Atherosclerosis is a serious vascular pathology, fraught with life-threatening consequences, such as acute cerebrovascular accident (stroke), ischemic heart disease (coronary heart disease), myocardial infarction, etc.
With atherosclerosis, plaques made of cholesterol and other fats, as well as calcium, form in the walls of the arteries. These changes negatively affect the condition of the blood vessels, depriving them of elasticity, narrowing the lumen and impeding blood flow. As a result of narrowing of the artery, the blood supply to the tissues is disrupted; when the plaque ruptures, blood clots form, clogging the artery with subsequent necrosis of vital organs (ischemic stroke, myocardial infarction, intestinal infarction, kidney infarction, gangrene of the extremities).
In this article we will tell you how to check whether you have vascular atherosclerosis and what tests you need to take for this.
What makes atherosclerosis doubly dangerous is that it may not manifest itself for a long time. Therefore, it is difficult to overestimate the importance of timely diagnosis (laboratory and instrumental) and assessment of the risks of developing this pathology.
Who needs atherosclerosis risk screening?
Anyone can be screened for the risk of developing atherosclerosis, but there are categories of patients for whom this screening is especially recommended.
Groups at risk of developing atherosclerosis
Risk groups for the development of atherosclerosis are formed depending on the causes of its development. Some causes are modifiable (depending on the person), others are non-modifiable .
The first group includes patients:
- suffering from arterial hypertension;
- smokers;
- with obesity (waist circumference in men - 94 cm or more, in women - 80 cm or more), poor nutrition (mainly fatty foods);
- with impaired carbohydrate metabolism (increased fasting glucose, impaired glucose tolerance, type 2 diabetes mellitus);
- Chronic kidney disease with decreased glomerular filtration rate (less than 60 ml/min).
The second group includes:
- men over 40 years old; women over 55 years of age;
- women with early menopause (before menopause they are protected from atherosclerosis by female sex hormones);
- early cardiovascular diseases (myocardial infarction or unstable angina) in the family (in men under 55 years of age, in women under 60 years of age);
- hereditary diseases (familial hyperlipidemia 11A, 11B, 111 types).
Treatment of blood thickness
When blood thickening occurs, therapy should be aimed at combating the underlying disease and preventing thrombosis. To do this, doctors prescribe medications that thin the blood and strengthen blood vessels:
- Cardiomagnyl, Cardiopyrin, Aspirin-Cardio;
- Curantil, Heparin;
- Lyoton;
- Capilar, Dihydroquercetin;
- Alka-Mine.
Vitamins C and B contribute to better absorption of medications.
Along with traditional methods, treatment with folk remedies is also widespread. For example, decoctions with herbs (hawthorn, sweet clover, clover, willow bark, etc.), hirudotherapy.
How to prepare for analysis
Three days before the test, you should avoid fatty foods rich in cholesterol (meat products, especially fatty ones, sausages, sausages, dumplings, etc.)
Blood for analysis for atherosclerosis must be taken strictly on an empty stomach (i.e., at least 8-10 hours must have passed since the last meal).
What does atherosclerosis risk screening consist of?
The essence of this diagnosis is a comprehensive study of the patient’s blood to determine biochemical markers of the development of atherosclerosis.
Extremely important indicators in screening are lipidogram or lipid profile data:
- total cholesterol;
- high density lipoproteins (HDL);
- low density lipoproteins (LDL);
- triglycerides (TG).
Cholesterol - the concentration of this substance in the blood is considered one of the most informative indicators of the lipid profile. But cholesterol itself is not found in the body, but is part of lipoproteins - complex compounds of fats and protein.
of lipoproteins - HDL, LDL, VLDL (high, low and very low density lipoproteins).
The last two groups are atherogenic; the cholesterol content in such compounds can reach 45% or higher. These lipoproteins transport cholesterol from the liver to cells, where it is involved in the production of cell membranes.
LDL and VLDL cholesterol is a key risk factor for the development of atherosclerosis, since these compounds easily pass into the vessel wall and form an atherosclerotic plaque.
High-density lipoprotein (HDL) has much less cholesterol. And they are able to “take” cholesterol from the walls of blood vessels and other tissues and transport it to the liver for “utilization.” Therefore, HDL cholesterol is considered “healthy” or “good.”
Triglycerides are another form of fat. Their high concentration in the blood can also contribute to the development of atherosclerosis.
In some cases, an extended lipid profile is performed. In addition to the above parameters, it includes:
- lipoprotein(a);
- apolipoprotein A1;
- apolipoprotein B.
Lipoprotein (a), like triglycerides, is a transport form of fat. In composition, it is closest to LDL, and, accordingly, an increased content of this substance in the blood also indicates the risk of developing atherosclerosis.
Apolipoprotein A1 is a protein that is one of the main components of the source of “good” cholesterol - HDL. Normal values of this indicator create optimal conditions for reducing cholesterol in the walls of the arteries.
Apolipoprotein B is the main protein component of LDL and VLDL involved in cholesterol metabolism. This is a key marker in assessing the risk of atherosclerotic lesions of the coronary vessels.
Interpretation of lipid profile results. Normally, total blood cholesterol should be less than 5.0 mmol/l; HDL level be more than 1.2 mmol/l in women and more than 1.0 mmol/l in men; and LDL - less than 3.0 mmol/l in both sexes; The triglyceride content in a healthy person should not exceed 1.7 mmol/l.
Important! The interpretation of the screening results should be carried out by a doctor who will correlate the test results with the individual characteristics of the person (age, weight, gender, existing diseases, medications taken, etc.).
Having studied the diagnostic results, the cardiologist will draw up a conclusion about the individual risks of developing atherosclerosis for the patient, give recommendations for prevention or prescribe additional examination if alarming signs are detected.
Early detection of pathology will allow you to begin the necessary treatment and avoid unwanted health consequences!
Screening for the risk of developing atherosclerosis at MedicCity
- Biochemical blood tests;
- Apolipoprotein A-1;
- Apolipoprotein B;
- Lipoprotein (a) (Lipoprotein (a);
- Triglycerides;
- High-density lipoprotein cholesterol;
- Low-density lipoprotein cholesterol;
- Cholesterol total.
In the laboratory and diagnostic department of our multidisciplinary clinic, you can undergo atherosclerosis risk screening and any other examination at a convenient time, without queues and as quickly as possible. We guarantee the reliability of the results, anonymity, and speed of data processing!
THICK BLOOD IS A SOURCE OF INCREASED DANGER!
We talked about this with Denis Sokolov, a cardiologist at Meditsina JSC (academician Roitberg’s clinic), candidate of medical sciences, member of the Acute Cardiovascular Care Association (ASSA) .
Denis Vladimirovich, “thick blood” is a philistine concept. How does it sound in medical language? — In medical practice, this condition is called increased blood viscosity and depends on the ratio of the amount of formed elements and blood plasma. Human blood consists of formed elements (leukocytes, erythrocytes, platelets) and a liquid part (plasma). Normally, the proportion of formed elements is no less than 40 and no more than 45%. If this amount increases, we are talking about increased blood viscosity.
Does “thick blood” threaten human health or life? - Threatens. The fact is that increased blood viscosity negatively affects the condition of the heart, blood vessels and all internal organs, because in the presence of such a condition, there is a risk of blood clots.
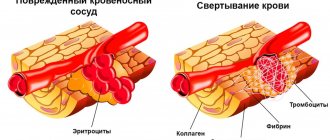
The main complication caused by increased blood viscosity is the formation of clots (thrombi) in the bloodstream. They block movement through the deep veins and vessels of the limbs, internal organs, and brain. As a result, increased blood viscosity can cause a number of diseases - ischemic stroke, myocardial infarction, pulmonary embolism, thrombosis of the veins and arteries of the lower extremities, and a number of internal organs. It is very dangerous. After all, acute disorders of coronary and cerebral circulation, pulmonary thromboembolism become causes of death if a predisposition to thrombosis is not detected in a timely manner and treatment is not started.
Are there any known causes that lead to increased blood viscosity? And who is at risk? — Such reasons are known, there are several of them. For example, dehydration often leads to increased blood viscosity. It occurs when a person does not drink enough water during intense physical activity and a hot climate. Diarrhea, vomiting, poisoning, and a number of somatic diseases also provoke dehydration and blood thickening.
Chronic diseases of the bronchopulmonary system, in which increased synthesis of blood cells occurs, is another risk factor for blood thickening.
Metabolic disorders in the form of macroglobulinemia (a malignant hematological disease), diabetes insipidus and diabetes mellitus, metabolic syndrome (manifested by impaired metabolism of fats and carbohydrates), obesity are also a trigger for increased blood viscosity. This group of causes also includes amyloidosis, in which a special, “abnormal” protein—amyloid—begins to be synthesized in the body. It is deposited in all tissues and organs, disrupting their functioning.
Increased blood viscosity is also diagnosed with increased spleen function and many oncological diseases.
People of what age, lifestyle and occupation are more likely to have “thick” blood? — The risk of high blood viscosity increases in older people. This is understandable: over the years, chronic diseases accumulate and metabolism slows down. Obese people are also at risk. People who work in hot weather conditions and in rooms with high air temperatures also have a high risk of blood thickening.
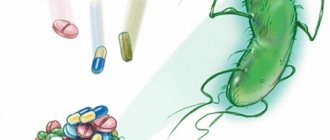
Can medications cause blood clotting? - Yes, this is possible. Blood thickening can occur due to uncontrolled use or overdose of diuretic drugs (furosemide, torsemide, spironolactone), because this leads to dehydration of the body.
Women have a specific risk factor - the use of oral contraceptives. The point here is that the estrogenic component present in such contraceptive drugs stimulates the activity of the blood coagulation system. In this regard, when taking contraceptives, blood clotting increases significantly.
There is evidence that drugs for the treatment of erectile dysfunction also provoke blood clotting.
What to do, stop taking much-needed medications? - Of course not. You just need to pass all tests and undergo examinations prescribed by your attending physician both before their appointment and during the appointment period. And strictly adhere to the rules for taking medications, avoiding their overdose.
Are there any manifestations of “thick” blood that should alert a person? — Signs of increased blood viscosity may include dizziness, noise in the head, headache with a feeling of heaviness, blurred vision, and numbness in the fingers. This may be accompanied by nausea, sleep disturbances, confusion, poor appetite, tingling shins and dry mouth.
Frequent infectious diseases should also be of concern. Indeed, due to blood thickening, blood circulation in the internal organs is disrupted, which, in turn, leads to a deterioration in the digestive function of the intestines and a deficiency of nutrients. The result is the body's instability to viral and bacterial pathogens.
Increased blood viscosity can be accompanied by dry skin, brittle nails, as well as thinning and hair loss. This again occurs due to insufficient blood supply to the tissues and impaired microcirculation.
Cold extremities are another manifestation. This is explained by the fact that with increased viscosity, blood circulation worsens. And this interferes with normal blood flow.
What specialty should you consult with in connection with the problem of “thick” blood? - To begin with, see a therapist, family doctor or general practitioner. The treatment of high blood viscosity itself must be comprehensive and carried out with the participation of a medical specialist. In particular, a cardiologist, and in some cases a hematologist.
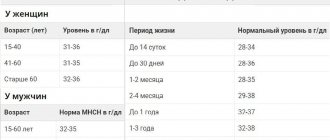
What tests need to be done to detect increased blood viscosity? — To diagnose increased or decreased blood viscosity, the patient must undergo a clinical blood test, which will reveal the number of red blood cells, hemoglobin, erythrocyte sedimentation rate and other indicators. Another mandatory test is hematocrit .
What kind of analysis is this? - Hematocrit readings accurately reflect the volume of blood contained in red blood cells (erythrocytes). In addition, the analysis reflects the cell size of red blood cells. Normal hematocrit values depend on the person’s gender and age. So, for an adult man it is 40-48%, for an adult woman - 36-46%, for a newborn child - up to 60%, for children under 13 years old - up to 38-40%. If the values are increased by at least 0.55%, then patients are diagnosed with high hematocrit .
What other tests need to be performed? — In some cases, the clinical laboratory uses the determination of the duration of bleeding and the determination of blood clotting. Clotting time describes how quickly blood clots form, the ability of platelets to stick to each other, and also gives information to the doctor about how long it will take for the body to seal the leak if the integrity of the vascular walls is compromised.
It is also necessary to perform a coagulogram . This study is a comprehensive laboratory assessment of hemostasis. And hemostasis is a complex of physiological processes that stop blood loss in the event of damage to the vascular wall, as well as maintain blood in a liquid state.
How is too viscous blood treated? — To reduce the number of formed elements and reduce blood viscosity, the patient requires special therapy, including treatment of the pathology that provoked this condition. In addition, the patient is prescribed a diet and specific medications. There is no specific treatment regimen. Treatment tactics always depend on the patient’s clinical picture. The general principles of combating high viscosity include correction of metabolic processes, prevention of blood clots, and treatment of neoplasms of hematopoietic tissue.
What medications are used to reduce blood viscosity? — Medications that reduce blood viscosity and reduce thrombus formation include antiplatelet agents and anticoagulants . Such as acetylsalicylic acid, clopidogrel, warfarin, abigatran, rivaroxaban, apixaban, heparin and many others. etc. These drugs are prescribed exclusively by the attending physician and are taken strictly according to indications on an individual basis. Self-prescription may lead to negative consequences. For example, aspirin-based medications are highly effective in normalizing blood consistency, but are prohibited for use in patients with abnormal gastrointestinal tract functions - gastritis, peptic ulcers. Since these drugs negatively affect the mucous membrane of internal organs.
Is excessive blood thinning, in turn, dangerous? — Of course, excessive blood thinning is dangerous, because... it can cause bleeding. And those, in turn, can become a serious threat to life.
Is it important to adhere to a certain type of diet to thin the blood?
- Necessarily. So, you need a special diet with sufficient fluid intake. It will reduce blood viscosity. In addition, the following products help reduce increased blood density:
- berries (blueberries, cherries, strawberries, white and red currants, gooseberries, cranberries);
- fruits - oranges, lemons, peaches, apples;
- vegetables - cucumbers, tomatoes, beets;
- spices - garlic, ginger, pepper, cinnamon;
- dark chocolate, cocoa, coffee.
Is it possible to use folk remedies to thin the blood? — With the doctor’s permission, you can try auxiliary treatment using folk remedies, taking into account the healing properties of some herbs and plants. For example, yellow sweet clover herb, hawthorn berries, valerian root, lemon balm, narrow-leaved fireweed, etc. have blood-thinning properties.
Flax oil has good thinning and antithrombotic properties. The product helps to establish metabolic processes, remove excess cholesterol, and prevent the development of atherosclerosis.
What is better - to prepare medicinal herbs yourself or buy them in a pharmacy chain? — Independent preparation of medicinal herbs requires special knowledge. Therefore, it is easier and better to buy herbal remedies at the pharmacy. It’s not for nothing that they are called medicinal. And all medicines are sold in pharmacy chains.
And further. If you decide to take medicinal herbs on your own, be sure to notify your doctor. The fact is that the simultaneous use of herbs and medications often has either an activating effect on the body, or, on the contrary, a leveling effect.
Can leeches help thin the blood? — In some cases, hirudotherapy is used. And as an adjuvant, leeches can help. Leeches, by injecting saliva containing many different enzymes (including hirudin), can improve the properties of blood and reduce its viscosity. In addition, the use of leeches has a mechanical effect on the body, which consists in reducing the amount of blood at the site of its attachment, which leads to a decrease in pressure and redistribution of fluid in the body.
But hirudotherapy does not help everyone. This method also has contraindications. Therefore, you can use it strictly according to your doctor’s recommendations.
What can you recommend to prevent “thick” blood? — The first thing you need to do is establish the correct drinking regime. Much is known about the dangers of dehydration. Lack of water affects not only the functioning of organs and systems, but also the viscosity of the blood. It is dehydration that often causes the development of hyperviscosity syndrome. To prevent it, it is recommended to drink at least 30 ml of clean water per 1 kg of weight daily. If for some reason a person does not drink plain water, but replaces it with tea, juices or compotes, then the volume of liquid consumed should be higher.
Smoking and drinking alcoholic beverages contribute to significant blood thickening. That is why people with “thick” blood are advised to give up these bad habits.
Regular physical activity is indicated. You need to move more, walk in the fresh air. Swimming and cycling are also suitable.
Prevention and treatment of chronic diseases is also necessary. Especially associated with the bronchopulmonary system, metabolic disorders, diabetes insipidus and diabetes mellitus, obesity, and improper functioning of the spleen.
And, of course, you need to eat right. After all, there are foods that provoke blood thickening. In particular, these are meat broths, sausages and smoked meats, jelly, white bread, cream, lentils, bananas and pickles.
Medicinal herbs should also be used with caution. For example, St. John's wort, valerian, nettle and yarrow can also provoke “thick” blood.
It is summer now. Is heat dangerous for those with “thick” blood? — Hot weather is a significant risk factor for blood thickening. It is especially dangerous for people in the risk groups I mentioned above. That is why it is so important, if possible, to avoid going outside in the heat, stay in a cool room and replenish fluid loss with sufficient drinking regimen.
Is donation harmful or beneficial for those whose blood is too thick? — If there are no contraindications to becoming a donor, become one! This way you will benefit not only people in need, but also yourself. After all, scientists have proven that blood viscosity after bloodletting decreases by 20–30%. And this is very good!