Symptoms
Elevated leukocytes in a child’s blood have their own clinical picture.
It is worth noting that the symptoms expressed in this disorder are nonspecific and cannot accurately indicate the course of this particular disorder. In addition, external manifestations characteristic of this condition may go unnoticed, since the symptoms of the underlying disease often come to the fore.
It is very difficult to determine the increase in the number of white blood cells in the blood of an infant. This is due to the fact that infants cannot describe their condition and sensations in words.
Symptoms that develop due to the fact that the child’s white blood cells have increased include:
- constant fatigue;
- loss of appetite;
- increase in temperature indicators;
- dizziness;
- profuse sweating;
- sleep disorder;
- slight decrease in visual acuity;
- muscle and joint pain;
- weight loss;
- frequent mood changes;
- increased moodiness and tearfulness in infants;
- problems with concentration in older children;
- decreased physical activity.
Such external manifestations are common to all age categories. The only difference may be the intensity of symptoms.
Diagnosis of leukocytosis
Why does a child under one year bleed from the nose?
With leukocytosis, the number of “white” blood cells increases compared to their normal value. The increase may be slight or severe.
Thus, the level of leukocytes increases after eating or during exercise. These are physiological processes and do not pose any danger. After a short period of time, the indicators return to normal. If such growth is considered as a pathological reaction of the body, we are talking about an inflammatory process.
The famous pediatrician Komarovsky recognizes the need for a general blood test. It, first of all, allows you to determine the nature of the disease, bacterial or viral. This is the basis for subsequent treatment. If the body is attacked by bacteria, then it will be difficult to cope without antibiotics, but they have no effect on viruses. Therefore, their use does not make sense, just like the use of antiviral drugs. Immunity to them is usually developed on days 6-7, and the body copes on its own. If this does not happen and the disease develops, most likely a bacteria has joined.
Possible symptoms in a child
When a child's white blood cell count is elevated, it not only indicates that he or she is sick, but also that the immune system is active. The body's defenses began to fight pathogenic microorganisms.
- Why do women have an increase in leukocytes in the blood?
The following symptoms may indicate leukocytosis in a child:
- Increased body temperature without identifying the cause;
- Weakness and dizziness;
- Indigestion, lack of appetite, weight loss;
- Nausea, vomiting;
- Headache and migraine;
- Aches in joints and muscles;
- Sleep disorder, most often insomnia. The child becomes anxious and shudders;
- Increased sweating;
- Moodiness and irritability.
An infant will not be able to talk about his health; parents only have to guess about existing problems. What should alert you is that the baby’s behavior has changed, he is not the same as before. When this happens once, and then the baby becomes himself again, then there is no need to worry. If the condition drags on, behavior and well-being worsen, then you need to consult a pediatrician.
Upset child
We must remember! In a baby, a temperature of up to 37.5° is considered normal. At the same time, he is calm and active, no unpleasant symptoms are observed. This is often due to uncomfortable indoor conditions and too warm clothing. If the temperature is higher and the baby begins to act up, you should consult a doctor.
And who is to blame for the infection?
When you know which blood cells are responsible for what, using a blood test to figure out what kind of infection has attacked the child this time is not easy, but simply simple. A high ESR and high leukocytes mean that the infection is in full swing and it must be treated immediately (in addition to these indicators, there is most often a temperature above 38C). High neutrophils mean that we have met another bacteria, and high lymphocytes mean a viral infection.
Everything is simple, as you can see. Now let's look at examples. And in order not to get confused in the numbers, we will simply say “a lot” or “a little”. Shall we try?
Acute viral infection
Signs . Leukocytes and ESR are higher than normal, in the leukocyte formula there is an excess of lymphocytes, a decrease in the number of neutrophils. Monocytes and eosinophils may increase slightly.
What to do ? Most often, doctors prescribe drugs containing interferon - viferon, kipferon or genferon.
Important! The so-called intracellular parasites - chlamydia and mycoplasma - behave exactly like viruses. They can be distinguished by the clinical manifestations of the disease. The “calling card” of both is a prolonged dry cough with an extremely unclear external picture - the child looks active, there is no wheezing in the lungs. However, the cough may last for weeks.
Chronic viral infection
Signs . The child is often sick, the blood has a normal ESR and normal (or even low) leukocytes. In the leukocyte formula, lymphocytes and monocytes float at the upper limit of normal. Neutrophils are at the lower limit of normal or even lower.
What to do? Examine the child for antibodies to Epstein-Bar viruses and cytomegalovirus. Most likely, these two are to blame.
Important! If the child has just had a viral infection, the blood test will be exactly the same. So, if a child gets sick twice a year and has just suffered a viral runny nose, it is somewhat premature to run to get tested for chronic viral infections.
Advertising
Acute bacterial infection
Signs. Leukocytes and ESR are higher than normal, in the leukocyte formula there is an excess of neutrophils (or even monocytes along with them) against the background of a decrease in the number of lymphocytes. Externally, signs of inflammation are visible, such as fever, purulent nasal discharge, wheezing in the lungs or a wet cough.
What to do? The most common medical prescriptions with such a blood test are antibiotics of the penicillin group (Augmentin, Flemoklav, Solutab, Suprax), less often - antibiotics of the azalide group (Vilprofen, Sumamed).
Chronic or local bacterial infection
Signs. All the same - increased neutrophils (not higher than the upper limit of normal) and decreased lymphocytes (also within normal limits, only closer to the lower limit). If there are such changes in blood tests, you will have to look for a local, not very active source of infection (Examination by an ENT doctor or an image of the paranasal sinuses; if a urinary tract infection is suspected, a general urine test).
Important! A blood test after a recent bacterial infection looks exactly the same.
What is leukocytosis and leukocyte norms in children
Eating leads to a transient increase in leukocytes
Leukocytosis is an increase in the number of leukocytes in the blood. The number of white cells in the bloodstream varies throughout the day. There are a little more of them after physical activity, emotional experiences, and eating food. But significant growth indicates the presence of a pathological process in the body.
The normal level of leukocytes directly depends on the age of the child. When a baby is born, it only encounters millions of bacteria, so its immune system works especially actively. The number of protective cells during this period is high, the immune system is just being formed. Gradually, having learned to fight harmful pathogens, leukocytes decrease in number.
- Leukocytosis (increased white blood cells in the blood): normal or pathological?
In the analysis form, leukocytes are abbreviated WBC. For a more reliable study, it is recommended to know not only the total number of leukocytes, but also the percentage of their varieties in the child’s blood (leukocyte formula).
White blood cell levels in children depend on age
| Age | Leukocytes (10^9/l) | Band neutrophils (%) | Segmented neutrophils (%) | Eosinophils (%) | Basophils (%) | Lymphocytes (%) | Monocytes (%) |
| 1 day - 1 month | 8,5 — 24,5 | 1 — 17 | 45 — 80 | 0,5 — 6 | 0 — 1 | 12 — 36 | 2 — 12 |
| 1 – 6 months | 6,5 — 13,5 | 0,5 — 4 | 15 — 45 | 0,5 — 7 | 0 — 1 | 40 — 76 | 2 — 12 |
| 6 – 12 months | 5,5 — 12,5 | 0,5 — 4 | 15 — 45 | 0,5 — 7 | 0 — 1 | 42 — 74 | 2 — 12 |
| 14 years | 6 — 12 | 0,5 — 4 | 15 — 45 | 0,5 — 7 | 0 — 1 | 38 — 72 | 2 — 12 |
| 4 – 7 years | 5 — 12 | 0,5 — 5 | 25 — 60 | 0,5 — 7 | 0 — 1 | 25 — 60 | 2 — 10 |
| 7 – 12 years | 4,5 — 10 | 0,5 — 5 | 35 — 65 | 0,5 — 7 | 0 — 1 | 24 — 54 | 2 — 10 |
| 12 – 15 years | 4,3 — 9,5 | 0,5 — 6 | 40 — 65 | 0,5 — 6 | 0 — 1 | 22 — 50 | 2 — 10 |
Red blood: what is it?
Yeah. The blood test is divided into two parts. The first part is the so-called “red blood”, that is, hemoglobin, red blood cells, platelets and color index. All this fraternity is responsible for the transfer of oxygen into cells and does not suffer much during infection. You and I just need to quickly go through the standards and, making sure that everything is fine, move on to the second part.
Norms
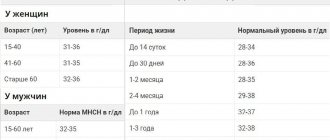
Hemoglobin (aka Hb) is measured in grams per liter (!) of blood and is responsible for the transport of oxygen.
A one-month-old child has a hemoglobin norm of 115-175 (this is not an adult, everything is more complicated here), at six months - 110-140 - the same as you and I, and so, in fact, right up to 10-12 years. 110-140 (145 according to other sources) grams per liter of blood.
Red blood cells , also known as RBCs, are cells in which hemoglobin floats in the blood. They carry oxygen with the help of hemoglobin. The norm for a child per month will be 3.8-5.6 - attention! - trillions of red blood cells per liter of blood. A one-year-old child (like an adult) already has fewer of these same trillions - 3.5-4.9 per liter of blood. What to do - if you pump out blood for analysis in liters, everything has to be counted in trillions. No problem, it will be easier next time.
Reticulocytes , also known as RTC, their number is measured, thank God, as a percentage. These are, so to speak, young red blood cells; they should not be more than 15% in children under one year old and no more than 12% in children over one year old or in adults. The lower limit of normal for reticulocytes is 3%. If there are fewer of them, the child is on the verge of anemia, and measures must be taken as soon as possible.
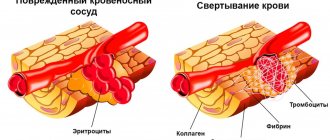
Platelets . English abbreviation PLT. There are significantly fewer of them than red blood cells - their number is measured “only” in billions per liter of blood, the norm is from 180 to 400 for children under one year old and from 160 to 360 for children over one year old or in adults. Platelets are actually not cells at all, but rather fragments of a giant precursor cell, from these fragments, in which case blood clots are formed - for example, to stop bleeding if the baby, God forbid, gets injured.
ESR (ESR). These are not even cells at all, but an indicator of the erythrocyte sedimentation rate - the higher this rate (and this is not a car, here the speed is measured in millimeters per hour), the more active the inflammatory process, for which you may have been recommended to take a blood test. ESR norms at 1 month are 4-10, at 6 months 4-8, but from one year to 12 years - from 4 to 12 mm per hour. Then the norms of that same ESR will also differ depending on gender, but that’s a completely different story.
In addition to these indicators, there are many others - hematocrit (HCT), red blood cell distribution width (RDWc), mean erythrocyte volume (MCV), mean erythrocyte hemoglobin content (MCH) and even mean erythrocyte hemoglobin concentration (MCHC). All these indicators serve to diagnose anemia, so it would be better for you and me (we are talking about infections, remember?) to postpone their discussion until later.
What is much more important for us is not the oxygen transport system, but the body’s defense system against infections. This is the so-called white blood, leukocytes. Here we will dwell on it in very, very detail.
How to treat leukocytosis?
Treatment can be prescribed only after the exact cause of this phenomenon has been established, for example, physiological leukocytosis is considered to be the norm. As soon as the causative agent of the infection is detected, the following drugs may be prescribed to the small patient:
- Antiviral agents that effectively fight viruses.
- In severe cases, antibiotics may be prescribed, but they are taken only as prescribed by a doctor.
- Chemotherapy drugs that are aimed at maintaining the immune system.
Sometimes, when leukocytosis is detected in children and the blood has a viscous consistency, leukapheresis is prescribed, during which the blood is purified.
How is the analysis performed?
When testing blood for a general or, as it is also called, clinical analysis, the child should, if possible, be hungry, i.e., the procedure is done on an empty stomach. Typically, blood collection rooms in clinics are open from 8.00. until 9.30. At this time, blood levels in the body are the most optimal.
Blood must be donated on an empty stomach, because after eating, the stomach begins to work actively and the number of leukocytes may increase, and this, in turn, may give the doctor incorrect information about the child’s health status. Also, before taking the test, you should not undergo any procedures, such as x-rays, FGDS and various physiotherapeutic procedures, this can also lead to an increase in leukocytes in the blood. [adsen]
Grodno Regional Children's Clinical Hospital
Details Published May 31, 2016
Head of KDL Rachkovskaya I.E.
Age-related features of a general blood test in children
A general blood test is considered one of the most accessible, simple and informative research methods that are used in children of any age, starting from the moment of birth.
Throughout the entire period of childhood, regular age-related features are revealed in the blood system. There is a characteristic dynamics of changes in hemoglobin, red blood cells, leukocytes and other hematological parameters in the first days, months and years after birth. Thus, the number of red blood cells and hemoglobin content in a child at birth is greater than in an adult, which is explained by the so-called placental transfusion and hemoconcentration. The hemoglobin content at birth in full-term infants is 180-217 g/l, in premature infants it is 145-225 g/l. Red blood cells at birth are 4.5-7.8x1012/l.
During the first week of life, hemoglobin levels begin to decline. Its minimum level is observed at 2-6 months of age and during this period is 100-130 g/l. Similar dynamics are observed on the part of red blood cells, the number of which by the end of the first half of the year reaches 3.1-4.6x1012/l. This decrease in hemoglobin concentration and the number of red blood cells is the result of increased hemolysis of fetal red blood cells (life expectancy of red blood cells in a newborn is 60-70 days) and a low level of production of red blood cells by the hematopoietic organs. The latter is due to the low production of erythropoietin, a factor that stimulates the differentiation of erythroid cells during the transition from relative intrauterine hypoxia of the fetus during placental circulation to arterialization of blood in the lungs, when blood oxygen saturation increases sharply (from 45% in utero to 95% after birth). Newborns in the first week of life are characterized by: red blood cells of large volumes (macrocytosis). In a general blood test, this indicator is designated as MCV, red blood cells with increased thickness (hyperchromia) MCH, and reticulocytosis (3-50%); which by 7-8 days of life decrease significantly. Macrocytosis and hyperchromia, characteristic of the first days of life, subsequently disappear, and at the age of 2 months to 2 years, MCV and MSI indicators are lower than the corresponding indicators for adults. MCV is 70-85 at this age, and MCH is 26-30. By 5 years, MCV and MSI levels are the same as in adults. The number of leukocytes at birth fluctuates between 8.5 and 25x109/l, then quickly falls, and by the 15th day it is 9-14x109/l. Subsequently, the number of leukocytes gradually decreases and by the age of 5 reaches the level of an adult. The number of neutrophils during the first days of life prevails over the number of lymphocytes. During the first 3 days, young cells may be found in the blood count. Subsequently, the number of neutrophils begins to decrease, while the number of lymphocytes increases. By day 5-6, the percentage of neutrophils and lymphocytes is equalized and amounts to 45% each. This is regarded as the “first cross” in the leukocyte formula in children. By three months of life, the number of neutrophils decreases to 16-46%, and lymphocytes increases to 42-74%. At the age of 4-5 years, children experience lymphocytosis due to the formation of their immune system. Then the number of neutrophils begins to increase and the number of lymphocytes to decrease, and at the age of 5-6 years a “second crossover” is observed, when the number of these cells is equalized again. By the age of 12-14 years, the leukocyte formula of children is similar to that of adults. ESR in newborns is somewhat slow: from 1.5-4 mm/h on the 1st day and up to 2.0-8.0 mm/h on the 2nd week. Over the course of 1 year of life, ESR fluctuates on average between 2-10 mm/h, and subsequently 2-12 mm/h. The number of platelets at birth is on average 180-490x109/l, then their number drops and at 1 year of life it is 150-450x109/l (as in adults). It is important to remember that changes in the blood only indicate that a certain pathological process is occurring in the body, the origin and cause of which, as a rule, is easy to understand if you compare the symptoms of the disease, their duration, the presence of similar diseases in the family, factors that could contribute to the occurrence of the disease and, if necessary, data from other research methods. The doctor, deciphering the results of a clinical blood test, carries out complex mental work, the result of which will be making a diagnosis and prescribing appropriate treatment. At the same time, it should be noted that small deviations from the norm of some indicators in a general blood test do not indicate the presence of any disease or condition; in each specific case this is decided individually after examination by a doctor.