Destruction of venous valves after thrombosis is the main cause of the development of circulatory failure and trophic ulcers in postthrombotic disease. Valvuloplasty (valve repair surgery) for incompetent deep vein valves is an effective method of improving venous outflow. Restoration of the valvular apparatus of the deep veins is possible in various ways, each of them has its own indications. This may involve replacing the affected venous segment with another section of the vein with preserved valves, or switching venous outflow through branches with preserved valves.
The best results are achieved through direct restoration of the valve apparatus using microsurgical valvuloplasty. Valvuloplasty allows for good compensation of venous outflow, which leads to a reduction in edema and healing of trophic ulcers. Deep vein valvuloplasty should be performed by experienced vascular surgeons who are proficient in microsurgical techniques and understand the pathology of venous outflow.
What is chronic venous insufficiency?
Under this term, doctors combine a number of diseases that lead to long-term, sometimes lifelong, disruption of the venous outflow from the legs. The most common causes of chronic venous insufficiency are varicose veins and previous deep vein thrombosis (postthrombotic and/or postthrombophlebetic disease). Congenital disorders of the venous system are less common. I note that disturbances in venous flow are not always associated with disease. They can occur during pregnancy, obesity, long journeys, flights, prolonged standing and a sedentary lifestyle.
Creation of a new venous valve
The principle is to construct a new valve using the patient's venous tissue. The technique for creating the valve depends on the situation with the venous wall. If it is thickened, then it can be stratified, then the resulting flap is fixed in the form of a sail directed with the convex side in the distal direction. You can make a bicuspid valve, which is the most physiological and effective. If there are fibrous cords in the lumen of the vein after thrombosis, then they can be used as leaflets of the valve being created. In the absence of such conditions, you can create a valve using your own venous wall, immersed in the lumen.
How does the venous system work?
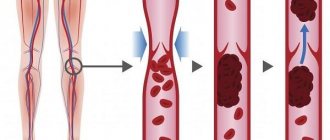
The outflow of blood from the legs occurs through deep veins, located deep in the muscles, and subcutaneous veins, passing through the subcutaneous fatty tissue. The deep and superficial venous systems of the lower extremities are connected to each other by the so-called perforating veins. The fundamental feature of the structure of the leg veins is the valves, which orient the blood flow strictly towards the heart. In addition, valves in the connecting veins allow blood to flow from the saphenous veins to the deep veins and prevent its return. Venous valves are distributed unevenly: the largest number is located on the lower leg (up to 20-30) and the smallest (2-3) on the thigh.
Transplantation (transplantation) of a normal venous segment
In order to restore the valve apparatus in veins that are not suitable for direct valvuloplasty, replacement of the venous segment with a section of the axillary or brachial vein with valves can be used. Using an incision in the shoulder, a section of a healthy vein with valves is removed and sutured into the femoral vein. Thus, a full-fledged valve apparatus is restored.
The disadvantage of this technology is the possibility of developing secondary expansion or, conversely, scarring of the transplanted segment, since the veins are somewhat different in structure.
Why do venous valves malfunction?
The main reason is disruption of the normal functioning of the vein valves. The blood flow becomes chaotic, and in the veins, especially the subcutaneous ones, the pressure increases so much that the walls of the vessel cannot stand it and begin to expand. In addition, other symptoms of the disease appear. The force of gravity is of greatest importance.
They say that vein diseases are a kind of payment a person pays for the ability to walk upright. That is, people who spend a lot of time on their feet have the greatest risk of disease - for example, doctors, salespeople, hairdressers. Since the amount of pressure in the veins is directly proportional to height, it is believed that tall people are more prone to chronic venous insufficiency.
Another important reason leading to disruption of the venous valves is an increase in intra-abdominal pressure. This occurs during heavy lifting and pregnancy. Venous thrombosis, which almost completely destroys the valves in the affected vein, has a disastrous effect on the valves. In addition, venous valves can be destroyed as a result of frequent household or sports injuries.
The operation does not require anesthesia, does not lead to disability, is performed without incisions and under local anesthesia
Photo: clinic “No Varicose Veins”
Anatomy of the veins of the lower extremities
Rice.
1 Proper operation of venous valves There are two types of blood vessels in our body - arteries and veins. With the help of arteries, oxygen-rich blood from the lungs and heart flows to all organs and tissues, including the legs. The function of the veins is to drain oxygen-poor blood back to the heart and lungs. In order for the blood from the legs to run upward against gravity, there are special venous valves that allow it to flow in only one direction. While walking, the muscles of the lower leg contract, they compress the deep veins, and blood is thrown upward. This mechanism is called the venous-muscular pump. This is why patients with varicose veins are advised to lie or walk more and stand or sit less.
What are the veins in the body and how do varicose veins appear?
In the legs there is a deep venous system and a system of saphenous veins (superficial) veins, as well as perforating veins connecting them. With varicose veins, the vein stretches and the valve flaps no longer reach each other, and blood begins to flow between them in the opposite direction. This is varicose veins. In the vast majority of cases, varicose veins are not deep, but superficial veins, surrounded on the outside by soft subcutaneous fat.
In the superficial venous network, the large and small saphenous veins are distinguished (Fig. 2). The first arises from the inner malleolus and continues to the inguinal fold, where it flows into the deep vein system. The second begins at the outer ankle and runs along the back of the lower leg. It drains into the deep vein system in the area below the knee. Varicose veins cause the tributaries of the main saphenous veins to become visible (Fig. 3). Our phlebologists also often encounter spider veins in patients (Fig. 4).
Rice. 2 Schematic anatomy of the saphenous veins of the lower extremities
It must be said that in most patients with varicose veins of the lower extremities we see not the main saphenous veins, but their tributaries
, that is, those veins that flow into them (Figure 3).
There is also an enlargement of the smallest, intradermal veins, which are also called “spider veins” (Figure 4). This is a separate disease, which we talk about in the corresponding section of the site.
Rice. 3 Dilated tributaries of the great saphenous vein (the largest saphenous vein (trunk) itself is not visible, only its tributaries - branches are visible)
Rice. 4 Spider veins (dilated intradermal veins)
All treatment methods for varicose veins are aimed at eliminating dilated saphenous veins. The most common question from patients is: “Then how will the blood flow back?” But, as we said earlier, through varicose veins the blood not only no longer flows upward towards the heart, but on the contrary - the oxygen-poor blood between the valves flows downwards. That is, patients no longer just live without these veins, but also in conditions where these veins are harmful.
Thus, an increased load falls on healthy veins, and when we remove varicose veins, it only becomes easier for healthy ones. In addition, you always have a deep venous system, which, as mentioned above, is almost never subject to varicose veins, since it is surrounded on the outside by dense muscles, bones and ligaments, and not by soft fatty tissue. Today, the most modern method of treating the main saphenous veins is endovenous laser coagulation, and their tributaries – miniphlebectomy and sclerotherapy.
Why does the risk of developing chronic venous insufficiency increase during pregnancy?
There are several reasons for this. Mechanical factor: from the second half of pregnancy, the growing uterus increasingly compresses the inferior vena cava and iliac veins. Compression of the retroperitoneal veins reaches a maximum towards the end of pregnancy.
Blood circulation : as pregnancy progresses, circulating blood volume (CBV) increases by 15-25%. This well-known fact is associated with the need to ensure placental blood circulation. An increase in blood volume, in turn, causes additional stress on the heart and vascular bed.
Hormonal factors : Increased levels of sex hormones during pregnancy cause a number of changes affecting the venous system. Dilatation (expansion) of venules (small veins) develops, their inner and middle layers thicken. In the intima (inner part of the veins), immune complexes begin to accumulate, causing aseptic inflammation like phlebitis. The result is progressive phlebostasis. In addition to the direct effect on the venous wall, estrogens and progesterone cause a cascade of changes in the hemostatic system.
Dysproteinemia : during pregnancy, the level of blood albumin (protein) decreases, which disrupts the colloid-osmotic balance.
Hemostasis and hemorrheology : changes in the hemostatic system occur already in the first trimester of pregnancy. By the third trimester, the fibrinolytic activity of the blood (an indicator reflecting the ability of the blood to dissolve formed blood clots) decreases significantly and its viscosity increases. Depression of anticoagulation mechanisms reaches its maximum.
How does venous insufficiency manifest?
The first signs of trouble with the venous system are swelling of the lower leg and foot at the end of the day, a feeling of heaviness and fullness in the calves. Patients pay attention to the fact that shoes that are comfortable in the morning begin to feel tight in the evening; socks or knee socks leave deep marks on the skin. Typically, these symptoms decrease with walking and after a night's rest.
Later, bursting pain in the calves, a feeling of heat in the legs and night cramps in the calf muscles appear. External changes are also taking place. Small blue-red spider veins, dark blue intradermal veins and intricately convoluted varicose veins form on the thighs and legs.
Varicose veins in the form of dark blue conglomerates, resembling bunches of grapes, quickly appear on the thighs and legs. As the disease progresses, the skin of the lower leg becomes dry and sensitive to various injuries. Then small dark brown islands appear, gradually merging into a single archipelago. In its center, a skin area resembling a stearin deposit is formed, and after this a trophic ulcer opens.
Or maybe there is no need to treat CVI at all?
In principle, the question is reasonable. After all, dozens and even hundreds of people walk around all their lives with “veins in their legs” and supposedly nothing happens to them. That's what they say. In fact, they experience very painful sensations and constantly expose themselves to the risk of complications. Ulcers are not the most unpleasant thing. In a number of studies conducted mainly in Europe on fair-skinned people, the incidence of venous thromboembolism, standardized by age and sex, ranged from 30 to 117 cases per 100 thousand people. What is this and how to understand it?
Venous thromboembolism is when a blood clot first forms in the veins, then breaks off and travels to the heart. After this the heart stops. Now just count how many people live in Krasnoyarsk, divide the number by 100 thousand and you will understand for yourself whether there is a risk. Better yet, “try on” an ulcer for yourself. Do you need it? Moreover, modern technologies make it possible to get rid of these troubles quickly, practically painlessly and effectively. One of the most effective is the EVLC (endovasal laser coagulation) method.
What is special about EVLC?
Before the advent of EVLT, it was not possible to get rid of swollen veins in the legs so quickly, easily and effectively by any of the previously known methods. The main advantage of EVLT is an excellent cosmetic result with minimal trauma. Unlike open surgery, the procedure takes from 20 to 40 minutes, does not require anesthesia, is performed without incisions, under local anesthesia, and it is possible to treat both legs at the same time. In this case, the patient experiences minimal pain and does without bruises or hematomas. There is no need for hospitalization, there is no loss of ability to work. There are minimal postoperative complications.
Getting rid of veins that have lost their function is also possible with the help of miniphlebectomy, a gentle removal procedure through a small incision or puncture.
The laser beam “seals” the vein from the inside; in a maximum of six months it will disappear
Photo: Maria Lenz
To treat varicose veins in the initial stages of the disease and on vessels of not very large diameter, the clinic uses the sclerotherapy method, which is very effective and inexpensive. The procedure is not surgical in nature; it consists of introducing special medications directly into the affected vessel using a syringe with a very thin needle. Spider veins, spider veins, and small veins that are visible through the skin are removed.
Possible complications after valvuloplasty
As after any major surgical operation, after valvuloplasty there are complications associated with the intervention itself:
- Bleeding
- Damage to the lymphatic ducts (lymphorrhea)
- Damage to cutaneous and deep nerves
- Postoperative wound suppuration
In our clinic, such complications are extremely rare.
Specific complications of this intervention are:
- Thrombosis of the reconstructed segment
- Ascending venous thrombosis
- Pulmonary thromboembolism
Fortunately, these complications are rare, their frequency does not exceed 1% of all operations performed.
If a relapse occurs, who is to blame and what to do?
If all therapeutic and preventive measures are followed, relapse is rare. The fact is that the weakness of the venous wall is a property of the body, the same as eye color, nose shape, hair color, fingerprints. This is how you are made. During the course of treatment it is impossible to remove all the veins, and it is not necessary. The disease can occur again in those veins that remain. In addition, such patients often have anatomical features of the structure of the venous system.
But we must always remember that the disease cannot defeat us only as long as we resist it. As soon as we stop resisting, the disease comes with renewed vigor. Therefore, preventive measures and doctor’s recommendations must be followed, even when everything seems to be fine.
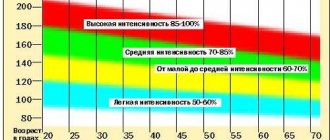
Is it possible for people with CVI to play sports?
There is an opinion among patients that venous insufficiency and sports are incompatible. This is wrong. On the contrary, to improve the health of the venous system, active sports such as running, cycling, race walking and especially swimming are useful and necessary. Only those types of exercises that lead to leg injury should be excluded. However, playing sports too hard and for a long time can also be harmful. Moderation is important in everything. If you run, it’s not long, walking isn’t far. Various types of physical education, gymnastics, and aerobics are ideal.
Is it possible to drive a car or fly on an airplane?
Staying immobile for a long time (driving, in a bus or airplane seat) disrupts the flow of blood through the veins, which can lead to an increase in venous insufficiency. Therefore, during long trips it is necessary to “insure yourself.” First of all, bandage your shins with an elastic bandage or put on special medical socks, stockings or tights. 10-15 days before the trip, start taking medications that improve venous outflow, for example, Detralex, Antistax, Ginkor, Anavenol.
Clinic “No Varicose Veins”:
Address : Krasnoyarsk, st. May 9, 51 Phone Website : varicose-net.rf
When traveling by car, you should stop every 1.5-2 hours and walk briskly for 10-15 minutes. During long flights or bus rides, it is advisable to stand up and walk around the cabin for a few minutes. In addition, periodic vigorous flexion and extension of the legs at the ankle joint are useful. So there are no special contraindications to traveling by car or plane.
Prognosis after valvuloplasty
The main goal of the intervention is to improve venous hemodynamics in the limb, which should ultimately lead to healing of trophic ulcers, reduction of edema and tissue hardening.
The result of treatment depends primarily on the correct determination of indications for surgery. Such a complex intervention as valvuloplasty should be performed only after all less complex methods of correcting venous outflow have been exhausted - eliminating reflux through the saphenous veins and perforators, the ineffectiveness of compression hosiery and venotonic drugs.