Sudden cardiac death and its prevention
Coronary death
Coronary death refers to death that occurs as a result of the cessation of effective heart function. As a rule, in this case, either ventricular fibrillation or primary cardiac arrest develops. In almost 90% of cases, acute coronary death is caused by coronary heart disease. It also happens that before this, IHD did not manifest itself in any way, that is, it was asymptomatic. In some cases, the patient was bothered by angina attacks and arrhythmia. After a heart attack, the risk of sudden death increases several times.
Manifestations and course of coronary death
Autopsies of patients who died suddenly usually reveal damage to the coronary arteries by atherosclerotic plaques. In this case, the lumen of the vessel narrows by 70% or more. Very often, on the damaged surface of the vessel there is a thrombus that has completely stopped blood flow in a fairly large area of the heart muscle. Usually, signs of myocardial infarction cannot be identified, since too little time has passed since the onset of the disease. Histological examination can reveal signs of incipient necrosis and cell restructuring.
Due to electrical instability of the myocardium, life-threatening arrhythmia occurs (asystole or ventricular fibrillation). Blood flow stops, including through the cerebral arteries. In this regard, the person quickly loses consciousness and falls. Noisy wheezing breathing and foam at the mouth may appear. After a few minutes, the muscles will begin to twitch involuntarily. The skin becomes pale, cyanosis of the lips and limbs is observed. The pulse and breathing stop completely, the pupils dilate and stop responding to light.
Help with cardiac death
Sudden coronary death leads to irreversible changes in the cerebral cortex within 5-6 minutes. Therefore, emergency measures to restore blood flow must begin immediately and continue until the arrival of the medical team.
Every person needs to know the basics of cardiopulmonary resuscitation. Her tasks include checking and, if necessary, restoring the patency of the airways, starting artificial ventilation (mouth-to-mouth, mouth-to-nose), and chest compressions. According to the latest recommendations, a person without experience can skip the first two points and immediately begin cardiac massage. Several studies have shown that this approach is more effective and leads to improved survival.
Indirect cardiac massage should be performed as follows:
- Place the person on their back on a hard surface;
- Place your palms on the middle third of the sternum perpendicular to it;
- Start squeezing your chest without bending your elbows;
- In this case, the sternum should bend by 5 cm, and the frequency of movements should be about 100 per minute.
The effectiveness of resuscitation measures can be judged by the color of the skin.
Prevention of sudden coronary death
To prevent cardiac death, it is necessary to influence the main provoking factors, among which the most important are:
- Myocardial ischemia;
- Decrease in left ventricular ejection fraction;
- Various arrhythmias.
To eliminate oxygen starvation of the heart, adequate drug therapy is necessary, including the main classes of drugs to improve coronary blood flow (nitroglycerin, beta blockers, aspirin, statins).
If necessary, endovascular restoration of artery patency should be performed. A special balloon is inserted into the affected area through a puncture in the femoral artery, inflated, and then a spring (stent) is installed, which prevents further narrowing of the vessel.
If such an operation cannot be performed for any reason, coronary artery bypass grafting is performed with opening of the chest and connection to a heart-lung machine. In this case, additional vessels (the person’s own arteries and veins, taken from an arm or leg) are sewn from the aorta to the coronary arteries. Recovery after this operation is longer, but the prognosis is favorable.
If myocardial contractility decreases, special devices can be installed to increase it. Special medications, such as digoxin, are also prescribed.
To prevent arrhythmia, in particular ventricular fibrillation, a cardioverter-defibrillator is installed. It is a miniature device that is placed under the skin in the chest area. Using special wires, it is connected to the myocardium and, if an arrhythmia occurs, it restarts the heart using a discharge. It should be remembered that with asystole this device will be ineffective.
Unfortunately, coronary death is a rather insidious disease, and it is not always possible to identify potential patients. That is why the most important thing in the fight against this condition is the timely implementation of emergency measures. Nowadays, many public places have defibrillators that can be used for life-threatening arrhythmias. They also often conduct special courses on teaching resuscitation measures to ordinary citizens.
RISK FACTORS FOR SUDDEN DEATH
Sudden cessation of blood circulation (“cardiac arrest”, clinical death) occurs most often as a result of diseases of the cardiovascular system. The cessation of blood circulation leads to the death of cells in the cerebral cortex, which cannot exist without a constant supply of oxygen for more than 5 minutes. The time frame originally used to describe sudden death was 24 hours. Now they have been reduced to 1 hour.
The risk factors for sudden death are essentially the same as for coronary heart disease.
1. Arterial hypertension and left ventricular hypertrophy
First of all, left ventricular hypertrophy. The risk of sudden death increases with increasing myocardial mass.
2. Lipids
The connection between high cholesterol levels and the risk of sudden death is well established and proven, although there is no reliable data on reducing this risk when lipid levels are normalized.
3. Nutritional features
Most epidemiological studies have not found a clear association between the risk of sudden death and any dietary characteristics.
4. Physical activity
The risk of sudden death is higher both in people who do not regularly engage in strenuous exercise and in people with a lack of physical activity.
5. Alcohol addiction
Severe alcohol dependence and especially binge drinking increase the risk of sudden death. However, moderate alcohol consumption reduces the risk of sudden death (30 g of ethanol per day).
6. Heart rate and heart rate variability
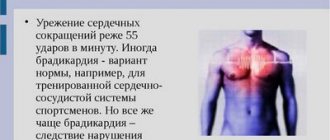
An increase in heart rate is an independent risk factor for sudden death. This may be due to a decrease in parasympathetic activity. Heart rate variability is an indicator associated not only with cardiac, but also with non-cardiac causes of death, so its relationship with the risk of sudden death cannot currently be assessed.
7. Smoking
Smoking is an independent risk factor for sudden clinical death and for the development of myocardial infarction. For persons with a history of circulatory arrest, continued smoking after discharge from hospital is also an independent risk factor for repeated sudden circulatory arrest.
8. Diabetes mellitus
To date, there is no convincing evidence that diabetes mellitus is an independent risk factor for sudden death.
9. Changes on the ECG
A large number of studies have noted a clear connection between ECG changes such as ST segment depression and T wave changes with cardiac death in general and sudden death in particular. Prolongation of the QT interval in individuals without heart disease is also an unfavorable prognostic factor for the development of cardiac death. Similar facts have not been proven regarding QT interval dispersion.
10. Genetic basis
Long QT syndrome, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, polymorphic ventricular tachycardia, dilated cardiomyopathy are inherited in a monogenic manner and have a clear predisposition to sudden death.
The cause of sudden death is often ventricular fibrillation (VF) 75-80% and ventricular tachycardia (VT), less often electromechanical dissociation (EMD) and asystole. Circulatory arrest usually occurs at home (2/3 of cases), in men over 50 years of age (3/4 of cases) during the day (8-18 hours).
All risk factors for coronary heart disease
Since in most cases sudden cardiac death is caused by ischemic disease, it is clear that almost all risk factors for coronary heart disease are also risk factors for sudden death. The greatest importance belongs to such factors as old age, arterial hypertension, left ventricular hypertrophy, tobacco smoking, high blood cholesterol, excess body weight, nonspecific electrocardiographic changes. The risk of sudden cardiac death increases especially significantly when several risk factors are combined.
Previous myocardial infarction
Myocardial infarction is an important risk factor for sudden cardiac death. The potential risk of sudden cardiac death in the first 72 hours from the onset of a heart attack ranges from 15 to 20% of cases. The highest risk of sudden cardiac death is observed in patients with myocardial infarction between 3 days and 8 weeks if the course of the disease was complicated by ventricular tachycardia or atrial fibrillation, or if paired, salvo, early ventricular extrasystoles, or repeated episodes of salvo ventricular extrasystoles were recorded. When heart rate is normalized and left ventricular dysfunction is eliminated, the risk of sudden death is sharply reduced.
An unfavorable prognostic factor in the post-infarction period is depression of the ST interval (painless or accompanied by pain) during exercise testing. The combination of subtotal stenosis of one or more coronary arteries, areas of left ventricular dyskinesia (detected by echocardiography) and frequent polytopic ventricular extrasystoles has a poor prognostic value. The risk of sudden death is significantly increased by the presence of a left ventricular aneurysm, its pronounced hypertrophy, as well as ventricular fibrillation that occurred in the acute period of myocardial infarction and was successfully stopped.
Left ventricular myocardial dysfunction
A decrease in the contractile function of the left ventricular myocardium is one of the main risk factors for sudden cardiac death in cardiac patients. A reduction in ejection fraction of less than 40% is considered critical. After the onset of congestive heart failure of various origins, the risk of sudden cardiac death is very high, it can be 35-40% within 5 years.
Left ventricular myocardial hypertrophy
Left ventricular myocardial hypertrophy of any origin significantly predisposes to sudden cardiac death, with fatal arrhythmia being the most common mechanism of death. This is explained by the fact that with myocardial hypertrophy, the kinetics of ions in it is disrupted, there is a pronounced heterogeneity in the medium of propagation of depolarization and repolarization waves in the myocardium, which contributes to the development of ventricular fibrillation and flutter.
“Unreasonable” decrease in exercise tolerance
Usually, the basis for an unreasonable decrease in exercise tolerance is myocardial ischemia, which is also often combined with cardiac arrhythmias. These factors significantly increase the risk of sudden cardiac death.
Previous sudden cardiac death and previous resuscitation
In patients who have survived sudden cardiac death, the risk of recurrence of ventricular fibrillation is very high: up to 25% during the first year and approximately 5% during the second year (N. M. Shevchenko, 1992).
Violation of autonomic regulation of the heart
In case of coronary artery disease, inflammatory myocardial diseases, diabetes mellitus and other diseases, damage to the autonomic nervous system is observed, which causes its dysfunction and leads, in particular, to a decrease in the effects on the heart and an increase in sympathetic activity. Signs of a violation of the autonomic regulation of the heart are an increase in heart rate and a decrease in heart rate variability.
An increase in sympathetic activity significantly increases the risk of sudden cardiac death, especially in the morning, after the patient awakens. Sympathetic stimulation is also promoted by various toxic effects on the myocardium (smoking, alcohol).
REMINDER FOR THE POPULATION
Prevention of Sudden Cardiac Death
The problem of sudden cardiac death (SCD) has remained one of the pressing health problems for many years due to its medical and social significance, as well as its drama. Sudden cardiac death is understood as circulatory arrest that develops suddenly, within an hour from the onset of clinical symptoms. This outcome is unexpected both for doctors and relatives, since the patient is in a stable condition on the eve of the attack. In some people, sudden cardiac death is the first and last manifestation of the disease. What is the reason for such transience of events? Sudden cardiac death in most cases is an arrhythmic death, in which medical care should be provided within the first 5-6 minutes, and in 90% of cases, circulatory arrest during sudden cardiac death occurs outside of a hospital setting.
According to WHO, the incidence of sudden cardiac death is 30 cases per week per 1 million population. To make it easier to imagine the scale of the problem, here are the following figures: in Europe and the USA, about 350,000 people die suddenly every year (this is an entire city of regional significance!), and every 5 minutes in the world one person dies suddenly! Unfortunately, there are no accurate statistics on sudden cardiac death in our country, since such a diagnosis is not included in post-mortem reports. However, given the high morbidity and mortality from cardiovascular diseases in our country, one of the highest in Europe, there is no doubt that we are “leaders” in this matter.
Since, as indicated, resuscitation measures in case of circulatory arrest must be carried out immediately, and in real life are not always feasible, the main approach to solving the problem of sudden cardiac death is its prevention. It should primarily be carried out in individuals at high risk of sudden cardiac death. Among heart diseases, the main cause of sudden cardiac death is coronary heart disease, which accounts for up to 80% of all cases of sudden cardiac death, and especially in patients who have had a myocardial infarction.
The examination program for patients with coronary artery disease should include:
- Consultation with a cardiologist;
- ECG;
- Test with physical activity - treadmill test;
- Echocardiography;
- Daily ECG monitoring with additional options (assessment of heart rate variability, sinus rhythm turbulence, T wave alternans);
- High-resolution ECG with registration of late ventricular potentials.
Recently, the issue of the risk of sudden death in athletes has become relevant. In an analysis of 185 cases of death of athletes in the United States (1985-1995), the main cause was identified as cardiovascular pathology, with hypertrophic cardiomyopathy leading in it (36%). When analyzing medical documentation, more than a third of athletes noted fainting or pre-fainting conditions, or cardiac complaints several months before death.
It is customary to distinguish three main categories of sudden death in athletes:
- 1st: “commotio cordis” syndrome - develops in the event of a strong blow to the heart, followed by a life-threatening arrhythmia;
- 2nd: sudden death in athletes under 30 years of age is usually associated with congenital cardiac pathology (hypertrophic cardiomyopathies, WPW syndrome, Brugada syndrome, etc.);
- 3rd: sudden death in athletes after 30 years of age, when the death is caused by an already acquired pathology, for example, ischemic heart disease.
The examination program for athletes should include:
- Consultation with a cardiologist;
- ECG;
- Echocardiography;
- Test with physical activity - treadmill test;
- Daily ECG monitoring.
In recent years, the development of sudden cardiac death has been identified as a cause such as respiratory arrest during sleep (obstructive apnea syndrome). This syndrome is manifested by snoring, pauses in breathing during sleep, and daytime sleepiness. In contrast to the generally accepted fact that the peak of cardiovascular mortality in the general population occurs in the early morning hours (from 6.00 to 12.00), in patients with obstructive apnea syndrome, the highest incidence of sudden cardiovascular mortality occurs during the night period (from 00.00 to 6.00). Sleep apnea leads to the development of sinus node arrest, AV blockade of various degrees, up to complete transverse block, and also contributes to the development of arterial hypertension, diabetes mellitus, and maintains obesity (obesity is typical for persons with obstructive apnea).
The examination program for patients with obstructive apnea syndrome should include:
- Consultation with a cardiologist;
- Consultation with an otolaryngologist;
- Polysomnography;
- Consultation with an endocrinologist.
To combat this disease, special breathing devices are selected that eliminate sleep apnea and normalize sleep.
I would like to emphasize that persons with so-called risk factors for cardiovascular diseases are also at risk of premature death. These include: smoking, hypertension, high cholesterol, family history of cardiovascular pathology, obesity, diabetes, physical inactivity. These individuals are recommended to undergo examination using scales developed by European cardiologists (see figure), as well as additional tests (homocysteine, myeloperoxidase, C-reactive protein, comprehensive lipid profile, etc.) and calculate the risk of fatal complications in the next 10 years.
About holding Health Day on the topic
“Let’s prevent the risks of sudden death!”
On October 8, 2021, the State Budgetary Institution “Center for Medical Prevention” of the Ministry of Health of the Krasnodar Territory will organize the next Health Day, which is held as part of the Day for the Prevention of Sudden Death and Life-Threatening Aries. Health Day is held with the aim of preventing cardiovascular diseases and promoting the principles of a healthy lifestyle. An indicative Health Day with the participation of regional specialists will be held in the city of Krasnodar. During the Health Day, organized jointly with the city administration and with the participation of the press, diagnostic tests, consultations, lectures, propaganda and festive events will be carried out.
Cardiovascular diseases, mainly sudden cardiac death (SCD), are the leading cause of death in most countries of the world. SCD is the most pressing problem of our time. The mechanisms underlying the development of sudden cardiac death in the vast majority of cases are ventricular tachycardia (VT) and ventricular fibrillation (VF) - 95%, and the remaining 5% are due to bradyarrhythmias and asystole. The main cause of SCD is coronary heart disease.
Sudden cardiac death is one of the pressing problems of our time. Currently, many different studies are being conducted to study this problem. When treating patients with cardiovascular diseases, the main efforts of doctors should be aimed at actively preventing sudden cardiac death with the help of drugs that have maximum effectiveness and safety.
The issue of preventing sudden cardiac arrest is very important, since the correct attitude to one’s own feelings and the complaints of a loved one will in many cases prevent a fatal outcome. As a number of research works show, many people ignore the warning signals sent by their own body. Thus, very often, patients resuscitated after a sudden stop of blood circulation report previous chest pain, attacks of severe weakness, shortness of breath, palpitations and some other symptoms that appeared hours, days or even weeks before the development of the episode. Many patients with diagnosed heart disease report deterioration of their condition prior to cardiac arrest, but the appearance of these symptoms for some reason does not prompt many of them to seek medical help. And this is due, first of all, to the lack of awareness of patients about the symptoms of heart disease and its potential complications and outcomes.
Sudden cardiac death is a rather insidious disease, and it is not always possible to identify potential patients. That is why the most important thing in the fight against this condition is the timely implementation of emergency measures. Nowadays, many public places have defibrillators that can be used for life-threatening arrhythmias. They also often conduct special courses on teaching resuscitation measures to ordinary citizens.
GBUZ "Center for Medical Prevention" of the Ministry of Health of the Krasnodar Territory.
Causes
Epidemiology
. One of the leading causes of death in the adult population of developed countries is SCD due to coronary heart disease. In patients with sudden cardiovascular collapse, the rhythm of ventricular fibrillation is most often determined on the ECG (in 75-80% of cases), while bradyarrhythmias are the cause of SCD in a minimal number of patients. In 5-10% of cases of sudden cardiac death, patients do not have coronary heart disease or congestive heart failure. According to statistical data obtained annually in Western countries, the incidence of SCD varies from 0.6 – 1.28 per 1000 people per year. These studies only include data on those killed or resuscitated by emergency medical services; thus, official data are lower than the actual number of SCD cases in the general population.
Prevention of sudden cardiac death: general population and high-risk group. Among the adult population, the incidence of SCD is 1 in 1000 per year. Prophylactic interventions to reduce the risk of sudden cardiac death in this population appear to be neither practical nor cost-effective, since the costs include the remaining 999 per 1000 people per year who are not at risk for SCD. Thus, general principles of a healthy lifestyle are recommended in the general population.
Subgroups in which the annual risk of sudden cardiac death progressively increases are relatively few. It follows from this that promoting a healthy lifestyle among the population will naturally lead to a decrease in the number of patients with coronary heart disease, which in turn will reduce the number of cases of sudden cardiac death.
V. Pathology of the coronary arteries
Anomalous origin of the coronary arteries
SCD most often occurs in patients with an anomalous origin of the trunk of the left coronary artery from the right or non-coronary sinus of Valsalva. Therefore, special attention should be paid to young patients with chest pain similar in description to angina. Surgery is the most appropriate treatment option for patients at high risk of sudden cardiac death.
Anomalous origin of the coronary arteries
| Class | I | IIa | IIb |
| Risk stratification | VF | Young patients with angina or a positive stress test | |
| Primary prevention | Surgery | ||
| Secondary prevention | Surgery |
Myocardial bridges
The long-term prognosis for patients with the presence of myocardial bridges seems favorable, but in some cases this pathology can cause the development of tachyarrhythmias or sudden cardiac death. In symptomatic patients, quantitative coronary angiography, Doppler, and intravascular ultrasound are used to diagnose myocardial bridges. Drug treatment with beta blockers, surgery, angioplasty and coronary artery stenting are alternative treatments.
Myocardial bridges
| Class | I | IIa | IIb |
| Risk stratification | Symptomatic VT VF | Myocardial ischemia | |
| Primary prevention | Surgical treatment in patients with myocardial ischemia | Beta blockers | |
| Secondary prevention | Surgical treatment in patients with myocardial ischemia |
Prevention of SCD: recommendations of the European Society of Cardiology
The European Society of Cardiology Specialist Group on Sudden Cardiac Death presents recommendations aimed at reducing the incidence of SCD. The recommendations are presented in tables and distributed as follows:
Class I:
Reliable evidence and/or consensus among experts that a given procedure or treatment is appropriate, beneficial and effective.
Class II:
Conflicting evidence and/or differences in expert opinion about the benefit/effectiveness of a procedure or treatment.
Class IIa:
evidence and/or expert opinion for benefit/effectiveness predominates.
Class IIb
: Benefit/effectiveness is not well supported by evidence and/or expert opinion.
In these guidelines, the terms “primary” and “secondary” prevention are used primarily in the context of ventricular arrhythmia. Therapy prescribed to prevent the development of sustained ventricular arrhythmias in patients without a history of episodes of life-threatening ventricular arrhythmias, but classified as at high risk for their development, refers to “primary” prevention. The therapy recommended for patients with cardiac arrest and syncope/hypotension secondary to paroxysmal ventricular tachycardia is “secondary” prevention.
VI. Wolff-Parkinson-White syndrome (WPW)
According to modern research, in patients with WPW syndrome, the incidence of sudden cardiac death is 0.15% per year. The main cause of SCD is the transition of atrial fibrillation with a rapid ventricular response to ventricular fibrillation. Survivors of resuscitation for sudden cardiac death are typically characterized by the absence of symptoms, shortened RR intervals (less than 250 ms) during paroxysmal atrial fibrillation, and the presence of multiple or posteroseptal accessory pathways. Electrophysiological study with atrial excitation and determination of RR intervals between preexcited QRS complexes has high sensitivity, but specificity and significance in determining a positive predictor are limited. In patients at high risk for SCD, catheter ablation is recommended, particularly in those resuscitated from ventricular fibrillation or in patients with symptomatic episodes of atrial fibrillation with a rapid ventricular response.
Wolff-Parkinson-White syndrome
| Class | I | IIa | IIb |
| Risk stratification | less than 250 ms cycle duration in AF less than 270 ms anterograde refractory period of additional pathways Multiple additional pathways | Cessation of pre-excitation during treatment with ajmaline | |
| Primary prevention | Ablation for atrial fibrillation and the presence of rapid conduction through accessory pathways | Ablation in asymptomatic patients with – family history of SCD – athletes | Amiodarone Antiarrhythmic drugs classes Ia and Ic |
| Secondary prevention | Ablation |
VII. Bradyarrhythmias
It has been established that bradyarrhythmias are the cause of sudden cardiac death in 15-20% of cases. Risk factors for bradyarrhythmic death include high-degree AV block with intraventricular conduction disturbances, but in the presence of structural changes in the heart, these factors may predispose to the development of tachyarrhythmias. Pacing is the treatment of choice in high-risk patients with bradyarrhythmia: it relieves symptoms and may reduce mortality.
Risk stratification for cardiac conduction disorders
| Class | I | IIa | IIb |
| Profound AV block | AV block III degree AV block II degree, type II Syncope Combination of heart disease with CHF | ||
| Congenital AV block of the third degree | Syncope QT prolongation Congenital heart disease | ||
| Chronic two- or three-fascicle blockade | Combination of heart disease with CHF | Syncope Conduction from the Hiss bundle to the ventricles 100 ms (HV interval 100 ms) Intraventricular blocks Blocks induced during EPI |
III. Genetic pathology of ion channels
QT prolongation
Long QT syndrome is associated with a high risk of sudden cardiac death. Risk stratification is mainly based on the presence of syncope, Torsades de Pointe (VT) and a history of cardiac arrest. Primary prevention of SCD is generally based on treatment with beta blockers. CD implantation is recommended for secondary prevention, as well as in patients with VT/VF with a history of adequate treatment with beta blockers.
QT prolongation
| Class | I | IIa | IIb |
| Risk stratification | Torsade de pointes/VF/cardiac arrest Syncope Jervell–Lange-Nielsen syndrome QT prolongation | QT greater than 600 ms Development of VT/VF in childhood Prolongation of QT + AV block Macroscopically dynamic T waves Female gender Postpartum period | Family history of SCD Increased QT interval dispersion |
| Primary prevention | Avoid drugs that prolong the QT interval Beta blockers Avoid strenuous exercise | Sympathetic denervation of the LV pacemaker | |
| Secondary prevention | KD + beta blockers + avoid drugs that prolong the QT interval Avoid intense exercise |
ECS - electrical pacemaker
Brugada syndrome
Diagnosis of Brugada syndrome (BS) is based on the presence of spontaneous or inducible ST segment elevation in leads V1-V with or without right bundle branch block (RBBB). Risk stratification is still poorly defined, and the role of EPS in identifying patients with high-risk factors is debated. In survivors of cardiac arrest, CD implantation is recommended. Prophylactic use of KD in high-risk populations is strongly recommended, but this approach is limited by the lack of clearly defined risk criteria.
Brugada syndrome
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Syncope Family history of SCD | Inducible VT/VF during EPI |
| Primary prevention | CD in patients with syncope/VT | KD in asymptomatic patients with VT induced by EPI | |
| Secondary prevention | KD |
Catecholaminergic polymorphic ventricular tachycardia
To date, there is no precise definition of catecholaminergic polymorphic ventricular tachycardia (CPVT), since large-scale studies are not possible. This disease is associated with a high risk of sudden cardiac death at a young age, but criteria for stratification are lacking. Prevention of sudden cardiac death is based on the use of beta blockers; KDs are recommended for secondary prevention, since the significance of KDs for primary prevention has not been determined.
Catecholaminergic polymorphic ventricular tachycardia
| Class | I | IIa | IIb |
| Risk stratification | VF | Family history of SCD Unsustained VT/syncope in childhood | Syncopations |
| Primary prevention | Beta blockers | KD | |
| Secondary prevention | KD + beta blockers | Beta blockers |
IV. Valve pathology
Aortic stenosis
Among patients whose cause of death is aortic stenosis (AS), about 20% are sudden cardiac death. In the absence of symptoms, the survival rate of patients with AS is high even without valve replacement. The prognostic value of various hemodynamic and electrophysiological studies is limited. Asymptomatic patients with hemodynamically severe aortic stenosis should be under constant observation and, if symptoms develop, undergo immediate surgery. In patients with documented sustained ventricular tachycardia, cardiac implantation should be considered.
Aortic stenosis
| Class | I | IIa | IIb |
| Risk stratification | Syncope Angina | VT, including those induced by EPS Decreased exercise tolerance | Significant stenosis |
| Primary prevention | Surgery | Amiodarone | |
| Secondary prevention | KD |
Mitral valve prolapse
Mitral valve prolapse (MVP) generally has a favorable prognosis; There are suggestions about the risk of sudden cardiac death, but there is no evidence. Most cases of SCD are described in patients who have previously suffered syncope or cardiac arrest, a family history of SCD at a young age, with severe prolapse or myxomatous changes in the mitral valve leaflets. For patients surviving cardiac arrest, CD implantation is recommended.
Mitral valve prolapse
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Family history of SCD Severe prolapse or myxomatous changes in the leaflets | QT prolongation Frequent/group ES Inducible VT/VF with EPS Mitral valve regurgitation Late potentials |
| Primary prevention | |||
| Secondary prevention | KD |
Disease clinic
I would like to draw special attention to the fact that the death of a patient due to cardiac failure is not actually “sudden”. There are symptoms that begin several days or even weeks before sudden death.
Harbingers
In the vast majority of cases, warning signs are noted a couple of weeks before death. According to statistical studies, 75% of people experience certain symptoms. But many do not pay attention to them, considering them as temporary and transitory deterioration. It could be:
- fatigue when performing usual activities;
- transient rhythm disturbances of various types, most often with an increase in the frequency of contractions;
- constant unmotivated weakness;
- fainting;
- shortness of breath with slight exertion or at rest.
Along the left ventricle
Signs also indicate a type of deficiency. If the function of the left ventricle is impaired, the movement of blood in the pulmonary circle worsens, simulating pulmonary pathology. In this case, the following deviations are observed:
- severe lack of air with attacks of suffocation (cardiac asthma);
- pale skin;
- tachycardia;
- painful cough with pink, foamy sputum;
- moist coarse rales in the lungs, which are sometimes heard without the use of a stethoscope.
Right ventricle
If the functioning of the right ventricle is impaired (a problem with the systemic circulation), the symptoms are as follows:
- severe sweating;
- blue color of the nasolabial triangle;
- visible swelling of the veins in the neck;
- shortness of breath, turning into suffocation;
- decreased blood pressure;
- weak pulse that is difficult to palpate;
- enlarged liver and bursting pain in the hypochondrium on the right;
- swelling of the distal legs;
- leakage of fluid into the abdominal cavity (ascites).
Any type of heart failure gradually turns into total or mixed. In this case, general symptoms will be observed. And the likelihood of sudden death will increase many times.
Signs before death
For a dying person with cardiopathy, there are a number of signs and symptoms:
- sharp pain behind the sternum;
- significant increase in heart rate;
- rhythm disturbance (ventricular fibrillation or tachycardia);
- loss of consciousness;
- tonic convulsions;
- a special type of breathing (Cheyne-Stokes) - frequent and deep, then slow and convulsive;
- the heart stops working;
- the skin becomes gray;
- pupils dilate.
Death during sleep from heart failure occurs as a result of increased blood flow to the myocardium, which increases the load on it. In the presence of cardiac pathology, this can sometimes cause the development of arrhythmia or re-infarction with a fatal outcome.
Out-of-hospital resuscitation
Survival after cardiac arrest varies from 5% to 60% depending on the characteristics of the cardiac arrest (ie, cardiac etiology or not; verified or not; ventricular fibrillation or not). The outcome of cardiopulmonary resuscitation (CPR) is influenced not only by the success of its implementation, but also by the patient’s condition before the start of CPR.
It is now generally accepted that time to electrical defibrillation is the single most significant determinant of survival after cardiac arrest.
The instructions for the automatic external defibrillator allow defibrillation in cases of out-of-hospital ventricular fibrillation or ventricular tachycardia to people of non-medical professions, often many minutes before the arrival of the ambulance team. This strategy is known in the West as “first responder defibrillation,” based on the principle of mutual aid.