The most popular drugs for high blood pressure
April 5, 2021
10075
4.9
4
Content
- Captopril
- Amlodipine
- Losartan
- Prestarium
- Veroshpiron
- Concor
- Enalapril
Blood pressure can tell a lot about the state of the cardiovascular system, the functioning of the endocrine organs, the hematopoietic system and the nervous system. There is simply no universal remedy for blood pressure, because blood pressure can be constantly high, or it can rise sporadically. High blood pressure can be an independent pathology, or it can be one of the symptoms among a whole list of problems.
Therefore, you cannot just come to the pharmacy and ask for “something for blood pressure” - such drugs are prescribed exclusively by a doctor, knowing the full picture of the disease.
Which blood pressure medications do not cause coughing?
Since a dry cough appears after taking ACE inhibitors and beta-blockers, tablets from these groups must be prescribed with caution in case of arterial hypertension.
It is better to choose a medicine for blood pressure that does not cause coughing and has a milder effect.
For example, calcium antagonists do not usually cause the side effect of coughing. Combination medications and diuretics are also well tolerated.
Calcium antagonists
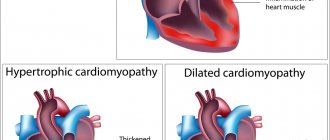
The most pronounced hypotensive effect is exerted by tablets belonging to the group of calcium channel blockers. At the same time, they are characterized as tablets for hypertension that do not cause coughing. The drugs act exclusively on myocardial and vascular cells.
- ACE inhibitors - list of drugs. Mechanism of action of new generation ACE inhibitors and contraindications
Calcium antagonists:
- normalize excitability processes;
- improve impulse conductivity;
- reduce blood pressure to normal levels;
- stabilize the tonometer readings for a long time;
- normalize carbohydrate metabolism;
- increase the contractile activity of the heart muscle;
- increase myocardial oxygen consumption. And this minimizes the likelihood of developing coronary heart disease;
- prevent the development of depressed and depressed mood;
- reduce the risk of left ventricular hypertrophy;
- have a beneficial effect on the functioning of the kidneys.
Calcium antagonists do not harm physical and mental activity, do not provoke the development of bronchospasm, and do not impair carbohydrate metabolism and kidney function. The most well-known drugs in this group are Nicardipine, Nimodipine, Isradipine, Lacidipine and Riodicin.
Since the list of side effects of calcium channel blockers is minimal, drugs in this group are recommended for use in the treatment of elderly people and patients diagnosed with diabetes mellitus.
Patients who take calcium antagonists note a rapid improvement in their overall health.
Diuretics
For hypertensive patients who have an increased risk of developing a dry cough during drug therapy, doctors advise using medications from the group of diuretics. Such tablets remove all excess fluid and salt from the body.
This allows you to normalize and stabilize the tonometer readings. A gradual decrease in blood pressure while taking diuretic tablets is explained by a decrease in circulating blood volume.
Furosemide tablets
But which blood pressure medications don't cause coughing? The drug Furosemide does not cause a cough attack. Doctors also often prescribe Indapamide, Veroshpiron, Spironolactone, Triampur, Arifon and Hydrochlorothiazide.
- IS KNEE PAIN ONLY DUE TO CALCIUM LACK?
Tablets from the diuretic group are prescribed in short courses. In this case, parallel administration of Panangin is indicated, the main active component of which is potassium. After all, a number of diuretics tend to wash out this microelement from the body.
To achieve maximum results and neutralize the influence of negative consequences, many doctors combine diuretics with calcium blockers or ACE inhibitors. There are also potassium-sparing diuretics. According to patient reviews, these are the best blood pressure medications that do not cause coughing.
Combination medications
Many cardiologists today prefer to prescribe their patients combination blood pressure medications that do not cause coughing. They are more effective, suitable for a wide range of people with high blood pressure and much easier to tolerate.
The main components of such tablets can be components from different medicinal groups, where the negative effects of some are suppressed by the positive effects of other medications.
The most popular combinations are given below:
- calcium antagonists + ACE inhibitors;
- diuretics + beta-blockers;
- diuretics + ACE inhibitors;
- calcium channel blockers + diuretics.
Many pharmaceutical organizations offer their consumers cough-free blood pressure tablets that contain not two, but three active ingredients.
All combination medications are available in different dosages of one and the other active substance.
The most popular and effective are the following combination drugs:
- Co-Renitec;
- Phosicard N;
- Equator;
- Logimax;
- Tarka;
- Atacand Plus;
- Noliprel forte.;
- Micardis Plus;
- Coaprovel.
New generation tablets have a number of advantages:
- The role of calcium in the treatment of arthrosis, is it needed?
- prolonged action;
- minimal risk of side effects;
- maximum therapeutic effect.
Self-prescribing antihypertensive drugs that do not cause a cough can worsen your health. The decision on the advisability of using a medicine should be made by an experienced doctor, based on the severity of the disease and the characteristics of the patient’s body. Sometimes the cardiologist selects an individual combination of drugs. This allows you not to provoke a deterioration in the overall clinical picture.
Captopril
This is one of the best drugs when you need to quickly lower your blood pressure. "Captopril" is not prescribed for use on an ongoing basis or in a course. This drug is often prescribed if a person has heart problems. Captopril has different dosages, but the most popular is 25 mg. For optimal results, take one tablet and place the second one under the tongue.
Captopril
OZON, Russia
Arterial hypertension (including renovascular), chronic heart failure (as part of combination therapy), left ventricular dysfunction after myocardial infarction in patients in a clinically stable condition.
Diabetic nephropathy in type 1 diabetes mellitus (with albuminuria more than 30 mg/day). from 8
700
- Like
- Write a review
Dry cough when taking blood pressure pills
Any drug that lowers a person's blood pressure has side effects. ACE inhibitors often provoke a cough without sputum discharge.
Many scientists have come to the conclusion that the occurrence of a dry cough when taking antihypertensive drugs occurs as a result of the accumulation of bradykinin in the bronchi.
Beta blocker medications can also trigger a cough. These drugs affect receptors located in the blood vessels, heart and bronchi.
| Medications | Side effects |
| Captopril | During drug therapy, a dry cough may occur. After stopping the medication, it goes away on its own. |
| Enalapril | A dry cough, difficulty breathing, bronchospasm, and pharyngitis may occur. |
Amlodipine
This long-acting blood pressure medication is available by prescription and is very popular. Amlodipine helps cells become saturated with oxygen, therefore preventing heart attacks. The medicine is also prescribed for angina pectoris.
Amlodipine
OZON, Russia
Arterial hypertension (monotherapy or in combination with other antihypertensive drugs).
Angina pectoris, vasospastic angina (Prinzmetal angina) from 15
782
- Like
- Write a review
Read also: Top 10 best blood thinners Blood thinners
Journal "Arterial Hypertension" 2(16) 2011
Angiotensin-converting enzyme (ACE) inhibitors are widely prescribed drugs, with more than 30 million patients receiving them worldwide today. ACE inhibitors reduce morbidity and mortality in patients with heart failure [1] and are well tolerated by most patients. However, when using these drugs, a side effect such as a dry cough often develops, which in severe cases leads to cessation of therapy. The latest edition of the Physicians' Desk Reference (PDR) reports that the incidence of cough with enalapril is 1.3% [2].
The purpose of this study was to evaluate the incidence of cough and the frequency of treatment discontinuation due to cough according to the literature and compare the obtained figures with those given in the PDR and drug instructions.
Patients and research methods
Research search and selection strategy
From 1990 to February 2010, we searched the PUBMED/EMBASE/CENTRAL databases using the keywords “angiotensin-converting enzyme inhibitors” and the names of individual ACE inhibitors (enalapril, lisinopril, perindopril, moexipril, ramipril, trandolapril, and fosinopril). We limited our search to studies performed on humans. We reviewed reference lists of review articles, meta-analyses, and original studies identified through electronic searches to identify other studies potentially eligible for analysis. There were no language restrictions in the search. When study results were unclear or significant data were not reported, we contacted the authors of the articles.
Studies eligible for inclusion in this analysis had to meet the following criteria: they must be randomized clinical trials (RCTs) in which one of the compared treatment regimens must be based on the use of ACE inhibitors; studies must have included at least 100 patients in the ACE inhibitor-treated group; the observation period had to last at least 3 months; Data on the frequency of cough development should be provided.
Assessing the quality of studies
Two authors (SB and SK) independently performed duplicate work assessing study eligibility and extracting data. Study quality was assessed using the Cochrane Collaboration's method for assessing risk of bias [4], which is based on 7 components. For each component, all studies were categorized as having low, high, or unclear risk of bias. Studies with a low risk of bias for 7 of the 7 components were considered low risk, 6 of the 7 components were considered to be at intermediate risk, and less than 6 of the 7 components were considered to be at high risk of bias.
Extracting data and merging it
Among the treatment outcomes, we were interested in the incidence of cough and the associated incidence of discontinuation of therapy in the group receiving ACE inhibitors, as well as in the other groups. The presence of cough was determined either by interviewing patients during routine visits or using a special questionnaire in which patients noted the frequency, severity and nature of cough.
Clinical significance - The frequency of a typical side effect when using angiotensin-converting enzyme inhibitors - cough - is significantly underestimated in drug reference books for doctors and instructions for the drugs. According to the literature, it is several times higher. — Measures should be taken to ensure that drug labels are regularly updated regarding both drug safety and specific side effects.
Physician's Drug Reference (PDR)
We searched the PDR from 1990 to 2009 and obtained information on the incidence of cough and associated discontinuation rates for each ACE inhibitor and for each indication (heart failure, hypertension). We also visited the Food & Drug Administration (FDA) website [5] and retrieved approval letters, final approved drug labels, number of label revisions, and frequency changes. cough when correcting instructions. Not surprisingly, the frequency of cough reported in the drug instructions was the same as in the PDR. If the PDR reported a range of frequencies, for example, “perindopril causes dry cough with an incidence of 6–12%,” then we took the higher of the two frequencies.
Statistical analysis
The meta-analysis was performed in accordance with the Cochrane Collaboration guidelines and the QUOROM/PRISMA algorithm [4, 6]. Stata 9.0 software (Stata Corporation, College Station, Texas) was used for calculations [7]. Cough rates reported across studies were pooled by weighting cough rates in each individual study using the inverse variance (1/(std dev)2). Cumulative meta-analytic frequencies were estimated for enalapril for each year separately. Heterogeneity was assessed visually using the Q test (chi-square) and/or I2 test. If studies were homogeneous, a model with fixed factor levels was used to estimate the pooled effect size. Otherwise, the random effects model of Der-Simonian and Laird [9] was used to calculate the overall difference.
We also assessed placebo-adjusted and other-drug-adjusted cough incidence associated with ACE inhibitor prescriptions. To do this, we found the difference between the frequency of cough when prescribing ACE inhibitors and placebo/other comparators. This was done only for groups from head-to-head comparison studies to minimize bias between the ACE inhibitor and comparison groups. We compared the data obtained with the placebo-adjusted frequency from the PDR/drug instructions (it was calculated in the same way). It should be noted that no other comparison groups, besides placebo, were given in the PDR/instructions for the drugs.
To calculate effect sizes in direct comparative studies, we used Peto's method [10, 11]. Presence of publication bias of positive study results was assessed visually using funnel plots or Begg's test and the weighted regression test of Egger et al. [12].
Sensitivity analyzes (for the incidence of cough and the incidence of treatment discontinuation due to cough) were performed by stratifying the analysis based on the following data: how patients reported the presence of cough (questionnaire or self-reported); what cohorts of patients were included in the study (with or without heart failure); the use of a combination therapy regimen compared with monotherapy; group size (for treatment with ACE inhibitors) ≥ 1000 patients or < 1000; duration of therapy ≥ 12 months or < 12 months; quality of studies (high risk of bias or low/intermediate risk of bias).
results
Study selection
Using electronic and manual searches, we identified 2811 RCTs, of which 125 studies (159 pairs of comparison groups) met the inclusion criteria and were selected for analysis (Fig. 1, Table 1). We excluded studies that administered a combination of ACE inhibitors and angiotensin receptor blockers (ARBs) (for example: ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET) - Study of the effect of telmisartan monotherapy and the combination of telmisartan and ramipril on the overall study endpoint) , and studies that included only those patients who were intolerant to ACE inhibitors. However, studies that administered a combination of ACE inhibitors and other drugs not commonly associated with cough (non-CABs) were included in the analysis.
Characteristics of studies
A total of 198,235 patients participated in 125 studies. Of these, 111,798 (56%) were randomized to receive ACE inhibitors and 86,437 (44%) to other treatments (including placebo). Of the 159 pairs of comparison groups, only 27 (17%) included patients with heart failure. In the majority of cases (132 pairs of compared groups; 83%), the patients did not have heart failure (mainly hypertension was present). Of the 125 studies, only 13 had a high risk of bias, while the remaining studies had a low or intermediate risk. None of the methods we used revealed the presence of bias associated with preferential publication of positive study results.
Cough incidence
Enalapril. Among 55 comparison pairs, 23,559 patients were randomized to enalapril treatment. In this population, the pooled weighted incidence of cough (according to a random effects model) was 11.48% (95% CI 9.54–13.41%), which was nine times higher than that reported in the PDR (incidence 1.3%; p < 0.0001; Fig. 2). It is worth noting that as data have accumulated over the past two decades, the frequency of cough has progressively increased and the confidence interval has narrowed (greater precision of the estimate).
Other angiotensin-converting enzyme inhibitors. Similar to the above, the frequency of cough according to the literature (random effects model) was significantly higher (except for ramipril and perindopril) compared to that reported by PDR (Fig. 3).
Discontinuation rate due to cough
Enalapril. The pooled weighted discontinuation rate due to cough with enalapril was 3.08% (95% CI 2.23–3.93%), which was 31 times higher than the rate reported in the PDR (discontinuation rate 0 .1%; p < 0.001; Fig. 4). It should be noted that while the frequency reported in the PDR remained unchanged, the cumulative frequency continually increased as literature data accumulated, and the confidence interval narrowed (a more accurate estimate), until eventually a plateau was reached by the beginning of the last decade.
Other angiotensin-converting enzyme inhibitors. Similar to the above data, the rate of discontinuation of therapy due to cough (random effects model) according to the literature data was significantly higher (except for benazepril and ramipril) than that given in the PDR (Fig. 5).
Direct comparative studies
Frequency of cough development. The pooled weighted incidence of cough (from lowest to highest) during treatment with calcium channel blockers was 2.72% (1.15–4.29%), diuretics - 3.25% (1.93–4.57%), ARB - 3.50% (2.35-4.65%), placebo - 5.33% (2.79-7.87%) and beta blockers - 5.86% (1.82-9.90%) ). It was significantly lower compared to the pooled rate for all ACE inhibitors (10.60% [9.14–12.07%; p < 0.001 for all comparisons]).
In direct comparative studies, the prescription of ACE inhibitors was associated with a significantly higher risk of cough compared with ARBs (Fig. 6), calcium channel blockers (odds ratio (OR) 4.35; 95% CI 3.89–4.87; I2 = 77.8%), placebo (OR 1.91; 95% CI 1.79–2.04; I2 = 47.5%), diuretics (OR 2.29; 95% CI 1.48–3. 54; I2 = 0.0%) and beta blockers (OR 1.81; 95% CI 1.56–2.12; I2 = 65.5%).
A comparison of placebo-adjusted cough rates reported in the literature and PDR/drug labels for ACE inhibitors is presented in Table 1. 2. The difference between the frequency of cough when prescribing ACE inhibitors and drugs of other classes is presented in table. 3.
Rate of discontinuation of therapy due to cough. Pooled weighted discontinuation rates due to cough (random effects model; rates in order from lowest to highest) for beta blockers were 0%, diuretics 0.35% (0.06–1.04%), placebo 0 .64% (0.40-0.88%), ARB - 0.35% (0.18-0.52%) and calcium channel blockers - 1.08% (0.09-2.06%). This was significantly lower than the pooled weighted discontinuation rate for all ACE inhibitors (2.54% [2.10–2.99%; p < 0.001 for all comparisons]).
In head-to-head comparative studies, ACE inhibitors were associated with a significantly higher risk of discontinuation due to cough compared with placebo (OR 3.37; 95% CI 3.06–3.72; I2 = 48.3%), ARBs (Fig. 6), calcium channel blockers (OR 5.65; 95% CI 3.87–8.25; I2 = 7.9%) or beta blockers (OR 6.29; 95% CI 2.69–14, 70; I2 = 0.0%). However, when compared with diuretics (1 study), there was no significant difference (OR 1.93; 95% CI 0.20–18.65).
Sensitivity Analysis
The incidence of cough was significantly higher in studies that used a cough questionnaire and among patients with evidence of heart failure compared with studies in which patients self-reported cough and patients without heart failure. However, the rate of discontinuation due to cough was similar (data not shown).
However, the rate of discontinuation of therapy due to cough was higher in studies with ACE inhibitor monotherapy, especially with large numbers of patients and long duration of therapy, compared with the corresponding comparison groups (data not shown).
There were no significant differences in the incidence of cough (10.59% [9.03–12.15%] vs. 10.81% [6.54–15.07%; p = 0.678]) and the rate of discontinuation due to cough (2.57% [2.09–3.05%] vs. 2.23% [0.96–3.50%; p = 0.401]) between studies at low/intermediate risk of bias and studies at high risk .
Discussion
The results of the present study, which included almost 200,000 patients, indicate that the incidence of a common side effect with ACE inhibitors, cough, is significantly underestimated in the PDR/labeling information. According to the literature, it is several times higher.
Cough incidence
The frequency of cough reported in the literature varies widely [13, 14]. This may be due to many factors: the size of the groups, the duration of treatment, the cohorts of patients included, the ways in which patients reported the presence of cough. The results of this study indicate that these factors influence the reported frequency. For example, there was a lower incidence of cough and a lower incidence of discontinuation due to cough in studies where ACE inhibitors were given in combination with non-ARB agents. Although there is currently no evidence to suggest that the incidence of these side effects is reduced in the presence of other agents, such a possibility cannot be excluded. Therefore, more research needs to be conducted to test this hypothesis. The incidence of cough was higher in the heart failure cohort. In a cohort of patients with heart failure, cough could be multifactorial in nature (pulmonary edema, exacerbation of heart failure), which may lead to misdiagnosis as cough due to the prescription of ACE inhibitors. The rate of treatment discontinuation due to cough did not differ between the two cohorts (with and without heart failure). This suggests that the higher incidence of cough reflects either difficulty in differentiating cough from heart failure itself or the presence of a higher threshold for discontinuation of ACE inhibitor therapy due to the well-known ability of these drugs to reduce morbidity and mortality in patients with this pathology. . Similarly, the frequency of cough was higher among patients who reported cough using a questionnaire. However, the rate of discontinuation due to cough was similar among patients who reported cough using a questionnaire or self-reported cough. This suggests that the rate of discontinuation due to cough is a more objective measure of side effects than the rate of cough [15]. Of note, the placebo-adjusted rate from the meta-analysis was greater than the corresponding placebo-adjusted rate from the PDR/label instructions. This suggests that regardless of how the data are presented (baseline rate or placebo-adjusted rate), the rates in the PDR/drug labels are lower than the corresponding rates in the literature.
US Food and Drug Administration Drug Instructions and Physician's Drug Reference (PDR)
The approval process for any new drug includes data from preclinical studies and at least two phase 3 RCT studies in patients with a specific disease. FDA reviewers evaluate these data from a clinical, epidemiological, statistical, toxicological, and pharmacological perspective, weigh the potential risks and benefits, and decide whether to approve the drug. The FDA helps communicate information to physicians through drug labeling. Section 201(n) of the Federal Food, Drug, and Cosmetic Act requires that drug labels be free of errors by either including unnecessary information or omitting relevant information. Instructions for drugs are published in PDRs and other electronic reference books and serve as a source of information for doctors and patients.
The results of the present analysis revealed differences between the literature data and the data provided to clinicians and patients. In table Table 4 shows the dates of the first approval for the use of each ACE inhibitor, the number of revisions of instructions, the incidence of cough and the frequency of discontinuation of therapy due to cough according to the instructions. Surprisingly, during the numerous revisions of the guidelines, no changes were made to the cough frequency or discontinuation rate. As a result, the risk of side effects is underestimated - sometimes in PDR it is 31 times lower compared to the data given in the literature. What does such an underestimation of actual indicators lead to? First, reporting a low incidence creates a false impression of safety among clinicians and patients. Secondly, this leads to a search for other causes of cough, which entails diagnostic errors and the prescription of unnecessary therapy. Vegter et al. [16] analyzed data from 27,446 patients taking ACE inhibitors and showed that the incidence of antitussive therapy for cough associated with ACE inhibitors was about 15%. Failure to recognize cough as a side effect of ACE inhibitors may lead to additional evaluations, diagnostic tests, and even empirical treatment with antibiotics and antitussives. Third, to uninformed clinicians and the untrained public, the frequencies reported in the PDR may provide the basis for broader recommendations for some drugs over others. For example, the PDR reports that the incidence of cough with enalapril is 1.3%, and with ramipril it is 12%. This leads to the false conclusion that enalapril is better tolerated than ramipril. The results of our analysis indicate that the incidence of cough is the same for all ACE inhibitors (enalapril 11.48%, ramipril 11.72%; p = 0.679). Data from a large number of studies clearly indicate that cough is a class-wide effect of this group of drugs. It should be noted that cough was not recognized as a class-specific side effect in studies of older ACE inhibitors until studies performed after the drugs were marketed showed that cough was quite common. This fact is one of the most likely reasons for the low frequency of cough for older ACE inhibitors compared to newer ones. However, it should be noted that the first approved instructions for enalapril (approved for use on December 24, 1985) reported that the incidence of cough with this drug was 1.3%. Since then, over the course of 23 years, the instructions have been revised 29 times. But even after the last revision of the instructions (September 25, 2008), the cough frequency given in the instructions remained at 1.3%.
In light of this state of affairs, it is necessary to oblige pharmaceutical companies to regularly submit new data on the effectiveness and safety of drugs to the FDA. It is probably impossible and even clinically impractical to update information on all nonspecific drug side effects. However, information about drug-specific side effects, such as cough and angioedema for ACE inhibitors, foot edema for calcium channel blockers, myalgia and myositis for statins, dyspnea for ticagrelor, should be collected systematically and reflected in the instructions for the drugs .
Limitations of the study
We were not able to include primary data from patients in different studies into the analysis. Therefore, we could not adjust for drug dose, concomitant therapy, smoking status, or any pulmonary or respiratory pathology that may contribute to the development of cough. Although we report the incidence of cough and discontinuation rates due to cough separately for each ACE inhibitor, any direct comparison is subject to bias due to heterogeneity in patient cohorts, group sizes, duration of therapy, and methods of reporting the presence of cough (whether patients complete a questionnaire). questionnaire or self-report the presence of cough). Therefore, the best way to evaluate this is to conduct a randomized comparison of individual ACE inhibitors.
conclusions
The results of this meta-analysis, which included almost 200,000 patients and is the largest to date, indicate that the incidence of cough with ACE inhibitors and the rate of discontinuation of therapy due to cough (a more objective indicator) in the literature are several times higher than similar ones. frequency given in the PDR (and drug instructions). In the real world, this frequency is apparently even higher than in the RCTs we analyzed. Accordingly, efforts should be made to ensure that drug labels are regularly updated regarding both drug safety and specific side effects.
Translation Ph.D. A.V. Savustyanenko Original article published in The American Journal of Medicine, 2010, 123, 1016-1030.
Losartan
This drug can be taken as a course or once for emergency blood pressure reduction. "Losartan" acts instantly, without having a negative effect on the cardiovascular system. A maximum of an hour after administration, the blood pressure returns to normal. The drug is also prescribed if a person suffers from heart failure.
Losartan
JSC VERTEX, Russia
Arterial hypertension.
Reducing the risk of associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, manifested by a combined reduction in the incidence of cardiovascular mortality, stroke and myocardial infarction. Protection of the kidneys in patients with type 2 diabetes mellitus with proteinuria - slowing the progression of renal failure, manifested by a decrease in the incidence of hypercreatininemia, the incidence of end-stage renal failure requiring hemodialysis or kidney transplantation, mortality rates, as well as a decrease in proteinuria. Chronic heart failure (as part of combination therapy, with intolerance or ineffectiveness of therapy with ACE inhibitors). from 30
1123
- Like
- Write a review
Is it necessary to stop taking a medicine that causes a cough?
The question of canceling treatment is decided on an individual basis. The appearance of a cough in the early stages of hypertension is an unfavorable symptom. It indicates developing vascular diseases and limits the range of medications that can be used to treat the underlying disease. If you continue therapy with the same drug, the side effects will become stronger.
If there are any signs of poor tolerability of the drug, it is better for the patient to seek help from a doctor. The best option is to replace the drug. However, this must be done correctly, after additional examination and identification of all the features of the course of hypertension. Independent selection of funds is fraught with a number of complications and aggravation of the patient’s condition.
Periodic pauses in therapy also lead to adverse consequences. Destabilization of pressure indicators and the development of a crisis are possible. In this case, the patient will have to go to the hospital. Severe changes are fraught with acute, life-threatening complications.
Prestarium
The advantage of this blood pressure drug is that it not only helps reduce blood pressure, but also treats hypertension, even complex forms. Prestarium is prescribed if there is a risk of heart attack; patients who have problems with cerebral circulation can take it. But the problem is that Prestarium tablets are not available in all pharmacies and they are not cheap. But there are analogues of this medicine that a doctor can select.
Prestarium
SERVIER (Servier), France
A drug used for arterial hypertension and heart failure.
Also for such indications as: Prevention of recurrent stroke in patients with cerebrovascular diseases. Prevention of cardiovascular complications in patients with documented stable coronary heart disease. from 193
956
- Like
- Write a review
What medications provoke the syndrome?
So, what medications are there for hypertension that cause cough? Today it is known for sure that it is provoked by medications that belong to the following groups:
| Types of medicines | Names of drugs as an example |
| Beta blockers | |
| Angiotensin receptor blockers | |
| ACE inhibitors |
As experts note, a strong cough reflex is most often stimulated by medications that belong to the enalapril class of ACE inhibitors.
Veroshpiron
This medicine helps the body remove excess fluid, eliminating swelling. Potassium in Veroshpiron improves the functioning of the heart and blood vessels, and many patients note that the drug relieves seizures.
Veroshpiron
Gedeon Richter, Hungary
The drug Veroshpiron is a potassium-sparing diuretic.
from 72
762
- Like
- Write a review
Read also How to treat migraine: the best drugs Top 5 best drugs against migraine
Concor
The active ingredients of these blood pressure pills reduce the amount of adrenaline in the blood, which has a good effect on the functioning of the heart. Concor reduces heart rate and is suitable for those who have had a heart attack. But Concor is not suitable for older people and those with severe hypertension.
Concor
Merkle GmbH, Germany
- arterial hypertension;
— IHD: stable angina; - chronic heart failure. from 132
5.0 1 review
1288
- Like
- Write a review