Local therapist
Ablyazov
Irshat Ravilevich
21 years of experience
Local therapist of the highest category. Member of the Russian Scientific Medical Society of Therapists.
Make an appointment
Thrombocytopenia is a separate disease or a symptom of another disease that is characterized by a low platelet count (less than 150,000 units per microliter). The condition is accompanied by high bleeding, as well as slow stopping of bleeding from small vessels.
Symptoms
Symptoms of thrombocytopenia include:
- Purpura. This is the name for hemorrhages in mucous tissues or skin. In fact, it looks like red spots - most often they can be seen in places of strong contact with clothing. The spots do not hurt, they can be pinpoint or quite extensive - including bruises of different colors (depending on the time of formation).
- Regular nosebleeds. Since small vessels are weakened, bleeding can begin due to a cold, sneezing, or minor injury. Bright red blood may flow for ten minutes or more, putting the patient at risk of losing a lot of blood.
- Bleeding gums, prolonged bleeding after tooth extraction. The mechanism is the same: due to weak blood vessels, the blood cannot stop quickly in case of small or large injuries.
- Bleeding of internal organs. For example, blood is found in the gastrointestinal tract, when the stool becomes colored, or in the genitourinary system - then the urine becomes colored. Both symptoms are very alarming and require immediate contact with specialists.
- Too heavy and long menstruation. Moreover, bleeding can be observed on other days of the cycle.
All of these symptoms may indicate other diseases - both concomitant with thrombocytopenia and independent. What complicates the situation is that there are a lot of reasons and mechanisms for the development of this condition. In medicine, there are several types of this disease.
How to avoid bleeding
Cancer and cancer treatments can cause low platelet counts. When your platelet count is low, you are at risk of bleeding. If your doctor has told you that you have a low platelet count, it is important to try to avoid injury.
We will list some general tips that can help you prevent bleeding. It is also very important to discuss your lifestyle with your healthcare professional. They may suggest other ways to prevent bleeding if your platelet count is low.
Personal care
- Do not use sharp objects such as straight razors, scissors or nail clippers. You can use an electric razor.
- Do not: manicure or pedicure;
- waxing;
- electrolysis;
- tattoos
- rectal suppositories (medicines that are inserted into the anus);
Dental care
- Use a brush with soft bristles.
- Consult your doctor before starting dental treatment.
Daily Activities
- Wear gloves when doing gardening, cooking, or making repairs at home.
- Avoid activities that could cause injury. These include: contact sports;
- climbing a stepladder;
- intense physical exercise;
- Biking;
- lifting weights.
- use lubricants if necessary;
Medicines
- Do not take: aspirin or medications containing aspirin;
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil®, Motrin®) and naproxen (Aleve®);
- vitamin E
to come back to the beginning
Classification of thrombocytopenia
Let's talk about the causes of thrombocytopenia that underlie the different types of this disease.
Hereditary thrombocytopenias
These conditions are based on diseases of genetic origin. These may be May-Hegglin anomaly, Bernard-Soulier syndrome, Wiskott-Aldrich syndrome, TAR syndrome, as well as congenital amegakaryocytic thrombocytopenia.
Each of these diseases has many characteristics. For example, Wiskott-Aldrich syndrome occurs exclusively in boys and occurs in four to ten cases per million. Bernard-Soulier syndrome can only develop in a baby who has received the altered gene from both parents, and May-Hegglin anomaly can develop in 50% of cases, provided that only one parent has the prerequisites for this. As a rule, all of these diseases have among their symptoms not only a low level of platelets, but also a number of other pathological conditions, and therefore require special treatment.
Platelet diagnostics
At the first appearance of relevant clinical symptoms (bleeding and bruising), it is necessary to consult a specialist, in this case it is a general practitioner. There is no need to postpone going to the doctor until the clinic gets worse, because in this case the treatment will be more difficult and the outcome will be less favorable.
To diagnose thrombocytopenia, you must first take a blood test. If the analysis reveals a low platelet count, the general practitioner may refer you to a hematologist, who will prescribe additional tests, such as:
- Coagulogram with determination of clotting time.
- Blood biochemistry for LDH, ASAT, ALAT and bilirubin.
- Antibody test.
- MRI.
- Ultrasound of the abdominal organs.
- Genetic studies (to exclude hereditary thrombocytopenia).
After conducting research and identifying the true cause of thrombocytopenia, a general practitioner or hematologist prescribes appropriate treatment, which includes eliminating the cause of the decrease in platelet count.
Online consultation with infectious disease specialist, allergist-immunologist Natalia Nikolaevna Gordienko
consultation cost: 1000 rubles
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
Productive thrombocytopenia
They are also caused by a huge list of reasons and factors of various origins. All of them are associated with the fact that platelet formation processes in the red bone marrow are disrupted.
For example, this includes some types of anemia, cancer metastases, acute leukemia, and taking cytostatic medications. There are even factors such as radiation or alcohol abuse.
For example, in acute leukemia, a disease of the circulatory system causes a mutation in the bone marrow stem cell. Because of this, it divides and begins to displace hematopoietic cells. As a result, the number of not only platelets, but also leukocytes, erythrocytes, and lymphocytes decreases. This condition has its own name - pancytopenia. That is, immune thrombocytopenia in this case is part of it.
If we are talking about the effect of medications, then most often a decrease in platelet levels is caused by drugs from the following groups:
- antidiabetic,
- anti-inflammatory,
- antipsychotics,
- antithyroid,
- antibiotics,
- diuretics,
- anticonvulsants.
Of course, not all medications and not in all cases are capable of causing such a reaction, but this is another reason to think about the fact that you should not prescribe any medications yourself or take them without the supervision of your doctor.
Moreover, there is also such a factor as increased sensitivity to certain medications. Usually it is initially determined by a peculiar genetic predisposition, but this is quite rare.
When we talk about radiation, we are talking not only about a person’s presence in dangerous areas, but also about treatment with radiation therapy. When tumors are destroyed, the blood-forming cells of the red brain can be affected, so a condition where platelet levels drop can become a side effect of cancer treatment.
The development of symptoms of thrombocytopenia due to alcohol abuse most often occurs against the background of binge drinking and is associated with a high level of ethyl alcohol in the blood. It has negative and long-lasting effects on the bone marrow and usually causes a temporary decrease in platelets. If binge drinking becomes frequent and too long, there is a risk that the changes will be irreversible.
Causes of the disease
Causes of thrombocytopenia include:
- Hereditary diseases. Bernard-Sourya syndrome, TAR syndrome, May-Hegglin anomalies and other diseases that can provoke pathological bleeding.
- Diseases that interfere with the creation of new platelets. Most often, this is due to bone marrow problems, cancer, reactions to chemical and radioactive elements, and leukemia. And sometimes even against the background of alcohol and drug abuse.
- Diagnoses that provoke excessive consumption of platelets by the body. A striking example of such a disease is DIC syndrome. There is an increase in platelet consumption, and as a result, the bone marrow increases its work on the formation of new cells. Over time, he gets tired, his reserves are depleted and thus new platelets do not appear in the blood.
- Increased size of the spleen. The fact is that a large number of platelets are stored in the spleen, as if in a depot. But when its size is pathologically large, it takes on too many cells, which leads to a decrease in them in the blood, and the bone marrow, in turn, does not compensate for the deficiency.
- Autoimmune thrombocytopenia. It develops when the body begins to destroy platelets in the blood.
- Drug-induced thrombocytopenia. Some groups of drugs can destroy platelets or suppress their formation in the bone marrow. For example, long-term use of cytostatics.
Many drugs can cause thrombocytopenia, but it is still quite rare. According to research, about 10 cases per 1 million population per year. (https://pubmed.ncbi.nlm.nih.gov/15588119/)
Thrombocytopenia destruction
Here we are talking about the active destruction of platelets, which is usually observed in the spleen. Such processes are also caused by a large number of factors. These include taking certain medications, some viruses, Fisher-Evans syndrome, etc.
Idiopathic thrombocytopenia deserves special consideration. This is the case when it is not possible to establish the cause even with a huge number of possible options. At the same time, doctors note that even in such a situation, the action of provoking factors is observed. For example, the problem appears after bacterial and viral infections, preventive vaccinations, use of a number of medications, hypothermia or prolonged exposure to the sun.
This condition also occurs in newborns. It begins to form in the womb, when antibodies in her body cause the destruction of platelets in the child.
Fisher-Evans syndrome is also not an independent cause, since it itself is a consequence of various systemic diseases. This syndrome occurs in systemic lupus erythematosus and rheumatoid arthritis, but in some cases it can be an independent deviation. As for viruses, rubella, chicken pox, measles, and influenza can lead to a decrease in platelet levels. Sometimes this is a reaction to vaccination, although such a mechanism is described quite rarely and almost never occurs.
Prevention
There is no specific prophylaxis for thrombocytopenia. It is recommended to lead a healthy lifestyle, including proper nutrition, normal sleep, not to overload yourself with work, abstain from drinking alcohol and tobacco products, treat infectious diseases in a timely manner and carry out routine vaccinations. Consult a doctor promptly if there is a sudden disturbance in the body’s functioning.
Author: infectious disease doctor. Allergist-immunologist Natalia Nikolaevna Gordienko
Thrombocytopenia consumption
Here the mechanism is as follows: platelets, for some reason, begin to be activated in the vascular bed. In response to this, the red bone marrow begins to actively produce them - and as a result, its capabilities are slowly depleted. After this, the level of red cells begins to fall.
One of the causes of consumption thrombocytopenia is disseminated intravascular coagulation syndrome. It stands for disseminated intravascular coagulation syndrome. And it can develop against the background of severe tissue destruction during operations, burns, injuries, due to severe infections, chemotherapy, organ transplants, etc. That is, there are many underlying reasons that can cause a decrease in the level of platelets in the blood.
Increased and decreased platelets in the blood
We continue our series of publications on laboratory blood tests. On our portal you can find useful information on how to independently decipher indicators in general and biochemical analyses, as well as in the lipid profile. This time Dr. Fedorov answers questions about platelet levels in the blood. If you still have questions, you can ask them using the Doctis service.
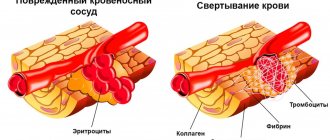
The ability of blood to clot is one of the foundations of life. After all, if this mechanism had not been laid down, any, even the most insignificant wound, would become mortally dangerous. A number of biochemical compounds, which are usually called factors, are responsible for the coagulation system, but the basis of the process is the smallest formed elements of blood - platelets. Unfortunately, disruption of this system can lead to consequences no less serious than bleeding.
An excess of platelets threatens to increase the risk of intravascular thrombus formation; low platelets in the blood are the cause of internal hemorrhages.
1. What does a decrease in platelet levels in the blood indicate?
The lower limit of normal blood platelet content is 150 thousand/μl. The reason for the decrease in PLT (platelet designation in a blood test) may be numerous but rare congenital thrombocytopenias (Fanconi syndrome, Wiskott-Aldrich, etc.), as well as acquired thrombocytopenias. The most common cause of acquired ones is the constant use of antiplatelet drugs, especially with two-component therapy (acetylsalicylic acid + clopidogrel); fortunately, the number of platelets in this case is usually not greatly reduced. Other causes of low blood platelets include bacterial and viral infections, anemia, splenomegaly, congestive heart failure, etc.
Clinical signs of platelet deficiency (bleeding gums, bruising, frequent hemorrhages in the sclera, etc.) appear when the platelet level drops below 50 thousand/mcL - this is the indicator when you need to see a doctor immediately.
2. What does an increase in platelet levels in the blood indicate?
The upper limit of normal platelets in a blood test is 400 thousand/µl. Increased platelet levels are much more likely to occur for physiological reasons. These are so-called reactive thrombocytosis. Their cause may be recent physical overexertion, past stress, dehydration, that is, physiological thickening of the blood. Pathological factors most often include those that also thicken the blood - anemia due to chronic blood loss or acute blood loss, dehydration as a result of intoxication. The reasons for an absolute increase in platelet levels include inflammatory diseases, tuberculosis, malignant neoplasms in general and the hematopoietic system in particular.
An increase in platelet levels above 500 thousand/µl significantly increases the risk of thrombosis and requires the selection of antiplatelet therapy - the use of special drugs.
3. How does a blood clot form? Why is a test for induced platelet aggregation prescribed?
Normally, platelets in the blood are in an inactive state; the cells have a disc-shaped, slightly elongated shape, which is why in old textbooks they are called “blood plates.” When bleeding begins, platelets are activated: they acquire a spherical shape and form special outgrowths - pseudopodia. With their help, they can connect with each other (aggregate) and stick to the site of damage to the vascular wall (adhere). These two processes provide the basis for thrombus formation.
To assess the quality of platelet aggregation and find out whether it is reduced or, conversely, does not occur too intensely, an analysis for induced platelet aggregation is prescribed. To do this, they take blood from a vein, add special substances (activation inducers) to it and evaluate the process.
When preparing for the study, it is important to comply with certain conditions - for 3 days, follow a special diet prepared by a doctor, 24 hours before, avoid taking stimulants (coffee, alcohol, nicotine, garlic) and immunostimulant drugs, 8 hours before, stop taking medications and fatty foods.
Low platelet activity occurs in diseases of the hematopoietic system, constant use of antiplatelet drugs, in this case the duration of bleeding increases. Increased aggregation, on the contrary, increases the risk of thrombosis: venous thrombosis, heart attack, stroke. You may ask, why order an induced activation test if the risk of bleeding/thrombosis can be assessed by the total platelet count? Alas. Even with normal numbers, most of the cells may turn out to be “defective”, so we are talking about severe platelet deficiency with their normal concentration in the blood.
4. Why is it important to order a blood test for platelet resistance to aspirin and clopidogrel?
According to research, 35% of people have a reduced antiaggregation effect when using aspirin, and in 19% it has virtually no effect on aggregation. This means that in every fifth patient, aspirin does not help avoid complications of atherosclerosis. Less common, but no less clinically important, is resistance to clopidogrel, a drug that is vitally important to take after arterial stenting. Therefore, it is considered justified to order a test for aspirin and clopidogrel resistance before prescribing these drugs, especially when stenting of the coronary arteries is planned. To diagnose aspirin resistance, two tests are used today: optical aggregometry, which is considered the “gold standard,” as well as several types of portable test systems. A similar approach is used to diagnose resistance to clopidogrel, which, according to studies, is registered in 11% of patients receiving the drug. If resistance is detected, doctors have room for maneuver - to prescribe a drug from another group and avoid dangerous complications.
The platelet level allows you to assess both the risk of thrombosis and, conversely, the likelihood of insufficient blood clotting, which threatens the development of internal hemorrhages and bleeding. Studying platelet function gives the doctor the opportunity to correctly select antiplatelet therapy - an essential component of the prevention and treatment of cardiovascular diseases.
Thrombocytopenia redistribution
If we explain this mechanism very simply, it looks like this: due to some reasons, the patient’s spleen enlarges. And if under normal conditions it stores up to 30% of platelets, then in an enlarged state it retains up to 90% of these cells. At the same time, the system does not see that there are not enough platelets and does not trigger a compensatory mechanism.
The mechanism is also based on various causes: cirrhosis of the liver, some infections such as tuberculosis, autoimmune diseases (systemic lupus erythematosus), tumors of the circulatory system, alcoholism.
Treatment
If your platelet count is 10,000 microliters or less, you may need a platelet transfusion to increase your platelet count.
You may also need a transfusion if your platelet count is more than 10,000 microliters, but you are bleeding heavily, are having an invasive (involving going inside the body through an incision, cut or puncture) procedure, or have signs of other problems.
If you experience heavy menstrual bleeding, consult your doctor.
You may need to start hormonal therapy with birth control pills to prevent your next menstrual bleeding. to come back to the beginning
Thrombocytopenia dilution
This condition is usually observed in people who receive a large number of transfusions of various liquids: for example, plasma, plasma substitutes, etc. As a result, the level of platelets decreases due to the banal dilution of the blood.
Considering the huge number of reasons that can cause immune thrombocytopenia (and we have not named all the options), a patient with its symptoms should immediately consult a doctor who will find the essence of the problem and prescribe effective treatment.
Treatment of thrombocytopenia
Thrombocytopenia is treated by a hematologist. The treatment regimen is developed individually for each patient: the patient’s age, the presence of any diseases, the degree of deficiency, and the amount of bleeding are taken into account. It is necessary to determine the cause of thrombocytopenia so that treatment is as effective as possible. Standard drug therapy consists of:
- Corticosteroids – have anti-inflammatory and analgesic effects;
- Immunoglobulins – correct the functioning of the immune system;
- Immunosuppressants – stop the destructive effect of the immune system on the body;
- Agonists to thrombopoietin receptors – promote more active production of this hormone.
In case of thrombocytopenia caused by bleeding, it is necessary to identify the source of this bleeding and stop it. Only after this the platelet correction is carried out. The patient will have to take medicinal iron and drugs that promote the production of red blood cells.
If drug treatment does not produce any results, splenectomy is indicated - surgical excision of the spleen. For hereditary diseases that prevent the body from producing enough platelets, a bone marrow transplant is necessary. If the platelet level is critically low, a blood transfusion of platelet mass from a donor is performed. If a large volume of blood is lost, a transfusion of fresh frozen plasma and red blood cells is necessary.
Diagnostics
Since there are so many reasons, it is not possible to name diagnostic measures in detail - everything will depend on the specific situation. But we can highlight the main components of diagnosis:
- General blood analysis.
- Checking bleeding time (Duke test).
- Determining the time it takes for blood to clot.
- Red bone marrow puncture. The method allows you to identify quantitative and qualitative changes in cells.
- Determination of antibodies in blood.
- Research for genetic diseases.
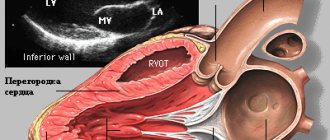
- Ultrasound of internal organs. Most often, the liver and spleen are studied immediately, but this list can be very large.
- MRI. Used to study internal organs and blood vessels.
Diagnosis of the disease begins with a visit to a general practitioner, who, based on a survey, initial examinations and tests, prescribes visits to other specialists.
Blood test for platelets
A complete blood test can determine the platelet count. The main indications for its implementation are the following:
- Increased bleeding of gums.
- Heavy menstruation.
- The appearance of bruises from minor impacts.
- Frequent nosebleeds.
- Difficulty stopping bleeding from minor injuries.
The number of platelets in the blood is measured in thousands per 1 microliter of blood. Counting is carried out in specialized laboratories in various ways that guarantee high accuracy.
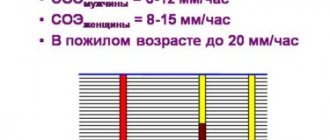
The normal platelet count in the blood depends on gender and age and is:
- For men, 200–400 thousand.
- In women, 180–320 thousand, during menstruation the amount can decrease to 75–220 thousand, and during pregnancy to 100–310 thousand.
- In children, indicators depend on age, and the corresponding values are given in special tables.
To conduct a general blood test, blood is taken from a finger. No special preliminary preparation is required before this. To ensure accurate results, it is better to donate blood in the morning on an empty stomach. At the same time, 12 hours before the procedure it is not recommended to consume fatty spicy foods, carbonated drinks, and alcohol.
Additionally, to determine blood clotting indicators, Sukharev and Lee-White tests are performed. They are informative and allow you to obtain the necessary additional data about the pathological condition. This will allow you to carry out correct treatment measures and avoid dangerous consequences.
Treatment and severity
Treatment of thrombocytopenia most often comes down to identifying the primary disease and its treatment, as well as eliminating various unpleasant symptoms. In the process, it is also important to take into account that the severity of thrombocytopenia varies:
Mild degree. It assumes that the platelet concentration is from 50 to 150 thousand units per microliter. The condition of the capillaries is usually normal, bleeding does not develop. Usually, treatment is not necessary at this stage - doctors recommend waiting and monitoring the development of the patient’s condition.
Average degree. In this case, the concentration is 20-50 thousand platelet units per microliter. Under this condition, bleeding gums and nosebleeds are observed. If injuries and bruises occur, serious hemorrhages form in the skin. At this stage, drug therapy may be prescribed.
Severe degree. The platelet concentration is below 20 thousand, hemorrhages are spontaneous and severe. At the same time, the patient himself may feel quite comfortable, does not complain of feeling unwell, but tests show that he needs help.
Since the treatment of thrombocytopenia requires the most thorough and detailed diagnosis, it is important to choose a modern clinic that will help you. JSC "Medicine" in Moscow is just the place where you can get qualified help from the best specialists. The clinic has everything necessary for both examination and treatment of each patient.
Prognosis and prevention
Thrombocytopenia is a dangerous disease that poses a huge threat to the life and health of the patient. Anemia often develops, and vision loss can occur due to hemorrhages in the retina. Advanced forms can provoke hemorrhages in the internal organs and in the brain. In most cases this leads to death.
Thrombocytopenia has no specific prevention. Experts give the following recommendations:
- Take a general blood test every year and undergo a general medical examination;
- Eat properly and nutritiously: eat as much meat and fresh vegetables as possible;
- Play sports and lead an active lifestyle;
- Avoid self-medication: taking aspirin and steroid drugs should be under the strict supervision of a doctor;
- Try to avoid any procedures where there is a risk of cutting (shaving, manicure);
- Treat any infectious processes in a timely manner;
- Take precautions when working with chemicals;
- Give up bad habits: drinking alcohol slows down platelet production.
Thrombocytopenia is a disease that requires constant medical supervision. If you suspect you have it or know about the pathology and want to get rid of it, contact the Medscan medical center. Experienced doctors will perform the necessary diagnostics and develop an individual treatment plan.