Kawasaki disease - what is it? Symptoms and treatment
Kawasaki disease (Kawasaki syndrome, mucocutaneous lymphatic syndrome) belongs to a group of diseases called systemic vasculitis. Diseases in this group cause abnormal damage by cells of the immune system to blood vessels, most often medium- and small-sized arteries and veins. In the case of Kawasaki syndrome, it can cause damage to children's coronary arteries - the vessels that carry oxygen-rich blood and nutrients to the heart.
In addition to the coronary arteries, the inflammatory process can affect the pericardium, which surrounds the heart, as well as endocardial tissue (the inside of the heart), and even the heart muscle itself.
Kawasaki disease most often affects children, usually under 5 years of age. Older children and adults are rarely exposed to it. The peak incidence occurs between the ages of 1 and 2 years, and boys are more often affected.
Causes
Currently, rheumatology does not have clear data on the causes of Kawasaki disease.
The most accepted theory is the assumption that Kawasaki disease develops against the background of a hereditary predisposition under the influence of infectious agents of a bacterial (streptococcus, staphylococcus, rickettsia) or viral (Epstein-Barr virus, herpes simplex, parvoviruses, retroviruses) nature.
A hereditary predisposition to Kawasaki disease is supported by the connection of the disease with race, its spread in other countries mainly among Japanese emigrants, and the development of the disease in 8-9% of the descendants of those who have recovered from the disease.
Introduction
Kawasaki syndrome (KS), or mucocutaneous lymphonodular syndrome, is an acute systemic disease with predominant damage to medium and small arteries and the development of destructive-proliferative vasculitis.
Clinically, KS occurs with fever, changes in the mucous membranes, skin, lymph nodes, and possible damage to the coronary and other visceral arteries [1]. This disease was first described by T. Kawasaki in Japan in 1967. Since 1961, he observed children with prolonged fever and symptoms such as cervical lymphadenitis, conjunctivitis, rash, swelling of the hands and feet, followed by peeling of the fingers. This symptom complex did not fit any known disease. T. Kawasaki described about 50 cases, then this condition was called “febrile oculo-cutaneoacrodesquamative syndrome with non-purulent cervical lymphadenitis.” And in 1992, the disease as an independent nosological unit was identified in the most important reference book for American pediatricians, the Nelson Textbook, and received the name of its discoverer - Kawasaki syndrome. In Russia, a detailed monograph by G.A. is devoted to the UK. Lyskina, O.G. Shirinskaya [2], however, a number of issues require additional coverage.
This work is presented with the aim of summarizing our own experience in the diagnosis and treatment of KS in the light of available literature data.
In the department of diagnostics and rehabilitation treatment of the National Center for Children's Health, we observed 22 children with KS. Of these, one was 12 years old, the age of the other children ranged from 2.5 to 36.0 months (average age - 12 months). The ratio of boys to girls was 1.0:1.2. In case of an unclear diagnosis, children with prolonged fever, in addition to the standard set of examinations for fever without a focus of infection, underwent ultrasound examination of the heart and coronary vessels. If KS was confirmed, cardiac ultrasound was performed again after the 10th day of illness.
Epidemiology and pathogenesis
Most often, KS is registered in Japan, reaching a level of 112–239 cases per year per 100 thousand children under 5 years of age [3, 4]. In total, more than 170 thousand cases of KS have been reported in Japan since 1960 [5]. In the USA, up to 3000 new cases of KS per 100 thousand children under 5 years of age are described annually; the frequency is 20.8 (range - from 18.5 to 23.1 in different years) [5, 6]. This age group accounted for 76.8% of all KS cases; the ratio of boys to girls was about 3:2 [6].
Over a 15-year observation period in the Irkutsk region, the average incidence rate of KS was only 6.6 cases per 100 thousand children under 5 years of age and 2.7 per 100 thousand children under 17 years of age. Thus, patients under 5 years of age accounted for 67.5% of cases, of which 50.8% were under 3 years of age. KS is most severely suffered by infants; in Russia their share is 23.5% [7].
In contrast to the 7-year observation data in the Russian Federation (3 seasonal increases in incidence: December–January [20.5%], March–April [21.6%], October [11.4%] and 3 months of decline – August, September, November [8]), in our observations, 55% of children fell ill in the spring months - (March - 5 children, April - 3, May - 3) and 25% in the winter (5 children - in January and February).
There is no clear opinion regarding the cause of the development of KS.
General inflammatory symptoms, increased levels of inflammatory markers, seasonality and epidemic outbreaks speak in favor of an infectious nature. In this regard, the Epstein–Barr virus, retro- and parvoviruses, strepto- and staphylococci, as well as toxins were considered. The fact that KS is rare in children under 4 months of age may indicate passive maternal immunity, while the extremely rare occurrence in adults may reflect acquired immunity. The geographic sequence of the increase in incidence (Asia–Japan–Hawaii–West Coast of the USA) can be explained by the spread of the KS pathogen under the influence of atmospheric phenomena. Local outbreaks may also be associated with the circulation of an infectious agent [9]. But so far it has not been possible to confirm or refute the infectious hypothesis [2, 8].
The immune response also plays a role in the pathogenesis of KS: polyclonal activation of lymphocytes, increased levels of circulating T-helper cells, monocytes and macrophages, deposition of immune complexes in affected tissues. There is also a widespread belief that the disease develops only in genetically predisposed individuals [7, 10].
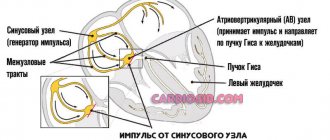
In KS, medium and small caliber arteries are affected; the involvement of the coronary arteries (CA) in the process is of particular importance - up to 20% of cases. At autopsy, edema of endothelial and smooth muscle cells with inflammatory infiltration of all three layers of the vascular wall is revealed in the coronary artery, which leads to fragmentation of the internal elastic membrane with the formation of aneurysms. Neutrophils in the infiltrates quickly give way to macrophages, lymphocytes (mainly CD8 cells) and plasma cells, which in turn produce immunoglobulin A. Fibrosis with pronounced proliferation of the vessel intima at the healing stage eventually leads to stenosis or complete occlusion of its lumen [4] .
Clinical manifestations and diagnosis
The clinical picture of KS is conventionally divided into three stages. The acute febrile stage lasts 1–2 weeks, and without proper treatment – up to 3–4 weeks, which increases the risk of coronary artery disease [10]. It is characterized by persistent febrile fever lasting more than 5 days, but most often in the absence of treatment - 2-3 weeks. Damage to the mucous membranes is usually (in 95% of cases) represented by non-purulent conjunctivitis with pronounced injection of conjunctival vessels (mostly bulbar - episcleritis) (Fig. 1). Cheilitis, changes in the mucous membrane of the mouth and tongue (“crimson” tongue), and cracked lips, which we observed in 15 (75%) children, are also common (Fig. 2). Skin lesions are accompanied by the appearance of a rash, usually on the torso, limbs, and groin area. Exanthema, sometimes confluent, is most often represented by papules and macules, although urticarial and micropustular elements are also found. Bullae and vesicles have never been described. We observed a rash in 90% of patients, not always profuse, sometimes ephemeral; in all cases, the rash appeared on days 2–6 of the disease and faded after 2–4 days (Fig. 3).
We recorded enlargement (unilateral) of the anterior cervical lymph nodes in half of the cases; in two children it had a mask of purulent lymphadenitis with local hyperemia of the skin and fluctuation. These children, however, did not undergo puncture, because the presence of other signs of KS made it possible to prescribe intravenous immunoglobulin (IVIG), after which, along with the fever, changes in the lymph nodes disappeared within 24 hours. In the first days of the disease, we observed the characteristic pastiness of the hands and, more often, the feet (Fig. 4) in 12 patients; in 7 children, pain during movements in the joints and hyperemia of the skin over them were detected. These symptoms were also relieved by IVIg administration.
KS is characterized by irritability of the patient; the child is usually whiny and inconsolable, which can also be a sign of aseptic meningitis (lymphocytic pleocytosis is detected in the cerebrospinal fluid up to 25-100 in 1 μl with normal levels of glucose and protein). A characteristic clinical sign in young children is redness and hardening of the BCG injection site (in patients with KS there is cross-reactivity between heat shock proteins and T cells).
The subacute stage covers the 3rd to 5th weeks of the disease and is characterized by peeling of the skin, which begins in the fingers and toes, as well as in the groin, often accompanied by ongoing fever. Large-plate peeling from the end of the 2nd week of illness was observed by us in 11 (50%) children, just as often - pronounced peeling of the red border of the lips. 1–2 weeks after the fever subsided, transverse deep lines on the nails (Bo's lines) were detected in a number of children. Recovery, as a rule, occurs 6–10 weeks from the onset of the disease, all clinical symptoms resolve, and ESR gradually normalizes.
Changes in the heart usually manifest themselves in the form of arrhythmias, heart murmurs (“machine” noise) caused by regurgitation. Echographic signs of coronaritis with thickening of the walls or expansion of the lumen of the coronary artery, as well as ST-T changes of the ischemic type on the ECG are recorded in more than half of the patients; A quarter of patients who did not receive treatment in the acute period of KS show signs of a previous myocardial infarction [11]. It is believed that the formation of coronary artery aneurysms occurs on the 7th–9th day of illness, which is directly related to the destruction of their elastic framework. Aneurysms in patients who underwent KS are found not only in the coronary artery, but in 2.2% of patients in the axillary, common and internal iliac, renal, subclavian, superior mesenteric, internal thoracic, and femoral arteries [12]. We identified signs of coronaritis, such as thickening of the walls and dilatation of the coronary artery, in 13 (65%) patients. In 3 out of 4 children - during hospitalization after the 10th day of illness. In one 4-month-old child, hospitalized on the 31st day of fever, dilation of the left and right coronary artery was detected up to 4.5 mm. When IVIg was prescribed, positive dynamics were noted, and within 6 months the echographic picture returned to normal.
Without treatment in the acute period, signs of heart failure and myocardial ischemia are often recorded. According to Russian authors, heart failure develops in 56.3% of cases (50% – functional classes I–II, 6.3% – III–IV). Myocardial dysfunction in the same study was significantly more common in patients with coronary artery dilatation than without it – 78.3 and 43.8%, respectively [18]. Giant coronary aneurysms (with an internal diameter greater than 8 mm) are rare but carry a risk of cardiac tamponade, thrombosis, or myocardial infarction.
Often at the onset of KS, tonsillitis, symptoms of pneumonia, gastroenterocolitis, damage to the liver, urinary, and central nervous systems are detected. In these cases, especially with an incomplete picture of KS, the fever is naturally initially attributed to a bacterial infection; but maintaining a temperature after prescribing an antibiotic casts doubt on the diagnosis and can delay the diagnosis of KS by no more than 2–3 days.
Orchitis, pulmonary infiltrates, pleural effusion, hemophagocytic syndrome [13–15], as well as transient sensorineural hearing loss [16, 17] are considered rare manifestations of the disease. An example of a complex diagnostic situation is the case we encountered in a child who was admitted to the department on the 3rd day of fever with leukocyturia, an increase in the size of one kidney, leukocytosis and an increase in the level of markers of bacterial inflammation. The persistence of fever on the 3rd day of therapy with ceftriaxone, then meropenem, as well as the appearance of a generalized rash (initially regarded as allergic), an increase in the severity of scleritis, cheilitis and pasty feet from the 5th day of illness made us suspect KS. The fever stopped after administration of IVIg at a dose of 2 g/kg during the 6th–7th day of the disease; on the same day, all other symptoms began to regress and large-plate peeling of the fingers appeared.
In two more children hospitalized before the 10th day of illness, the diagnosis of KS competed with a suspicion of severe bacterial infection with increased inflammatory markers.
In one of them, the presence of watery diarrhea tilted the diagnosis in favor of a bacterial intestinal infection, and in the second, in the absence of a focus of infection, in favor of bacteremia. These suspicions seemed to be confirmed by a decrease in temperature after 36–48 hours of antibiotic therapy, but a new increase in temperature a day later with increased symptoms of KS became the reason for the introduction of IVIg, which gave a quick effect.
Laboratory studies in the acute period usually reveal acute inflammatory changes - neutrophilic leukocytosis, increased ESR, high levels of C-reactive protein, as well as normochromic normocytic anemia, but none of these tests are pathognomonic for KS. Laboratory parameters usually return to normal within 6–8 weeks. The dynamics of procalcitonin levels are somewhat different: in the first days of the disease its level is high (3 or more ng/ml), but by the second week it usually returns to normal. The platelet level increases already in the 1st week of the disease, increases significantly in the 2nd week, reaches a peak in the 3rd week and gradually normalizes in the 6–10th week of the disease. Other changes in the hemostatic system are also detected, in particular platelet hyperaggregation, depletion of the fibrinolytic system, as well as physiological anticoagulants [18], which makes it necessary to introduce them into therapy.
Predictors of severe KS that increase the risk of cardiogenic complications are increased levels of transaminases, total bilirubin, decreased levels of albumin and serum sodium. In 67% of patients, gammaglutamyl transpeptidase increases [19]. Clinical urine analysis reveals sterile pyuria and proteinuria in about a third of cases. An analysis of 1000 protein molecules showed that about 190 of them can be found in the urine of children with KS. Two proteins associated with endothelial and muscle cell damage, filamin C and the immunoregulator meprin A, were identified to be significantly elevated in patients who did not respond to initial therapy compared with patients who became afebrile after the first dose of IVIG. These indicators can be regarded as markers of disease activity, and an increase in their level in children with an incomplete form of KS can theoretically become an additional criterion for making a diagnosis [20].
One of the problems with the reliability of the diagnosis is the following: manifestations of KS can occur sequentially - so that early symptoms, for example, conjunctivitis, rash, which disappeared before hospitalization, will not be registered by the doctor. And the most frequently detected symptom, peeling of the skin, is detected in the subacute stage, when cardiac complications may already occur. Taking into account the nonspecific clinical signs of KS, differential diagnosis must be made with a number of diseases. These include streptococcal and staphylococcal infections, yersiniosis, measles, toxic shock, allergic reactions, juvenile rheumatoid arthritis, rocky mountain spotted fever, leptospirosis, urinary tract infection, etc. However, a significant increase in the risk of severe complications, including coronary artery disease, in the absence of onset treatment before the 10th day of illness dictates the need for the fastest possible diagnosis of KS.
Due to the lack of specific diagnostic markers, the American Academy of Pediatrics developed the most convenient diagnostic criteria, which made it possible to correctly interpret MC in 98% of cases [10].
In addition to unexplained fever for 5 or more days, these include at least 4 of the following 5 signs of classic KS:
- hyperemia, swelling of the hands and feet;
- polymorphic exanthema;
- bilateral injection of conjunctival vessels without discharge;
- changes in the lips and oral mucosa (hyperemia, peeling, “crimson tongue”);
- enlarged cervical lymph nodes >1.5 cm, usually unilateral.
Usually these signs are not present at the same time and the child must be observed for some period to make an accurate diagnosis.
In some patients, the clinical picture is incomplete. In the presence of an unclear 5-day fever and 2-3 of these symptoms, it is possible to make a diagnosis of “incomplete” (or atypical) KS. In our observations, the diagnosis of KS was established on the first day of hospitalization in 70% of children admitted before the 10th day. For all children hospitalized after the 10th day of illness, the diagnosis was also beyond doubt.
Incomplete KS was diagnosed in 5 children (25%) in the following cases:
- a 3-month-old girl with fever for 9 days attracted attention with hyperemia of the skin over all interphalangeal and, to a lesser extent, over the metatarsal joints with controversial swelling of the palms and feet and subtle scleritis. The diagnosis was made after identifying signs of coronaritis during cardiac ultrasound. A dose of IVIG of 2 g/kg had no effect; after the infusion, dilation of the right coronary artery was recorded to 3.5 mm. After the second dose of IVIG, the fever stopped, the diameter of the right coronary artery decreased to 2.4 mm;
- in a 12-month-old girl, on the 8th day of fever, only 2 out of 5 signs occurred: swelling of the hands with hyperemia of the skin over the interphalangeal joints and pronounced scleritis without signs of coronaritis. When IVIG was administered at a dose of 2 g/kg, the fever stopped on the first day;
- The diagnosis was difficult for a 5-month-old girl with a family history of periodic illness and a carrier of a mutation of the same gene. She was admitted on day 32 with fever; after careful questioning, the mother was able to find out only about moderate conjunctivitis and mild swelling of the hands at the beginning of the disease; The detection on ultrasound of the expansion of the left coronary artery to 3.4 and the right coronary artery to 3.2 mm decided the diagnosis. Administration of IVIG at a dose of 4 g/kg led to apyrexia on the 3rd day, followed by a decrease in the diameter of the coronary artery to 2.6 mm;
- A 22-month-old boy was admitted on the 18th day of fever with a history of scleritis and rash. His diagnosis was also confirmed by the detection of expansion of the right coronary artery to 5.5 mm with thickening of the walls. 4 g/kg IVIG was administered continuously with relief of fever for two days, after which fever and scleritis returned. Pulse therapy with methylprednisolone at a dose of 30 mg/kg for 3 days gave a positive effect with a decrease in the diameter of the coronary artery to 3 mm and normalization of hematological parameters. In the next 2 weeks, scleritis and low-grade fever up to 37.7°C periodically appeared, with further complete recovery;
- a 1-year-old girl with a picture of a retropharyngeal abscess (fever, pain with head movements, trismus) and a hypoechoic (20–30 U H) lens-shaped formation that does not accumulate contrast in the retropharyngeal region, identified by computed tomography. The absence of pus upon opening the site of edema on the posterior wall of the pharynx and the persistence of temperature, despite antibacterial therapy, helped to suspect KS. In addition, the mother was able to find out the presence of a one-day scleral injection and an ephemeral rash on the 1st–2nd day of illness. The introduction of IVIG stopped the fever, and on the 10th day peeling of the fingers appeared. We found a description of few similar observations in the literature [21].
Incomplete KS is more common in infants, so we, like foreign authors, recommend echocardiography for all children with unclear fever and laboratory markers of inflammation [10, 22].
A number of diseases with exanthema and joint changes have signs similar to KS (infections accompanied by exanthema, toxic shock and scalded skin syndromes, juvenile rheumatoid arthritis, Stevens-Johnson syndrome, etc.). Some of them are excluded based on clinical data, even if the duration of fever is less than 5 days (including the effect on the administration of an antibiotic).
With infectious mononucleosis, a maculopapular rash appears in 10–15% of cases, but the fever usually lasts less than a week, and laboratory data help in verifying the diagnosis. Stevens-Johnson syndrome differs from KS in the presence of bullous-erosive elements. Juvenile idiopathic arthritis often presents for several weeks with only fever, generalized lymphadenopathy, and a patchy, faint, floaty rash. This diagnosis, like polyarteritis nodosa, should be kept in mind in patients with suspected KS who have been treated with an adequate dose of IVIg without effect. We observed a similar picture in an infant, which, together with the indication of “possible changes in the walls of the coronary artery” on cardiac ultrasound, forced us to administer IVIG, which did not give the expected improvement; the child was subsequently diagnosed with juvenile idiopathic arthritis.
Therapy
Initial therapy for both complete and incomplete SC involves the administration of 2 g/kg IVIG and acetylsalicylic acid (as an anti-inflammatory and antiplatelet agent) at a dose of 80–100 mg/kg/day in 4 divided doses. Children with giant coronary aneurysms may require additional anticoagulants (warfarin, dipyridamole). In Japan, there is experience in treatment with lower doses of acetylsalicylic acid (30–50 mg/kg/day) to prevent hepatotoxic effects [23, 24]. Most children respond to IVIG administration by relieving fever and significantly improving their well-being within the first 24 hours, while the risk of vascular and cardiac damage and aneurysm formation is significantly reduced (from 20 to 5%). More than 2/3 of coronary aneurysms regress during the first year after the disease; there is insufficient data on the persistence of signs of residual coronary stenosis. If the child has a normal temperature for 4–5 days, the dose of aspirin can be reduced to 3–5 mg/kg once a day. Approximately 10–20% of patients treated with IVIG develop recurrent fever [7]. In this case, immunoglobulin is reintroduced in the same dose (2 g/kg); As a rule, this is enough and the fever stops. Only if repeated administration of IVIg is ineffective is the question of prescribing infliximab considered, although there is evidence of its effectiveness as a starting drug in the treatment of KS [25]. If two doses of IVIG or infliximab are ineffective, the effect of glucocorticosteroids is sometimes observed, but due to their negative effect on the condition of the coronary artery, such treatment is not recommended, at least until the results of multicenter controlled studies are available [26]. Patients are considered resistant to IVIg if a repeat dose had to be administered 2 days or more after the initial dose. Resistant KS, according to research, occurs in 16.3% of cases with a range between clinics of 8.0–26.8%. More often cases of resistance are registered among African Americans [27].
Due to the potential for inactivation of live vaccines following IVIG treatment, measles, mumps and rubella vaccination should be delayed for 11 months. There is also a risk of developing Reye's syndrome in children receiving acetylsalicylic acid for a long time, especially if they have influenza or chickenpox. In case of contact or illness of a child with these infections, temporary withdrawal of acetylsalicylic acid is possible, and for children with an aneurysm, dipyridamole can be prescribed for this time.
Forecast
KS is the leading cause of acquired heart disease in children, increasing the risk of developing coronary heart disease and myocardial infarction at a young age. Prognostically unfavorable factors for the development of coronary artery aneurysm include male gender, age under one year, prolonged fever, and relapse of KS. Thrombocytopenia, hypoalbuminemia, as well as low levels of hemoglobin and immunoglobulins G are predictors of severe KS with a possible outcome in the formation of a coronary artery aneurysm [2, 10].
In case of timely adequate treatment of KS, the mortality rate, for example, in the USA is less than 0.01%. A follow-up observation of 546 cases of KS showed that 5 of them were fatal. Of the causes of death, in one case there was damage to the coronary artery, in one - sudden death without signs of thrombosis or myocardial infarction, in another - acute coronary syndrome as a result of thrombosis of an aneurysm, in two - other variants of acute coronary syndrome. In 50% of cases, death occurred within a month after relief of the acute condition [28].
Approximately 2% of patients experience a recurrence of KS several months or even years after the first disease. Of the children we observed, one 6-month-old child had a relapse of KS 2 months after the first episode, treated in another hospital. The girl was admitted on the first day of fever with clear clinical manifestations of the disease and dilation of the coronary vessels. The fever resolved after the first dose of IVIG, with further regression of clinical symptoms and normalization of ultrasound changes.
Currently, many studies are devoted to studying the role of KS in the development of periodic febrile syndromes and some autoimmune diseases [29]. All children with KS we observed received treatment with IVIG; in 77% of cases, we achieved a lasting effect after a single dose of 2 g/kg in the form of normalization of temperature and significant improvement in condition.
In 23% (5 children) of cases, IVIg administration had to be repeated, which significantly increased the cost of treatment. The use of acetylsalicylic acid at a dose of 80–100 mg/kg/day in 4 doses did not cause side effects in our observations, as did its further long-term use at a low dose (3–5 mg/kg/day).
Conclusion
We observed 22 children with KS in both the earliest and late stages of the disease. All these children were hospitalized with one constant complaint - persistent fever, which did not stop until specific treatment was carried out. One of the main difficulties in diagnosing KS in the early stages of the disease before the appearance of signs of coronaritis was the absence of several characteristic symptoms, which in most patients nevertheless appeared at a later date. In addition, in some parents, upon close questioning, it was possible to find out the presence of some typical signs of the disease that appeared at the very beginning of the disease and disappeared before hospitalization.
Measures for timely diagnosis and adequate treatment of KS in accordance with international standards and recommendations include close attention to children with persistent fever, especially those that do not respond to antibiotics, structured questioning of parents about the presence of KS symptoms at the onset of the disease, and timely qualified ultrasound of the coronary artery. After discharge from the hospital, patients undergo long-term follow-up monitoring with ultrasound, monitoring of the heart and hematological parameters.
Symptoms of Kawasaki disease
The most striking symptom of Kawasaki disease syndrome in children (see photo) is fever that lasts longer than 5 days. Also observed with KS:
- increase in the size of the cervical lymph node;
- swelling of the tongue;
- acquisition of a scarlet hue by the tongue;
- redness of lips;
- cracks on the lips;
- rash of a polymorphic nature, localized on any part of the body;
About 2 weeks after the onset of the fever, your child may develop lumps with flaky skin on the palms of the hands or soles of the feet.
During the pathology, three stages are distinguished, cyclically replacing each other:
- The acute stage lasts two weeks and is manifested by fever, symptoms of asthenia and intoxication. An inflammatory process develops in the myocardium, it weakens and ceases to function.
- The subacute stage is manifested by thrombocytosis in the blood and symptoms of cardiac disorders - systolic murmur, muffled heart sounds, arrhythmia.
- Recovery occurs by the end of the second month of the disease: all symptoms of the pathology disappear and the general blood test indicators normalize.
Kawasaki syndrome in adults is characterized by inflammation of the coronary vessels, which cease to be elastic and swell in some areas. The disease leads to early atherosclerosis, calcification, thrombus formation, myocardial dystrophy and infarction. In young people, aneurysms become smaller over time and may disappear permanently.
Patients complain of heart pain, tachycardia, arthralgia, vomiting, and diarrhea. In more rare cases, symptoms of meningitis, cholecystitis and urethritis, cardiomegaly, and hepatomegaly are noted.
How is Kawasaki syndrome diagnosed?
Doctors make the diagnosis solely on the basis of the clinical picture. Thus, a diagnosis may be made if an unexplained high fever lasts five or more days along with four of the following five signs: bilateral conjunctivitis (inflammation of the membrane that covers the eyeball), swollen lymph nodes, skin rash, lesions of the mouth and tongue, and related changes in limb areas. But at the same time, the doctor must make sure that there are no signs of any other disease that may have the same symptoms.
If symptoms are detected, doctors conduct an ECG and echocardiography, the patient is prescribed testing to exclude other diseases (complete blood count, blood tests for ESR, C-reactive protein, antinuclear antibodies (ANA), rheumatoid factor (RF), albumin, liver enzymes, smear culture from the throat and blood culture, urinalysis, chest x-ray).
Diagnostics
To make a diagnosis of Kawasaki syndrome, fever must be present for more than 5 days and any 4 of the following criteria must be present:
- Erythema of the palms or soles;
- Dense swelling of the hands or feet on the 3-5th day of illness;
- Peeling on the fingertips in the 2-3rd week of the disease;
- Bilateral conjunctival injection;
- Changes on the lips or in the oral cavity: “strawberry” tongue, erythema or cracks on the lips, infection of the oral mucosa and pharynx;
- Any of the listed changes, localized on the extremities;
- Polymorphic exanthema on the body without blisters or crusts;
- Acute non-purulent cervical lymphadenopathy (diameter of one lymph node >1.5 cm).
If 2-3 of the 4 mandatory signs of the disease are absent, a diagnosis of an incomplete clinical picture of the disease is made.
What is Kawasaki syndrome?
Kawasaki syndrome is a mucocutaneous lymphonodular syndrome that manifests as necrotizing systemic lesions of medium and small arteries. The disease is characterized by fever, changes in the mucous membranes, skin, damage to the coronary and other visceral arteries with the possible formation of aneurysms, thrombosis and ruptures of the vascular wall.
Kawasaki syndrome affects the arteries and can cause serious heart complications. According to the medical reference, coronary artery damage occurs in approximately 20% of untreated patients.
The disease was first described in the English-language medical literature in 1967 by a Japanese pediatrician named Tomisaku Kawasaki . He identified a group of children with fever, skin rash, conjunctivitis, redness of the throat and mouth, swelling of the arms and legs, and enlarged lymph nodes in the neck. And a few years later, patients experienced heart complications, such as coronary artery aneurysms (expansion of the lumen of these blood vessels).
Fool Down, Asperger's. How much does it cost to identify a genetic disease? More details
Complications
Kawasaki disease has a very severe course and is often complicated by the development of serious disorders:
- Myocarditis,
- Acquired aortic and mitral insufficiency,
- Hemopericardium,
- Otitis media,
- Myocardial infarction,
- Aneurysm rupture
- Pericarditis,
- Valvulitis,
- Acute and chronic heart failure.
Timely diagnosis and treatment of Kawasaki syndrome have dramatically reduced morbidity and infant mortality.
Symptoms
The disease in question always begins acutely:
- body temperature rises, often to critical levels;
- cervical lymph nodes enlarge;
- I am worried about severe abdominal pain, nausea and frequent vomiting after eating.
The child categorically refuses to eat, cries constantly, and has trouble sleeping. In the first month, the symptoms of Kawasaki disease are aggravated by skin manifestations - rashes affect the lower and upper extremities and torso. Blisters quickly form and mature, then burst and heal, and in their place a red, dense surface forms - it is painful and causes a lot of inconvenience.
Complementing the clinical picture:
- redness of the mucous membrane of the eyes;
- severe dryness of the mouth and lips;
- crimson tongue color;
- conjunctivitis;
- swelling of the feet and hardening of their skin.
As the disease progresses, the child experiences severe shortness of breath after light physical exertion, fatigue and general weakness with increased drowsiness.
Treatment of Kawasaki disease
The main goal of drug therapy is to protect the cardiovascular system from damage.
The following drugs have a good effect on Kawasaki disease:
| Aspirin | has a powerful anti-inflammatory effect and promotes blood thinning, therefore it is widely used to treat Kawasaki disease. |
| Immunoglobulin | is administered intravenously once a day and allows the body to quickly cope with the disease by increasing passive immunity. |
| Anticoagulants | To prevent thrombosis, patients are prescribed anticoagulants, most often clopigel and warfarin. |
With the development of complications from the cardiovascular system (stenosis, aneurysms, myocardial infarction), children who have suffered the acute and subacute stages of Kawasaki disease may be prescribed angioplasty, coronary artery bypass grafting or stenting.
How does the infection progress?
Pathology has four forms of occurrence:
- Flu-like syndrome. Another name is Flu-Like. This pathology has the mildest form. Characteristic symptoms are fever, muscle pain, discomfort in the bones and general malaise. Signs of the disease are observed within three days. Next comes recovery. Influenza-like syndrome rarely causes complications, but only with qualified therapy;
- Intestinal infection. Children under two years of age most often suffer from this form of pathology. With such a disease, it is not necessary that other children will become infected from the child. In a group, this case may be exclusive and no one else may suffer from it. Characteristic symptoms are high fever, discomfort in the bones and general weakness of the body. In the first days of infection, other signs are observed - intestinal upset, nausea accompanied by vomiting. For this reason, the disease is often confused with poisoning. The period of exacerbation is 2-3 days for children of primary school age and a week for newborns. This disease can cause milk intolerance during the first time after recovery. This makes it necessary to give the child medical lactose before breastfeeding or to refuse it;
- Boston Pathology. The disease manifests itself in the same way as rubella, which makes it difficult to diagnose. A child, like an adult infected with the Coxsackie virus, in this case becomes covered with formations of a red hue. Symptoms: high fever, rashes on the epidermis in the form of blisters. The treatment period is 3-5 days. After this, recovery begins. With this form, relapse rarely occurs, and complications are most often not observed;
- Pleurodynia. Another name is Bronholm's disease. Symptoms: high fever, severe pain in the back, abdomen, muscles and chest. Spasms occur at regular intervals – once every 60 minutes. The duration of the attack is from 1 to 20 minutes. They cause spasms in the pleura and peritoneum, which cause pain during friction.
With any form of pathology, the patient needs urgent medical care.
Coxsackie viruses are divided into two large groups
There are two groups of pathology:
- Type A virus: Infection with the Coxsackie virus causes damage to the throat and may cause meningitis.
- Virus type B. Affects the brain, muscles and heart, causing irreversible changes in these internal organs.
Course options: mild, moderate and severe
Pathology has varying degrees of progression. The severity of the disease depends on how much the mucous membranes and internal organs are damaged. The degree is also affected by damage to the body by toxins.
The mild form of the pathology is characterized by a rapid course. Recovery occurs within a few days. In this case, the virus does not affect the patient’s internal organs and brain.
With moderate severity, therapy takes a little more than a week. The pathology has pronounced symptoms. The virus can affect internal organs, but with qualified treatment the problem can be quickly resolved.
The severe form of the disease is characterized by pronounced symptoms and a long course. This causes damage to the brain and internal organs.
Experts also identify the following variants of the pathology:
- smooth – recovery occurs quickly and the disease does not recur;
- wavy - the pathology either fades or flares up with renewed vigor;
- recurrent – after recovery, the disease develops again;
- with complications – the disease is difficult to treat and causes complications.
Forms of the disease
There are two forms of pathology:
- Isolated. The disease occurs in one syndrome.
- Combined. In this case, the Coxsackie virus affects several organs and systems at once.
Diagnostics: analysis for Coxsackie virus
Typically, infection is diagnosed by clinical symptoms. In rare cases, in severe cases, a test for the Coxsackie virus is prescribed. On average, it takes 2 weeks to get results, which is why such tests are not prescribed en masse. As a rule, the patient will recover faster than the test result. There are rapid tests with a 66–90% confidence level, but they are very difficult to obtain and do not work for all subtypes of the virus.
The doctor may prescribe a general blood test to assess the state of immunity and the severity of the inflammatory process. In some cases, biochemical blood tests may be additionally prescribed to check the functioning of internal organs. In children with symptoms of acute intestinal infection, rapid tests are sometimes performed to rule out other diseases. If a sore throat manifests itself, it is advisable to exclude a streptococcal infection, which will require the use of antibiotics.
If meningitis is suspected, a spinal tap is performed to rule out the bacterial nature of the disease. Ultrasound and ECG are used in the diagnosis of heart pathologies.
What is a hemorrhagic rash?
When the capillaries are damaged, some of the red blood cells come out of the vessel, which leads to the appearance of a rash with red spots - this is a hemorrhagic rash.
Initially, the rash is painless, but if you ignore the rash, it may become painful. When you press on the rash, its color does not change in any way, and the rash does not become smaller. This is the hallmark of hemorrhagic rashes.
Depending on the lesion that caused the rash, the types of rashes can be different - small dots, stripes or spots, the color of which can also be varied - blue, red, purple. The size of the spots may vary. In medical practice, medium-sized spots are usually called liver purpura, and small spots are called petechiae.
The most common area of localization of the rash is the lower extremities. If a hemorrhagic type rash develops, you should immediately consult a doctor, as this is a direct indication for hospitalization, even in the absence of other symptoms.
Features of hemorrhagic rash in children
A hemorrhagic rash in children usually accompanies hemorrhagic vasculitis, hemophilia, meningococcemia, and thrombocytopenic purpura. But hemorrhagic vasculitis is the most common disease, the manifestation of which is a rash.
As already mentioned, the most common manifestation of the rash occurs on the front surfaces of the legs. However, it can also be localized on the torso, buttocks, and thighs. The rash is located symmetrically, does not disappear when pressed and does not change its color. The disease usually affects children under six years of age.
In addition to hemorrhagic rashes, other types of rashes also occur in children. In the article on the website you can see a photo of a rash on a child’s body with explanations.