Accelerated metabolism and increased oxygen demands cause children's hearts to beat faster. Heart rate norms are individual for each age. If for some reason this indicator exceeds the norm for no apparent reason (emotional experiences or physical exertion, overheating), tachycardia is diagnosed. At the medical center (Moscow, Otradnoye metro station, North-East Administrative District), cardiologists diagnose and treat tachycardia in children. Therapy begins with eliminating the root cause, and along the way, doctors select medications that alleviate the condition.
Causes and types
Restlessness is considered one of the causes of cardiac tachycardia in childhood. Children are constantly moving, which naturally causes an increase in heart rate and heart rate. Other factors are also possible:
- dehydration;
- heart murmurs;
- anemia;
- cardiopathy;
- thyrotoxicosis;
- Congenital heart defect.
In addition, there are two forms of the disease: sinus and paroxysmal, which also develop for certain reasons. Sinus tachycardia in children is a consequence of:
- accelerated growth;
- stress;
- disorders of the endocrine or cardiovascular systems;
- overwork.
Diagnosing the cause of the paroxysmal form is more difficult, since in this case the heart rate increases and slows down suddenly. Seizures occur at any age, including in newborns.
Features of pediatric sinus tachycardia
Content
Sinus tachycardia in children is when the heart beats too fast when there is an acceptable sinus rhythm. A sign of it is a pulse of more than 100 beats per minute for adults. In children, the bar above which the heart rate is considered abnormal depends on age. The older the child, the lower the threshold beyond which pathology is determined.
Causes of this disease
The causes of heart palpitations are slightly different in infants and adolescents. If we talk about newborns, their heart rate increases greatly due to the fact that the automaticity of the sinus node is increased. The specific reasons are as follows:
- physiological reasons: overheating, swaddling, pain, anxiety, examination;
- pathology;
- myocarditis;
- hypoglycemia;
- damage to the central nervous system.
This syndrome is a benign condition in newborns.
If a baby has sinus tachycardia for a long period of time, myocardial metabolism may be disrupted. However, most often for newborns, the syndrome we are discussing is a benign condition. The reasons why sinus tachycardia occurs in adolescents are somewhat different:
- age-related characteristics, for example, strong growth of the body;
- emotional stress;
- diseases, endocrine, cardiovascular and so on;
- physical stress.
Types and symptoms
Sinus tachycardia can be of three types:
- Moderate, in which the heart rate increases by no more than 20 percent;
- Average, characterized by an increase in rhythm by no more than 40 percent;
- Pronounced – increase in rhythm up to 60 percent.
Symptoms of tachycardia are as follows:
- palpable episodes of increased heart rate;
- pain in the heart area;
- weakness;
- dizziness;
- dyspnea:
- fainting;
- fast fatiguability.
Diagnosis and treatment
Diagnostics includes a number of methods.
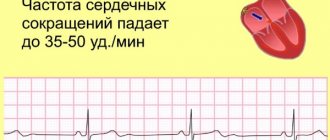
- ECG. Using it, it is easy to determine the frequency and rhythm of heart contractions in both infants and adolescents.
A nurse performs an ECG
- Daily ECG monitoring. The method is informative and safe for both infants and adolescents.
- Echo CG is performed to determine sinus pathology that can affect the heart.
- Electrophysiological study of the heart. Allows you to find out the mechanism of tachycardia and cardiac conduction disturbances.
- General blood analysis
- Determination of thyroid-stimulating hormones in the blood.
- EEG of the brain. It is with the help of this study that blood disease and central nervous system pathology can be excluded.
- Open access to fresh air into the room; it is better to go outside by loosening the collar of your shirt or sweater. The neck should be free.
- Place a cold, wet towel or handkerchief on your forehead.
If you witness an attack of tachycardia in a child, you must:
Treatment can only be prescribed by a doctor
If this does not bring relief, be sure to call a doctor. In most cases, the disease goes away on its own. The increased heart rate resulting from high temperature returns to normal after it decreases. Treatment of childhood tachycardia by doctors involves taking sedatives based on medicinal herbs. Only a cardiologist, knowing the medical history, can select individual treatment methods that are suitable for each patient. They are based on certain principles.
- In case of sinus disease of a neurogenic nature, you need to consult a neurologist, who will certainly prescribe his own treatment.
- It is worth distinguishing between reflex tachycardia (with hypovolemia) and compensatory tachycardia (anemia, iron deficiency). To do this, it is necessary to eliminate the causes of sinus disease.
- If a patient has endocrine disorders, they can be eliminated by an endocrinologist, to whom the patient goes for a consultation.
- If tachycardia is associated with cardiac dysfunction, the cardiologist prescribes cardiac glycosides.
Prevention
Preventive measures include three main principles.
- Early diagnosis. The earlier this disease is detected, the sooner a treatment method will be prescribed.
Symptoms
In addition to palpitations, cardiac tachycardia in children manifests itself:
- chest pain;
- shortness of breath;
- dizziness and fainting;
- lethargy and pallor;
- nausea;
- sweating
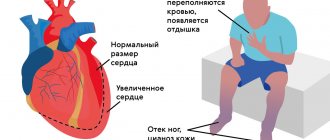
At such moments, infants become restless and capricious, refusing to eat and sleep. It is important to consult a doctor as soon as you notice the first signs of illness. If tachycardia in children is not treated, the severe pathologies that caused it will lead to serious complications:
- arrhythmogenic shock;
- pulmonary edema;
- heart failure;
- cardiac arrest.
Sinus tachycardia
The causes of sinus tachycardia in adolescents may be neurogenic effects, organic heart damage, or increased thyroid function. An increase in heart rate is said to occur if it becomes more than 80 beats per minute.
The occurrence of neurogenic sinus tachycardia is also based on an imbalance in the autonomic nervous system, expressed in the increased effect of sympathetic innervation on the Kate-Fleck sinus node. In this case, the heart rate can increase to 100-120 beats per minute. Characteristic features of this form of tachycardia are its variability, periodic transition to a normal rhythm, and greater rhythm lability in response to exogenous influences, mainly neuropsychic.
The increase in rhythm is especially pronounced in a standing position, therefore the ortho-clinostatic test for this form of tachycardia is positive, the body temperature is normal, and the general state of health is satisfactory. The diagnosis of neurogenic sinus tachycardia should be approached in a strictly differentiated manner. It is necessary to exclude damage to the cardiovascular system.
Thus, the causes of tachycardia can be acquired and congenital heart defects, of which tachycardia is especially often observed with an open ductus arteriosus, atrial septal defect, etc.
Sinus tachycardia can occur with a small heart; in this case, a decrease in stroke volume causes a compensatory increase in rhythm. Making a diagnosis in all of the above cases does not cause any particular difficulties. It can be more difficult to exclude thyrotoxicosis, especially if thyroid function during testing turns out to be normal, despite its slight increase and the presence of other mild signs of thyrotoxicosis.
In this case, it is necessary to resort to treatment with microdoses of iodine, sometimes ex uvantibus, in order to come to a final conclusion.
“Clinic of diseases, physiology and hygiene in adolescence”, G.N. Serdyukovskaya
Tachycardia
Diagnostics
The task of a cardiologist who examines a child with suspected tachycardia is to make sure that the signs he has do not indicate other diseases, for example, bronchial asthma. Also during the examination, he looks for the cause of the disease. To do this, the specialist uses:
- ECG and daily monitoring to analyze how the heart rhythm changes during the normal activity of a small patient;
- EchoCG and MRI to make sure there are no heart pathologies;
- an electrophysiological study to check how the electrical impulse travels through the heart muscle;
- laboratory methods: urine, blood analysis;
- EEG of the brain to make sure that the activity of the central nervous system is not impaired.
Treatment and prognosis
In case of sudden attacks of tachycardia, the child should be taken out into the fresh air, tight clothes should be removed, a damp handkerchief should be placed on the forehead, and then a doctor should be called. If there is no pathology, and hormonal changes and stress lead to an acceleration of the heart rate, to treat tachycardia in children, the cardiologist will prescribe drug therapy (beta-blockers, cardiac glycosides, calcium antagonists, sedatives). Auxiliary measures: physical therapy, valgus techniques. To alleviate the condition, a diet is recommended in which it is undesirable to consume chocolate, tea, spicy, and salty foods.
Children who follow the doctor's recommendations usually return to their previous lives and activities. In rare cases, when the disease develops due to other serious pathologies that cannot be treated conservatively, surgery is prescribed.
Paroxysmal tachycardia in children
Supraventricular tachycardia
Perform sequential reflex activities that stimulate the vagus nerve.
If the child is over 3-4 years old, carry out:
- massage in the area of the carotid artery lasting 5-10 seconds on the right, then on the left
- Valsalva maneuver (consists in the fact that the child closes his nose and strains for 10 seconds)
For children over 7 years old, additional diagnostic methods are used:
- slow, deep swallowing
- pressing on the root of the tongue with a spatula
- wiping with cold water
It is highly not recommended to use the Aschner test, because retinal detachment may occur.
Sedatives are used for treatment:
- valerian
- valocardine
- corvalol
It is also necessary to take asparkam. The dose, depending on the age of the child, is from 1/3 to 1 tablet.
If the above treatment does not bring results, antiarrhythmic drugs are used. Self-medication is contraindicated, since the intake is sequential - it is determined by the doctor. Verapamil 0.25% is administered intravenously, monitoring blood pressure and heart rate. The dose for children under 12 months is from 0.4 to 0.8 ml, for children from 1 to 5 years old - from 0.8 to 1.2 ml, for patients aged 11 to 15 years - 1.5-2 .0 ml.
Verapamil should not be taken together with beta-blockers and quinidine. Contraindications for taking the drug are the supraventricular form of paroxysmal tachycardia with aberrant ventricular complexes, WPW syndrome.
A 1% ATP solution is quickly injected intravenously, the dose is 0.5-1 ml for preschool children and 1 ml for children over 7 years old. Ajmaline (gilurythmal) 2.5% is slowly administered intravenously per 10.0-20.0 ml of 0.9% NaCl solution at a dose of 1 mg/kg.
Digoxin 0.025% is administered intravenously or intramuscularly. The saturation dose is 0.03-0.05 mg/kg. Saturation rate – 3 days. The maintenance dose is 1/5 - 1/6 of the saturation dose.
If the therapy does not produce results, Amiodarone 5% solution is administered intravenously very slowly at 10.0-20.0 ml of 5% glucose solution at a dose of 5 mg/kg. If there is no effect, transesophageal pacing or electrical pulse therapy is performed.
Ventricular tachycardia
For a child with this form of paroxysmal tachycardia, a gentle regime is introduced, physical activity should be limited, and sufficient sleep. It is important to systematically walk in the fresh air. During an attack, stay in bed. You can't play sports. The diet should contain potassium and magnesium, vitamins. Potassium and magnesium are found in dried apricots, raisins, dried fruits, and baked potatoes. You cannot drink coffee or tea or eat chocolate.
Relieving an attack of ventricular tachycardia:
1. 1-1.5 mg/kg lidocaine 1% is slowly administered intravenously. If there is no effect, I repeat the injection with a 2-fold smaller dose after 5-10 minutes.
2. If there is no effect, a 2.5% solution of ajmaline (gilurhythmal) is slowly injected intravenously into 10.0-20.0 ml of a 0.9% NaCl solution at a dose of 1 mg/kg.
3. If no effect is observed, a 5% amiodarone solution is administered intravenously - very slowly with 10.0-20.0 ml of a 5% glucose solution at a dose of 5 mg/kg.
4. If no effect is observed, transesophageal pacing or electrical pulse therapy is performed.