhythm), 24-hour ECG recording is performed (Holter ECG monitoring)
— Sometimes coronary angiography (contrast study of the arteries of the heart) is required.
Warning signs of angina development:
— sudden discomfort, pain, or burning sensation;
— Pain can be triggered by walking, any physical activity, anxiety, emotional stress, cold air, smoking, less often pain appears at rest;
— pain most often occurs behind the sternum, but can radiate (radiate) to the left arm, left half of the lower jaw, teeth, shoulder, back or upper abdomen;
— pain occurs predominantly in the form of mild attacks (3-5 minutes), attacks can be repeated with varying frequency;
— usually the pain disappears 2-3 minutes after stopping walking or other physical activity, or taking nitroglycerin;
— attacks of angina may intensify with increased blood pressure, smoking, late intake or withdrawal of medications.
Types of angina:
V If your attacks appear during the day after the same load, with the same frequency and are of the same type, then you have stable angina.
V If your attacks become more frequent, occur with less stress and even at rest, become stronger, more severe and last longer, and are poorly controlled by the usual dose of nitroglycerin, then you should suspect unstable angina .
You need urgent medical consultation.
V If the pain becomes more intense and lasts for more than 15 minutes, repeats in waves at rest and does not go away after taking three nitroglycerin tablets, there is severe weakness and a feeling of fear, blood pressure and pulse fluctuate sharply, then you should suspect myocardial infarction. In this situation, urgent consultation with a doctor and immediate call for emergency medical assistance is necessary!
To improve your well-being and prevent the development or further progression of IHD, determine whether you have risk factors.
Factors that increase your risk of developing CHD
(check your risk factors):
Factors you cannot control
[] age/gender: men over 45 years old, women over 55 years old
[] early development of IHD in close relatives: - in men under 55 years of age, - in women under 65 years of age
Factors you can control
[] elevated blood pressure
[] smoking
[] elevated blood cholesterol levels
[] elevated blood glucose levels (diabetes)
[] excessive alcohol consumption
[] passive lifestyle
[] overweight
[] stressful situations
Inform your doctor about the risk factors you have identified and ask for advice on what you should do to correct them and subsequently control them well.
Treatment of coronary artery disease and angina has two goals:
the first is to improve the prognosis and prevent the occurrence of serious complications - myocardial infarction, sudden death - and prolong life;
the second is to reduce the severity of clinical symptoms - the frequency and intensity of angina attacks and, thus, improve the quality of life.
You should:
* learn to stop an attack of angina:
— interrupt the load, stop,
— take nitroglycerin under the tongue;
* be informed:
— about the potential undesirable effects of nitrates,
— about the possibility of developing hypotension after taking nitroglycerin;
— about the need to immediately call an ambulance if an angina attack persists at rest and/or is not relieved by nitroglycerin for more than 15-20 minutes;
— about the nature of angina, the mechanism of its development and the significance of this disease in the prognosis of life and recommended methods of treatment and prevention,
* to prevent an attack of angina, take nitrates (nitroglycerin) before exercise, which usually leads to angina.
How can you reduce the high likelihood of progression of coronary artery disease, angina,
as well as the development of serious cardiovascular complications
(myocardial infarction, unstable angina, sudden death, heart failure, cerebral stroke)?
STEP 1 relieving an attack of angina
If you have an angina attack:
V stop physical activity, stop walking, sit down, calm down and relax,
V put one nitroglycerin tablet under the tongue or use nitroglycerin in the form of a spray,
V Before taking nitroglycerin, you should sit down, because the drug may cause dizziness or decreased blood pressure,
V crush the nitroglycerin tablet and let the tablet dissolve completely; if the pain does not stop, then after 3-5 minutes repeat taking nitroglycerin either in the form of a tablet (up to 3 tablets) or in the form of a spray (spraying into the mouth up to 3 times)
V If an attack of angina cannot be relieved within 15 minutes after taking 3 tablets of nitroglycerin, you should immediately seek emergency medical help, and immediately chew 1 tablet of aspirin with water (aspirin prevents the formation of a blood clot). You may be developing a myocardial infarction!
REMEMBER!
You should always have a sufficient number of nitroglycerin tablets with you and they should always be at hand, no matter where you are at the moment!
STEP 2 regular blood pressure checks
People with elevated blood pressure levels and untreated developed myocardial infarction in 68 out of 100 cases and cerebral stroke in 75 out of 100 cases.
Monitor blood pressure levels carefully:
* at least once a year – with a single unstable increase in blood pressure discovered by chance;
* at least once a month - if you feel well, but have a tendency to frequently increase blood pressure;
* at least 2 times a day – in case of exacerbation, poor health, stable increase in blood pressure
Aim for a blood pressure level below 140/90 mmHg.
If you have suffered a myocardial infarction, suffer from angina pectoris, intermittent claudication, then strive for a lower blood pressure level - below 130/80 mm Hg.
In people with good blood pressure control:
* 42% fewer brain strokes;
* 20% less lethal and other serious cardiovascular complications (myocardial infarction, unstable angina, sudden death);
* 50% less heart failure;
* 14% fewer deaths from any other non-cardiac cause.
STEP 3 regular monitoring of cholesterol levels in the blood
Check your blood cholesterol levels and, if they are elevated, discuss with your doctor the possibility of taking cholesterol-lowering medications.
Criteria for optimal lipid levels in the majority of patients with coronary artery disease, patients who have had myocardial infarction, or surgery on the vessels of the heart, carotid arteries or arteries of the lower extremities:
* Total cholesterol - less than 4.0 mmol/l
* LDL cholesterol – less than 1.8 mmol/l
* Triglycerides – less than 1.7 mmol/l
* HDL cholesterol – for Men – 1.0 mmol/l or more
* HDL cholesterol - for Women - 1.2 mmol/l or more
STEP 4 heart rate control
In case of coronary artery disease, angina pectoris, or after a myocardial infarction, it is very important to control the pulse rate (heartbeat).
The optimal heart rate should be between 55-60 beats per minute.
This optimal heart rate is usually maintained with special medications prescribed by the attending physician.
STEP 5 proper nutrition
Change your eating pattern: eat healthy foods with less animal fat (60-105 g/day for men and 45-75 g/day for women) and rich in vegetables, fruits, complex carbohydrates, dietary fiber, fish.
Exclude from the diet: fatty meats, strong meat broths, any fat, sausages (even the so-called doctor's ones!), sausages, ready-made dumplings, canned meat, mayonnaise, internal organs of animals, brains, caviar, butter, hard margarine, fatty cottage cheese , cream cakes, creamy ice cream.
STEP 6 more movements
Move more and be physically active (at least 30 minutes of moderate exercise on most days of the week). If you have heart problems and are taking medications, talk to your doctor before changing your level of physical activity.
If you have been physically inactive for a long time, or if you are over 40 years old, or have angina pectoris, then the mode and level of physical activity should be determined by your doctor or physical therapy specialist, determining the pulse safety zone.
Physical activity is useful: aerobic, dynamic and moderate intensity - cycling, measured walking, swimming, team sports (football, volleyball), etc.
Optimal training walking tempo (number of steps per minute) depending on physical load tolerance (according to a load test on a bicycle ergometer)
Amount of load performed
during bicycle ergometer test, W 50 75 100 125
Function class
angina III II II I
Optimal pace
number of steps per minute 99-102 105-108 111-114 118-121
(or average) or 100 or 105 or 110 or 120
STEP 7 monitor the status of other risk factors
> Monitor your weight and measure your waist circumference (a waist circumference greater than 102 cm for men and greater than 88 cm for women indicates abdominal obesity, which is associated with a risk of cardiovascular complications).
> Stop smoking.
> Learn to control your psycho-emotional stress (avoid conflict situations, devote time to auto-training and relaxation methods).
> Maintain normal blood glucose levels: < 6 mmol/L (110 mg/dL)
STEP 8 Take medications prescribed by your doctor regularly
Today, the doctor has at his disposal a sufficient number of highly effective and safe drugs to reduce high blood pressure, prevent angina pectoris and prevent the development of serious cardiovascular complications.
REMEMBER!
Interruptions in taking medications reduce the effectiveness of preventing the development of myocardial infarction, unstable angina, and heart failure.
For the treatment of coronary artery disease and angina pectoris, different classes of medications are used today, the action of which is aimed at preventing the development of myocardial ischemia and angina attacks, vascular thrombosis, preventing the progression of atherosclerosis, reducing blood pressure and pulse rate (heart rate).
Take medication as directed by your doctor!
If the disease, despite active drug therapy, progresses, it is necessary to use modern interventional and surgical methods to restore blood supply to the myocardium:
V balloon angioplasty – expansion of the vessel at the site of stenosis by inflating the balloon
V stenting of the coronary arteries - installation of a special stent (tube) that allows for a long time to expand the artery of the heart and ensure normal blood flow
V coronary artery bypass grafting is used for a certain localization of atheromatous plaque and significant and multiple narrowing of the coronary vessel, when the first two methods are not effective
MAIN!
Treatment of coronary heart disease through lifestyle changes and highly effective medications prescribed by a doctor must be constant, long-term and daily.
STEP 9 keep a self-monitoring diary
A self-monitoring diary must be kept in order to promptly notice negative changes in the course of the disease and immediately contact your doctor.
The diary should record: blood pressure level, pulse rate, number of angina attacks, amount of nitroglycerin in the form of tablets or spray inhalations that were taken to relieve (relieve) an angina attack or prophylactically, for example, before physical activity, going outside to prevent it development.
The diary will allow you and your attending physician to evaluate the effectiveness of treatment, prevent exacerbation of the disease and, if necessary, correct therapy.
IF YOU FOLLOW THESE RULES AND MANAGE YOUR LIFE SMARTLY, YOUR ILLNESS WILL ALWAYS BE UNDER GOOD CONTROL!
Diagnosis of angina pectoris
To diagnose angina pectoris, as well as exclude other possible diseases, complaints and the nature of pain are analyzed, laboratory blood tests and a functional examination of the heart are performed, and the patient’s physical condition is analyzed.
It is also important to determine the severity and severity of the process. To do this, if a diagnosis of acute coronary syndrome is made, a study of the vascular bed of the heart is performed - coronary angiography. Based on the results, the question of surgery or intravascular intervention is decided.
Laboratory blood diagnostics help determine the level of:
- total cholesterol and lipid fractions,
- high and low density lipoproteins,
- triglycerides,
- creatine kinase,
- glucose,
- markers of systemic inflammation (SII),
- indicators of the coagulation system - coagulograms,
- electrolytes,
- troponin - in acute situations.
Particular attention in the study is paid to the presence of cardiac troponins I and T - markers that indicate myocardial damage. Their presence confirms that the patient is suffering a microinfarction or acute myocardial infarction.
Functional research methods allow you to determine the condition of the heart:
- ECG - examination at the peak of an angina attack determines conduction and rhythm disturbances. Signs of myocardial oxygen starvation may also be detected.
- Daily ECG monitoring - records the level of oxygen starvation during an attack of angina, heart rate, arrhythmia. Indicators help determine the specific diagnosis and stage of the disease.
- EchoCG - reveals local ischemic changes and disorders of myocardial contractility.
- Bicycle ergometry or treadmill - determines the maximum possible physical activity for the patient without the threat of developing ischemia. The load is set using an exercise bike or treadmill, and the results are recorded by an ECG device.
- Stress echocardiography (Stress-ECHO) is a study of myocardial contractility using the ultrasound method, under conditions of dosed physical activity. At the same time, an ECG is recorded. Allows you to make a primary diagnosis of IHD and clarify indications for surgical treatment.
For a detailed study of the vascular bed of the heart, the following are used:
- Coronary angiography is an X-ray method in which a contrast agent is injected into the arteries of the heart using a special catheter.
- multislice computed tomography is a type of computed tomography in which X-ray “slices” of the heart and blood vessels are obtained at high speed. More than 100 such “slices” can be performed between contractions of the heart chambers.
These studies allow us to obtain information about the state of the vascular bed of the heart: which arteries are passable, which are completely or partially blocked, and in what place. Based on the information received, the doctor makes a decision about whether the patient has coronary artery disease, the need for surgical intervention and the timing of treatment.
Treatment of angina
Angina pectoris is an accompanying factor of coronary heart disease, so the main fight must be waged against it. Treatment of angina pectoris is aimed at relieving and preventing attacks and complications.
The first priority when an attack occurs is to take nitroglycerin. It helps relieve pain. If the attack does not stop, nitroglycerin can be used again. Drug therapy involves your doctor prescribing anti-ischemic drugs that help the heart cope with low oxygen levels. Anti-sclerotic drugs, antioxidants and antiplatelet agents are also prescribed.
Based on the diagnosis, a decision is made on additional treatment for cardiac conduction and rhythm disorders. For angina pectoris, surgical intervention is often prescribed: balloon angioplasty, stenting, coronary artery bypass grafting.
Symptoms, course
With angina, pain is always characterized by the following symptoms:
- has the nature of an attack, that is, it has a clearly defined time of onset and cessation, subsidence;
- occurs under certain conditions and circumstances;
- begins to subside or completely stops under the influence of nitroglycerin (1 - 3 minutes after its sublingual administration).
Conditions for the occurrence of an attack of angina pectoris: most often - walking (pain when accelerating, when climbing a mountain, during a sharp headwind, when walking after eating or with a heavy load), but also other physical effort, and/or significant emotional stress . The conditioning of pain by physical effort is manifested in the fact that as it continues or increases, the intensity of the pain inevitably increases, and when the effort stops, the pain subsides or disappears within a few minutes.
The above three features of pain are sufficient to make a clinical diagnosis of an attack of angina and to distinguish it from various pain sensations in the heart and generally in the chest that are not angina.
It is often possible to recognize angina pectoris at the first visit of the patient, while to reject this diagnosis requires observation of the course of the disease and analysis of data from repeated questions and examinations of the patient. The following signs complement the clinical characteristics of angina, but their absence does not exclude this diagnosis:
- localization of pain behind the sternum (most typical!), rarely - in the neck, in the lower jaw and teeth, in the arms, in the shoulder girdle and shoulder blade (usually on the left), in the heart area;
- the nature of the pain is pressing, squeezing, less often - burning (like heartburn) or the sensation of a foreign body in the chest (sometimes the patient may experience not pain, but a painful sensation behind the sternum and then he denies the presence of pain itself);
- simultaneous with an attack of increased blood pressure, pallor, perspiration, fluctuations in pulse rate, the appearance of extrasystoles.
All this characterizes angina pectoris. The thoroughness of the medical questioning determines the timeliness and correctness of the diagnosis of the disease. It should be borne in mind that often a patient, experiencing sensations typical of angina, does not report them to the doctor as “not related to the heart,” or, on the contrary, focuses on diagnostically minor sensations “in the area of the heart.”
Angina at rest, in contrast to steiocardia at exertion, occurs independently of physical effort, more often at night, but otherwise retains all the features of a severe attack of angina pectoris and is often accompanied by a feeling of lack of air and suffocation.
In most patients, the course of angina is characterized by relative stability. This is understood as a certain duration of occurrence of signs of angina, attacks of which during this period have changed little in frequency and strength, occur when the same or similar conditions occur, are absent outside of these conditions and subside under conditions of rest (angina pectoris) or after taking nitroglycerin. The intensity of stable angina is classified by the so-called functional class (FC).
IFC includes persons whose stable angina is manifested by rare attacks caused only by excessive physical stress. If attacks of stable angina pectoris also occur during normal loads, although not always, such angina is classified as FC II, and in the case of attacks during light (domestic) loads, it is classified as FC III. IV FC is recorded in patients with attacks with minimal loads, and sometimes in their absence.
Angina pectoris should alert the doctor if: an attack occurs for the first time, but especially if attacks that occur for the first time become more frequent and intensify from the very first weeks of the illness; the course of angina pectoris loses its stability: the frequency of attacks increases, they occur in conditions other than before (at lower loads, stress), they also appear outside of stress (at rest, in the early morning), as if they move from FC I - II to FC III - IV FC; that is, the course of angina has changed, acquiring significantly new characteristics.
ECG changes (decreased ST segment, T wave inversion, arrhythmias), as well as a slight increase in the activity of serum enzymes (CPK, LDH, LDH1, AST), are usually absent in such cases, but the presence of these signs additionally confirms the instability of angina. Pre-infarction angina does not always result in heart attack (the probability of developing a heart attack is about 30%); this must be taken into account in clinical diagnosis.
Occasionally, the so-called variant (vasospastic) form of angina occurs, characterized by the spontaneous nature of the attack, sharp rises in the ST segment recorded on the ECG, refractoriness to beta blockers (anaprilin and obzidan), but sensitivity to calcium ion antagonists (verapamil, phenigidine, corinfar).
The basis for the diagnosis of any of the forms and variants of the course of angina pectoris is a correctly constructed and carefully conducted questioning of the patient. In unclear cases, a test with physical activity (bicycle ergometer test) is performed in order to identify hidden coronary insufficiency. The tactics for establishing a diagnosis are determined by the following schematic sequence of solving the main issues:
- Is the nature of the pain coronary (anginal)?
- Are there signs of pre-infarction angina?
- Is the current exacerbation during coronary heart disease related to the influence of extracardiac (concomitant) diseases?
Only a convincingly reasoned negative answer to the first of three questions gives the right to search for another cause (source) of pain: the discovery of another disease in a patient as the source of his pain cannot exclude the presence of simultaneous attacks of angina pectoris as a manifestation of coronary heart disease. About pain in the heart area of a non-anginal nature ( see Cardialgia.)
Complications of angina pectoris itself are not observed if it does not become an expression of the progression of cardiosclerosis and if it does not turn out to be the first manifestation of a developing myocardial infarction. Therefore, an attack of angina pectoris that lasts for 20 - 30 minutes, as well as unstable angina pectoris, require an electrocardiographic examination in the next few hours (days) and determination of the presence of reactive changes in the activity of a number of enzymes in the blood, body temperature ( see Myocardial infarction
).