Let's imagine that you are a doctor or paramedic who has been called to provide emergency care. The patient has acute chest pain, shortness of breath, and nausea. Such events will resemble a heart attack, acute heart failure, cocaine abuse, indigestion, etc. [1] You will need to have an electrocardiogram done on site to see the approximate picture. You know that in the event of a heart attack, “time is saved heart muscle, and time spent is lost”! 2 Timely assistance can save the patient’s life and avoid possible consequences. [3] This is where a set of rapid troponin tests can come to the rescue. After pricking the patient's finger, apply a small amount of blood to the test strip. After a few minutes, a test line will appear that is highly likely to indicate a heart attack.
Figure 1 Cardiac troponin is a diagnostic marker for detecting heart attack. Such rapid tests help establish a quick diagnosis. The structural illustrations of the cardiac troponin complex in the figure are derived from the crystal structure of 1J1D deposited in the RCSB PDB. [4, 5]
Myocardial infarction
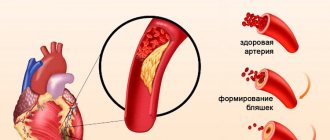
Myocardial infarction (heart attack or MI) is an acute condition that requires emergency medical attention.[1] Most heart attacks happen suddenly when one of the arteries leading to the heart becomes blocked, usually by a blood clot, cutting off blood flow. Lack of blood blocks the flow of oxygen and nutrients. Without them, heart cells begin to die. When it comes to treating a heart attack, every second counts. Extensive blockage, especially of a large blood vessel, can cause a severe heart attack. If heart disease is not treated early, it can lead to heart failure. Myocardial infarction is caused by a buildup of plaque made from fat and other substances that narrows or hardens the arteries.
Timely diagnosis is paramount for early treatment of MI
Irreversible cardiac damage resulting from coronary artery occlusion can be largely avoided with prompt reperfusion therapy. Reperfusion therapy includes the use of drugs and surgery. Medicines used to treat heart attacks dissolve the clot blocking the artery. Blood flow can be restored surgically by opening the artery at the site of the blockage (coronary angioplasty) or by grafting a new artery around the blockage (coronary artery bypass grafting).[6]
Early diagnosis of acute MI is critical in further treatment. Typical symptoms associated with MI—acute chest pain, often accompanied by upper body pain, shortness of breath, nausea, fatigue, and sweating—are not always observed in every case [7]. Thus, clinical assessment, even in combination with an electrocardiogram (ECG), is often insufficient to diagnose or exclude MI. A blood test to measure the concentration of cardiac troponin (cTn) is an important procedure for the early diagnosis of MI.
Cardiac troponins as diagnostic markers
Troponin is a regulatory protein complex responsible for the functioning of muscle cells. It consists of three subunits: troponin I, T and C (cTnI, cTnT and cTnC). [9] Cardiac muscle cells express cTnI and cTnT isoforms that are structurally different from their skeletal counterparts. In contrast, the cardiac and skeletal isoforms of troponin C are so similar that they are difficult to distinguish by standard diagnostic methods. Blood levels of cTnI and cTnT are usually very low. The death of cardiac muscle cells (myocardial necrosis) leads to the release of cTnI and cTnT into the bloodstream. After a heart attack, the concentration of cardiac troponin (cTnI) in peripheral blood increases 100-fold.
Immunoassays specific for cardiac troponin isoforms may show increased levels in peripheral blood independent of skeletal troponin levels. A number of immunoassays specific for cTnI or cTnT have been developed that meet the same characteristics and do not differ in terms of their diagnostic and prognostic value. cTn (I or T) is the preferred biomarker of myocardial necrosis due to its high-quality performance in the diagnosis and prognosis of cardiac conditions.[6]
Serial measurements of HF troponins
According to international recommendations, to diagnose NSTEMI, serial measurements of high-frequency troponins should be carried out, which should reflect: 1) the dynamics of increased Tn associated with an increase in the area of myonecrosis, or 2) in the absence of such, indicate chronic, non-ischemic elevated troponin.
A schematic diagram of the algorithm for serial measurements of HF troponins was recommended in 2012 by the European Society of Cardiology [5].
If upon admission the HF troponin was below or equal to the 99th percentile and after 3 hours the increase (delta) is more than 50% of the initial level, then a diagnosis of MI is made. If the picture is unclear, the measurement is repeated after another 3 hours.
If upon admission the HF troponin was above the 99th percentile, and after 3 hours the delta is more than 20% of the initial level, then a diagnosis of MI is made. If the picture is unclear, the measurement is repeated after another 3 hours (Fig. 3).
Rice. 3. Schematic diagram of the algorithm for serial RF measurements [5]
In order to increase the speed of diagnosis, HF test manufacturers are developing and offering their own faster serial measurement algorithms. It is important that the serial measurement algorithms for various RF tests are based on 99th percentile values and delta values that are strictly specific to these test systems, therefore such algorithms are not interchangeable: the serial measurement algorithm for the RF test from company A cannot be used for the RF test from company B and vice versa.
According to the European Society of Cardiology guidelines published in 2021 regarding the management of non-ST segment elevation ACS, “the use of a 0/3 hour HF troponin algorithm is recommended. Alternatively, the use of a 0/1 hour HF troponin measurement is recommended, if available.” corresponding RF measurement with a validated algorithm” [6].
The improvement of RF test systems today is proceeding very quickly. Regular updates on innovations in this industry can be very helpful. Information on accelerated RF measurement algorithms is provided by test system manufacturers and published in scientific journals.
Features of serial RF measurements during late admission
The degree of usefulness of HF troponins is related to the time elapsed from the onset of clinical symptoms of ischemia until the patient is admitted and the first measurement is made. With late admission, the dynamics of an increase in HF troponins may not manifest itself and serial measurements may show a plateau - high absolute concentrations of HF troponins and the absence of their increase (or decrease). In such cases, in late-presenting patients, the absence of an obvious delta does not exclude AMI.
Rapid tests help detect MI earlier than laboratory tests
This rapid test has many advantages for use in diagnosing MI: ease of use, reliability, instrument-free reading, and use of capillary blood taken from a finger prick. However, a key advantage is the ability of RDT to detect elevated cTnI earlier than laboratory testing in certain conditions. In the event of a myocardial infarction, early treatment is critical, which can help avoid extensive damage to the heart. Timely diagnosis is of paramount importance for early treatment of MI. RDT can be used whenever a result is needed before laboratory analysis.
Third universal (universal) definition of myocardial infarction
The high diagnostic efficiency of HF troponins led to the adoption of a new, third, universal definition of MI in 2012, which establishes that the diagnostic criteria for MI are “detection of an increase and/or decrease in the concentration of a cardiac marker (preferably cardiac troponin [cTn]) at least one value above the 99th percentile.” This means that HF tests must detect troponin concentrations below the 99th percentile, including in healthy individuals, and therefore the use of the terms troponin-positive and troponin-negative is not recommended [7].
In what cases is a rapid troponin test used?
Prehospital diagnostics
One of the advantages that makes it advisable to use a rapid test for the presence of troponin is that it gives a quicker result than a laboratory - this is the first contact of health workers with the patient. Peripheral blood cTnI levels begin to rise gradually several hours after myocardial infarction and typically peak at 24 to 48 hours, nearly 100 times the baseline level (Figure 2). Serious cases of myocardial infarction, or cases where several hours have passed between the onset of symptoms and contact with health care workers, can be identified at the scene or during transport to hospital. The patient can receive emergency medical treatment and upon arrival at the hospital, the correct treatment will be selected through cardiac imaging and coronary angioplasty.
Figure 2 Concentrations of cardiac troponin (cTnI) in peripheral blood increase 100-fold after a heart attack. The cutoff value of this test for diagnosing elevated cTnI is about 0.5 ng/ml. Figure from Mahajan and Jarolin, Circulation, 2011.[11].
It can take several hours for a patient's blood sample to arrive at the central laboratory. In addition, the in vitro cTnI test is associated with a long turnaround time. In contrast, the cTnI test with RDT can be performed on site and the result is known almost instantly. If the result is positive, the patient can be treated immediately.
Crowded emergency room
Overcrowding in hospital emergency departments (ED) is a widely recognized problem that has been shown to lead to increased inpatient mortality.[12] Guidelines from leading heart associations indicate that cTn results should be available to clinicians within 60 minutes of arrival in the emergency department. [13,8] Contrary to these recommendations, even in developed countries, the time from blood collection in the emergency department to receiving the troponin test result is one to two hours. [14] Overcrowding in departments often results in sample processing failures and increases laboratory turnaround times.[15] The cTn test using RDT cTnI can be easily performed by a nurse independently of a central laboratory. By detecting elevated cTnI in a timely manner, RDT can quickly provide important information for medical triage of patients. This can reduce the delay in patient treatment and also reduce the overall workload on the department.
brief information
Rapid tests for the determination of cTnI are easy to use and read the result, reliable, compatible with capillary blood and, above all, give quick results. These features make them ideal for diagnosing myocardial infarction in the prehospital setting. These tests assist in triage in emergency departments. However, the diagnosis of acute myocardial infarction should not be based solely on the results of a rapid test, but should also include the patient's symptoms, ECG and/or angiographic findings. Tests can confirm acute MI, but not rule it out. A negative result on this test with serial blood draws ranging from several hours to several days after the onset of symptoms may indicate a mild form of myocardial infarction or other heart disease.
Figure 3.
Point-of-care versus central laboratory testing for cardiac troponin in patients with suspected heart attack. Point-of-care testing may rule out myocardial infarction earlier than laboratory testing. [16]
References 1. OJ Mechanic and S.A. Grossman, Myocardial Infarction, Acute, StatPearls Publishing, 2021. 2. E. Braunwald, Evolution of the management of acute myocardial infarction: A 20th century saga, vol. 352, Elsevier Limited, 1998, pp. 1771-1774. 3. „Heart attack - your quick guide | BHF,” [Online]. Available: https://www.bhf.org.uk/informationsupport/publications/heart-conditions/heart-attack—your-quick-guide. 4. S. Takeda, A. Yamashita, K. Maeda and Y. Maéda, “Structure of the core domain of human cardiac troponin in the Ca2+-saturated form,” Nature, vol. 424, no. 6944, pp. 35-41, 3 7 2003. 5. “RCSB PDB - 1J1D: Crystal structure of the 46kDa domain of human cardiac troponin in the Ca2+ saturated form,” [Online]. Available: https://www.rcsb.org/structure/1j1d. 6. K. Thygesen, J. S. Alpert, A. S. Jaffe, B. R. Chaitman, J. J. Bax, D. A. Morrow and H. D. White, “Fourth Universal Definition of Myocardial Infarction (2018), “ Journal of the American College of Cardiology, vol. 72, no. 18, pp. 2231-2264, 30 10 2021. 7. R. Twerenbold, J. Boeddinghaus, T. Nestelberger, K. Wildi, M. Rubini Gimenez, P. Badertscher and C. Mueller, Clinical Use of High-Sensitivity Cardiac Troponin in Patients With Suspected Myocardial Infarction, vol. 70, Elsevier USA, 2021, pp. 996-1012. 8. M. Roffi, C. Patrono, J.-P. Collet, C. Mueller, M. Valgimigli, F. Andreotti, J. J. Bax, M. A. Borger, C. Brotons, D. P. Chew, B. Gencer, G. Hasenfuss, K. Kjeldsen and P. Lancellotti, „2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation,” European Heart Journal, vol. 37, no. 3, p. 267–315, 2021. 9. “Troponin - StatPearls - NCBI Bookshelf,” [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK507805/. 10. F. S. Apple, Y. Sandoval, A. S. Jaffe and J. Ordonez-Llanos, “Cardiac Troponin Assays: A Guide to Understanding Analytical Characteristics and Their Impact on Clinical Care,” Clinical Chemistry, vol. 63, no. 1, pp. 73-81, 1 1 2021. 11. V. S. Mahajan and P. Jarolim, “How to interpret elevated cardiac troponin levels,” Circulation, vol. 124, no. 21, pp. 2350-2354, 22 11 2011. 12. B. C. Sun, R. Y. Hsia, R. E. Weiss, D. Zingmond, L. J. Liang, W. Han, H. McCreath and S. M. Asch, “Effect of emergency department crowding on outcomes of admitted patients,” Annals of Emergency Medicine, vol. 61, no. 6, p. 605, 2013. 13. A.H.B. Wu, R.H. Christenson, D.N. Greene, A.S. Jaffe, P.A. Kavsak, J. Ordonez-Llanos and F.S. Apple, “Clinical Laboratory Practice Recommendations for the Use of Cardiac Troponin in Acute Coronary Syndrome,” Clinical Chemistry, vol. 64, no. 4, pp. 645-655, 1 4 2021. 14. C. Ho, K. Cimon, L. Weeks, M. Mierzwinski-Urban, L. Dunfield, L. Soril, F. Clement and M. Jabr, “Point-of-Care Troponin Testing in Patients With Symptoms Suggestive of Acute Coronary Syndrome: A Health Technology Assessment Economic authors: “A Health Technology Assessment, vol. 5, no. 1b, 2021. 15. K. D. Rooney and M. M. Schilling, “Point-of-care testing in the overcrowded emergency department—Can it make a difference?,” Critical Care, vol. 18, no. 1, p. 692, 8 12 2014. 16. A. R. Chapman, S. Stewart and N. L. Mills, Contemporary point of care cardiac troponin testing in suspected acute coronary syndrome, vol. 105, BMJ Publishing Group, 2021, pp. 740-741.
Ischemic and non-ischemic increase in HF troponins
Numerous studies have shown that a large proportion of patients admitted with suspected ACS have non-ischemic (chronically) elevated levels of high-frequency troponins not associated with ACS. The most common conditions associated with ischemic (acute) and non-ischemic (chronic) increases in troponins are presented in Fig. 2.
Rice. 2. Main types of ischemic and non-ischemic elevation of troponins
Current understanding is that non-ischemic elevated troponin is an early marker of subclinical structural myocardial damage associated with non-calcified plaques with a thin fibroatheromatous cap.
To discriminate between ischemic and non-ischemic increases in HF troponins, serial measurements should be taken: on admission and after 1-3 hours.
Indications for measuring HF troponins
- The highest priority is for the diagnosis of MI when symptoms suggest ischemia on a nondiagnostic ECG.
- Upon admission with signs of acute heart failure to quickly confirm or exclude type I MI; In AHF, troponin elevations above the 99th percentile are associated with a high risk of adverse outcome.
Important information. When ordering measurements of HF troponins, the clinician should assess in advance the likelihood of their increase based on: 1) the interval between the onset of ischemic symptoms and the time of patient admission; 2) the patient has pathologies associated with non-ischemic increases in troponins (chronic heart failure, renal failure, etc.).
3. When the purpose of RF measurements may be justified.
A. The appropriateness of HF measurement should be considered in patients without chest pain when ACS is suspected and one of the following symptoms is present:
- sudden onset of isolated shortness of breath,
- profuse sweating,
- interruptions in heart function,
- nausea, vomiting,
- severe weakness
- acute confusion,
- syncope.
B. If the symptoms indicated in paragraph A are present, HF measurement is prescribed under the following conditions:
- previous stroke,
- previous heart failure,
- diabetes,
- age over 75 years,
- female.