Bockeria L.A., Ermolenko M.L., Bayramukova M.Kh., Shinbaeva N.A. NC SSH named after. A.N. Bakulev RAMS. Moscow
Coronary heart disease (CHD) remains the leading cause of disability and mortality among adults worldwide. Despite the successes of traditional methods of drug and surgical treatment of coronary artery disease, there remains a number of patients with angina pectoris in whom these methods are ineffective, inadequate or impossible to apply. This predetermined the relevance of the development of new treatment methods, such as laser transmyocardial revascularization, the use of cellular technologies and drugs that change myocardial metabolism, etc. One of the new, most interesting, non-invasive approaches is the method of external counterpulsation (ECP).
The beginning of the development of theoretical prerequisites for the use of counterpulsation can be considered the end of the 50s. NCP was studied as a means of circulatory support in cardiogenic shock, being an alternative to intra-aortic counterpulsation, which made it possible to achieve an increase in perfusion pressure in the coronary arteries during diastole and a decrease in resistance to cardiac output during systole. The practical use of the NCP method was carried out in 1965 in a multicenter study in the treatment of cardiogenic shock in 8 patients with myocardial infarction [1]. Using this method, it was possible to achieve an increase in survival rate of up to 45%, which was significantly higher than the usual survival rate for cardiogenic shock (10-20%).
The use of NCP for the treatment of patients with angina pectoris was proposed by Banas in 1973 [2]. All patients showed a decrease in the functional class of angina pectoris and a decrease in the need for drug therapy. Further studies confirmed the effectiveness of NCP in the treatment of patients with coronary artery disease [3,4].
The advent of high technologies has made it possible to modify the device so as to perform sequential compression of the arteries of the lower extremities in such short periods of time as diastole; after which the procedure became known as enhanced NCP. The use of the “sequential” compression mode provides a greater increase in diastolic pressure in the aorta and a clear reduction in the energy expenditure of the myocardium during systole [5].
The largest study of the capabilities of NCP in patients with coronary heart disease can be considered the multicenter, double-blind, placebo-controlled, randomized study MUST-EECP (Multicenter study of enhanced external counterpulsation), completed in 1999, conducted at seven university medical centers [6]. Its goal was to determine the effectiveness and safety of using NCP in this category of patients. In 139 patients with angina, an increase in exercise tolerance, time to onset of ST depression during a treadmill test, a decrease in the number of angina episodes, and a decrease in the dose of nitrates taken was shown. When performing NCP, a positive effect can be achieved in 80-81% of patients. The mechanisms by which such an improvement occurs remain not entirely clear. NCP may reduce disease symptoms by improving endothelial function, enhancing left ventricular function, and peripheral effects similar to those observed with chronic exercise. Recent scientific work indicates that a regular artificial increase in diastolic pressure leads to the release of various growth factors and stimulates angiogenesis in the coronary bed [7-11].
The theoretical prerequisites for the use of NCP suggest that to achieve the desired effect, at least one of the coronary arteries should not be significantly stenotic [4]. The development of collaterals due to increased diastolic pressure during NCP will not be as effective if this pressure does not increase in the distal part of the coronary arteries due to their stenosis. A number of studies have shown that the most complete effect of treatment using the NCP method is achieved in patients with one- and two-vessel lesions. Based on this, it can be expected that the method of external counterpulsation can be used to treat patients who have undergone coronary artery bypass grafting (CABG) for three-vessel disease[12,13].
The small number of publications on this topic makes it possible to conduct further research into the effectiveness of using NCP in this category of patients. Non-invasive effects on hemodynamics using mechanical devices for the treatment of chronic ischemic heart disease have not been used in clinical practice in our country. To date, there have been no reports in the domestic literature on the use of the external counterpulsation method for coronary heart disease.
Material and methods
The study included fifteen patients with hemodynamically significant lesions of the coronary arteries documented by coronary angiography. These are patients with severe clinical angina, refractory to conventional antianginal therapy, in whom coronary artery bypass grafting is technically not possible, or clinical angina resumes after surgical treatment of coronary artery disease, as well as in preparation for CABG. To determine indications and contraindications for the use of the method, patients underwent: ECG, transthoracic echocardiography, duplex scanning of brachiocephalic vessels and vessels of the lower extremities, treadmill test, myocardial scintigraphy, coronary angiography, determination of rheological properties of blood.
Table 1. Patient characteristics
| Men: Women | 13: 2 |
| Age | 54,3 ± 7,2 |
| Angina pectoris | |
| 1 FC | 2 |
| 2 FC | 6 |
| 3 FC | 7 |
| History of myocardial infarction | 10 |
| Revascularization to NCP | |
| CABG | 4 |
| TLBAP | 4 |
| Number of affected arteries | |
| 1 arteries | 5 |
| 2 arteries | 3 |
| 3 arteries | 7 |
In accordance with the MUST-EECP recommendations, patients with severe decompensated heart failure were excluded from the study; with aortic insufficiency; with uncorrected arterial hypertension above 180/100 mm. rt. Art., patients with an implanted pacemaker; with arrhythmias that may affect the synchronization of counterpulsation with the ECG (atrial fibrillation, frequent extrasystole); with occlusive diseases of the peripheral vessels of the lower extremities; with hemorrhagic diathesis or significant coagulopathies, taking indirect anticoagulants (prothrombin time more than 15 seconds, INR more than 2.0); with a history of phlebitis and/or thrombophlebitis; patients who underwent interventional interventions within 2 weeks before the study.
Angina severity was assessed according to the Canadian Society of Cardiology classification. The patients (13 men and 2 women) suffered from chronic stable angina pectoris FC I–III. The characteristics of the patients are presented in Table No. 1. The average age of the patients was 54.3 years (40 – 64). Ten patients suffered myocardial infarction, four had TLBAP, and four had CABG. Two patients had heart failure (NYHA class I) with left ventricular systolic dysfunction and ejection fraction of 40% and 41%.
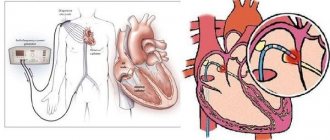
External counterpulsation procedures were performed on the TS3 model of the EECP Therapy System cardiac therapy complex (Vasomedical Inc., USA).
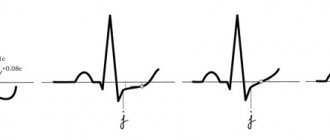
Cuffs are placed on the patient's legs, into which air with subatmospheric pressure is pumped at high speed during diastole. Synchronization with the ECG is carried out in such a way that the retrograde pulse wave reaches the aortic root to the complete closure of the aortic valve leaflets (Fig. No. 1). Each cuff is divided into three parts, covering respectively the calves, the lower third of the thigh and the upper third of the thigh with the capture of the buttocks, which are inflated sequentially from distal to proximal. This leads to retrograde arterial blood flow and an increase in diastolic pressure in the aorta, which in turn leads to an increase in coronary perfusion pressure and increased blood supply to the myocardium. There is also an increase in venous return to the right side of the heart. Instantaneous pumping of air from the cuffs into the ventricular presystole reduces vascular resistance and, therefore, reduces the work of the heart.
Figure.1 Operating principle of the NCP
NCP treatment was carried out for an hour, daily, with a course of 24 to 35 procedures. During each session, the acute hemodynamic effects of NCP, defined as the ratio of maximum diastolic to systolic pressure (NKP efficiency ratio), were measured using finger plethysmography. A cuff pressure of approximately 220 – 300 mm was applied. rt. Art., so that the D\S index (the ratio of the peak of the diastolic amplitude to the peak of the systolic amplitude) is from 1.1 to 2.0.
Analysis of the effectiveness of therapy was carried out on the basis of assessments of the condition by doctors and patients, as well as taking into account the influence of NCP on such indicators as the number of angina attacks per week, average consumption of short-acting nitrates per week, the patient’s quality of life, and the functional class of angina. Patients were asked to record the frequency and duration of angina attacks, as well as the number of doses of nitroglycerin taken before the start of treatment and after the course of NCP. Quality of life was assessed using a questionnaire based on the SF-36tm.
All patients performed an exercise test according to the Bruce protocol before and after treatment. Evaluation of the effectiveness of treatment was carried out according to the following criteria: increase in the duration of the load, time until the development of ST segment depression by 1 mm, double product at the peak of the load, tolerance to physical activity.
To assess left ventricular myocardial perfusion, patients underwent single-photon emission computed tomography with Tc-tetrofosmin (SPECT) before and after treatment according to a standard one-day protocol: exercise (bicycle ergometry) - rest.
Safety was assessed by observing side effects during the NCP procedure and throughout the course of treatment.
International EECP Patient Registry (EECP)
The purpose of the MRUP, established in 1998, was to document the safety, effectiveness, and use of EECP in a consecutive cohort of patients.9 The registry was open to all centers using EECP to treat patients with angina. Since it was voluntary, it occurred at no cost to patients and to the centers. The first phase involved more than 5,000 patients who were followed for at least three years. There are currently 92 centers participating in the registry, including 82 from the United States, 5 from Europe, and 5 from other locations around the world. The first 5222 enrolled patients who underwent 5718 EECP procedures were analyzed. The mean age of participants was 66 years (±11), with a male to female ratio of 74 to 26. Time since diagnosis was 9 years, and 78% had multivessel disease. Primary diagnoses and procedures were congestive heart failure (27%), myocardial infarction (64%), angioplasty/coronary artery bypass grafting (80%), and angioplasty (60%).
Fig. 4 Improvement in angina FC in patients participating in the EECP Consortium (n = 2,289).
Figure 5 shows 24-month changes in angina FC in a cohort of 567 registry patients. Only 2% of patients experienced worsening angina. Among all patients, 30% experienced cumulative side effects. Of these, the two most common were hospitalization for cardiac disease and repeat EECP. After more than two years, 7% of patients died. Most of these patients were excluded from revascularization before EECP. Quality of life, health status and satisfactory parameters were also measured. At the end of 24 months, there was a trend toward lower quality of life, although it was still significantly better than at baseline.
results
All patients (100%) showed a decrease in symptoms of coronary artery disease. Significant changes in the frequency, duration and severity of angina were noted. The functional class of angina was assessed twice during the study: before the start of therapy and after the course of treatment. As a result of the use of NCP, the average angina FC value decreased significantly (from 2.3 to 1.07). By the end of the course of treatment with NCP, six (40%) patients were transferred to FC I, five (33.3%) to FC II, and in four (26.7%) no angina attacks were observed at all (Fig. No. 2).
Figure 2. Distribution of patients by FC before and after treatment
The results of the study showed that during treatment with NCP, the number of angina attacks (from 15.7 to 5.2) and the doses of nitroglycerin taken (from 22.4 to 6.3 tablets) statistically significantly and systematically decreased from week to week.
All patients note an improvement in the quality of life, both in terms of the overall score and the results of physical and emotional parameters.
The study found a significant increase in exercise tolerance and the total duration of the stress test. The standard criterion for the anti-ischemic effect is the time until the onset of ST segment depression by 1 mm. We have identified a significant increase in this indicator.
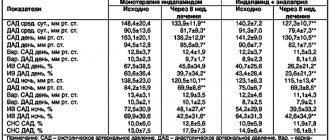
Table No. 2 shows the results of stress tests before and after treatment.
Table 2. Results of stress tests before and after treatment
| Before treatment | After treatment | |
| Total test duration, sec | 391 ± 163 | 642 ± 152 |
| Exercise tolerance, METs | 4,1 ± 1,1 | 7,1 ± 1,9 |
| Time to development of ST depression by 1 mm, sec | 324 ± 158 | 562 ± 185 |
| Double product at peak load, (SBP∗HR)/100 | 189 ± 36 | 213 ± 38 |
According to myocardial scintigraphy, after a course of treatment there is a decrease in the area and severity of myocardial damage in the form of a decrease in stress-induced ischemia and the size of the myocardial perfusion defect under load.
The procedures were well tolerated, all patients completed the course of treatment. There were no serious clinical complications associated with the use of NCP during the study. However, side effects associated with the effects of the device were observed: hyperemia, paresthesia and pain in the legs during the procedure.
Summary
Since the 1960s, many clinical trials of EECP have been conducted. Most of these studies have focused on the use of EECP in patients with angina. Only one of them was randomized. These clinical trials have shown the positive effects of EECP in reducing the incidence of angina, increasing the duration of physical activity and improving the quality of life of patients. The International EECP Patient Registry, taking into account stages I and II of patient inclusion, expands the database on the results of EECP treatment.
Discussion
Several studies have shown beneficial clinical effects associated with NCP: reduction in the number of angina attacks [5,14-17] and nitrate requirements [14-16], increased exercise tolerance [3,12,14,16,18,19] , beneficial psychological effects and improved quality of life [20,21], as well as an increase in the time of development of stress-induced ST-segment depression, accompanied by a decrease in myocardial perfusion defect [17,18].
The significant change in the symptoms of coronary artery disease is similar to the results of previous studies, and we noted that the greatest improvement after treatment was observed in the initially more severe condition of the patient (III angina).
In our study, there was a significant increase in exercise capacity, while the double product changed little, mainly due to a decrease in maximum BP. This fact confirms that NCP, as well as physical exercise, causes a decrease in peripheral vascular resistance. Peripheral effects may be particularly important for the symptomatic improvement observed in patients without evidence of increased myocardial perfusion after NCP [22]. Thus, in most patients, improvement in well-being was noted after 6–12 procedures.
The increase in exercise test time and exercise tolerance after NCP is similar to the data obtained in the MUST-EECP trial.
What is special about the counterpulsation device?
The device for the procedure is Lumenair. This is a unique device used to carry out this treatment method. The main features of the procedure are its non-invasiveness, atraumaticity and safety.
Equipment for EECP
This therapy does not require surgery, making incisions, or taking pills for a long time. A correctly performed course of procedures significantly improves the patient's condition. Clinical studies have given good results, which indicate high effectiveness.
There are several possible mechanisms for the positive effects of EECP:
- Increased current during diastole.
- Dynamic changes in neurohumoral regulation factors.
- Influence and changes in the functioning of the chambers of the heart - the ventricles.
In addition, the so-called “placebo effect” is possible. These mechanisms have not been confirmed. The likelihood of these hypotheses has not been confirmed. But it is already clear that the effectiveness of the method is high.
The operation of the device is controlled by a computer. Thanks to this, the possibility of errors during execution is completely eliminated.
conclusions
External counterpulsation is an effective non-invasive, outpatient procedure that causes a marked decrease in the frequency and duration of angina attacks, an increase in exercise tolerance, an improvement in the quality of life of patients with coronary artery disease, and when used after operations on the coronary arteries, it improves the results of surgical interventions.
Strict adherence to the MUST-EECP recommendations allows you to avoid unwanted complications and makes NCP safe for the patient.
Bibliography
1. Soroff HF. Birtwell W.C. Giron F et al. Support of systemic circulation and left ventricular assist by synchronous pulsation of extramural pressure. Surf; Forum. 1965:16:148-150. 2. Banas JS Brilla A. Levine HJ: Evaluation of external counterpulsation for the treatment of angina pectoris. Am J Cardiol 1973:31:118 3. Lawson WE, Hui JCK, Zheng ZS, et al. Improved exercise tolerance following enhanced external counterpulsation: Cardiac or peripheral effect. Cardiology 1996;87:271-275. 4. Lawson WE, Hui JCK, Zheng ZS, et al. Can angiographic findings predict which coronary patients will benefit from enhanced external counterpulsation? The American Journal of Cardiology 1996;77:1107-1109 5. Zheng ZS, Yu L, Kambic H, et al. New sequential external counterpulsation for the treatment of acute myocardial infarction. Transactions of the American Society of Artificial Internal Organs 1984;8(4):470-477 6. Arora RR, Chou TM, Jain D, et al. The Multicenter study of enhanced external counterpulsation (MUST-EECP): Effect of EECP on exercise-induced myocardial ischemia and anginal episodes. The Journal of the American College of Cardiology 1999;33(7):1833-1840. Feldman AM. Enhanced External Counterpulsation: Mechanism of Action. Clinical Cardiology. 2002 Dec;25(12 Suppl 2):II11-15. 7. Masuda D, Fujita M, Nohara R, Matsumori A, Sasayama Sh. Improvement of oxygen metabolism in ischemic myocardium as a result of enhanced external counterpulsation with heparin pretreatment for patients with stable angina. Heart Vessels (2004) 19:59–62 8. Bagger PJ, Roger JC, Koutroulis G, Nihoyannopoulos P. Effect of Enhanced External Counterpulsation on Dobutamine-Induced Left Ventricular Wall Motion Abnormalities in Severe Chronic Angina Pectoris. Am J Cardiol 2004;93:465–467 9. Masuda D, Nohara R, Kataoka K et al. Enhanced external counterpulsation promotoes angiogenesis factors in patients with chronic stable angina. Circulation 2001; 104; II445. 10. Soran O, Fleishman B, Demarco T, et al Enhanced external counterpulsation in patients with heart failure: a multicenter feasibility study. Congest Heart Fail. 2002 Jul-Aug;8(4):204-8, 227 11. Wu GF, Qiang SZ, Zheng ZS, et al. A neurohormonal mechanism for the effectiveness of enhanced external counterpulsation. Circulation 1999;100(18):I-832. 12. Lawson W, Hui J, Guo T, et al Prior revascularization increases the effectiveness of enhanced external counterpulsation. Clinical Cardiology 1998;21:841-844. 13. Lawson WE, Hui JCK, Oster ZH, et al. Enhanced external counterpulsation as an adjunct to revascularization in unstable angina. Clinical Cardiology 1997;20:178-180. 14. Lawson WE, Hui JCK, Soroff HS, et al. Efficacy of enhanced external counterpulsation in the treatment of angina pectoris. The American Journal of Cardiology 1992;70:859-862. 15. Lawson WE, Hui JCK, Zheng ZS, et al. Can clinical findings predict which patients will benefit most from enhanced external counterpulsation? Journal of Investigative Medicine 1995;43(5):392A. 16. Lawson WE, Hui JC, Cohn PF. Long-term prognosis of patients with angina treated with enhanced external counterpulsation: five-year follow-up study. Clinical Cardiology. 2000;23(4):254-258. 17. Stys TP, Lawson WE, Hui JC, Fleishman B, Manzo K, Strobeck JE, Tartaglia J, Ramasamy S, Suwita R, Zheng ZS, Liang H, Werner D. Effects of enhanced external counterpulsation on stress radionuclear coronary perfusion and exercise capacity in chronic stable angina pectoris. Am J Cardiol. 2002 Apr 1;89(7):822-4. 18. Masuda D, Nohara R, Hirai T, Kataoka K, Chen LG, Hosokawa R, Inubushi M, Tadamura E, Fujita M, Sasayama S. Enhanced external counterpulsation improved myocardial perfusion and coronary flow reserve in patients with chronic stable angina; evaluation by(13)N-ammonia positron emission tomography.Eur Heart J. 2001 Aug;22(16):1451-8 19. Urano H, Ikeda H, Ueno T, et al Enhanced external counterpulsation improves exercise tolerance, reduces exercise tolerance induced myocardial ischemia and improves left ventricular diastolic filling in patients with coronary artery disease. Journal of the American College of Cardiology. 2001;37(1):93-99 20. Fricchione GL, Jaghab K, Lawson WE, et al. Psychosocial effects of enhanced external counterpulsation in the angina patient. Psychosomatics 1995;77:494-497. 21. Springer S, Fife A, Lawson W, et Psychosocial Effects of Enhanced External Counterpulsation in the Angina Patient: A Second Study. Psychosomatics 42:124-132, April 2001 22. Bonetti PO, Holmes DR Jr, Lerman A, Barsness GW. Enhanced external counterpulsation for ischemic heart disease: what's behind the curtain? J Am Coll Cardiol. 2003 Jun 4;41(11):1918-25